What is Myeloproliferative Neoplasms (MPNs)?
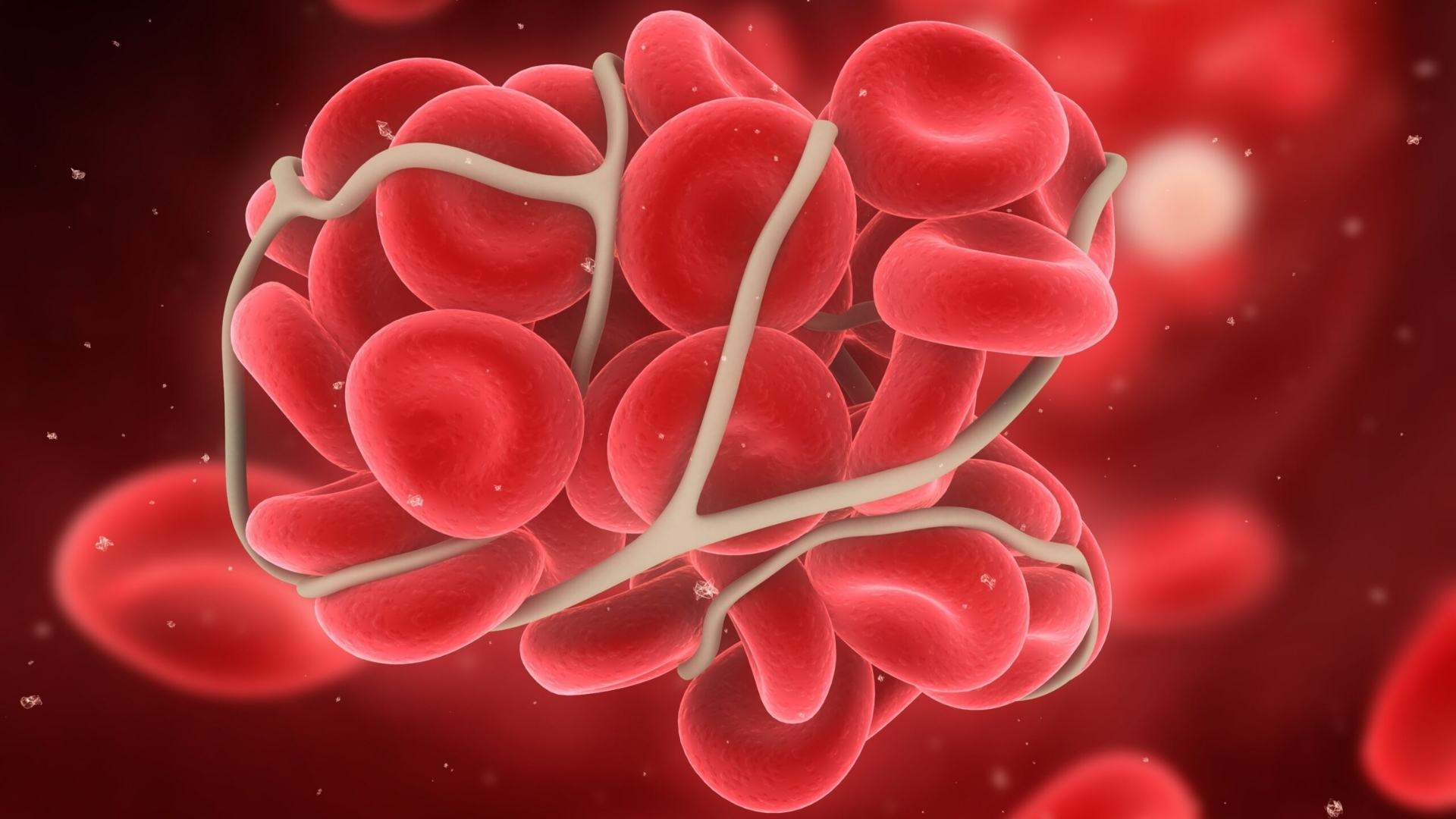
Myeloproliferative Neoplasms (MPNs) refer to a group of blood cancers characterized by excessive production of blood cells within the bone marrow. These disorders affect essential cell lineages, including white cells, red cells, and platelets, disrupting normal blood balance and function. At its core, an MPN results from genetic mutations that lead to uncontrolled cell proliferation.
Within the cancer biology field, understanding Myeloproliferative Neoplasms (MPNs) has evolved significantly, focusing on cellular metabolism abnormalities. A hallmark of many cancers, including MPNs, is the Warburg effect—a metabolic phenomenon whereby cancer cells consume glucose up to 200 times faster than healthy cells. This excessive glucose consumption provides rapid energy, fueling rapid and uncontrolled growth of cancer cells.
Biological Basis Behind Myeloproliferative Neoplasms (MPNs)
MPNs arise from mutations that primarily affect hematopoietic stem cells in the bone marrow. Several identified genetic mutations, notably JAK2, CALR, and MPL, contribute significantly to MPN pathogenesis. Among these, the JAK2 V617F mutation is the most common, found in approximately 50-60% of patients with essential thrombocythemia (ET) and primary myelofibrosis (PMF), and in more than 90% of polycythemia vera (PV) cases. These mutations activate signaling pathways promoting blood cell proliferation, erythrocytosis, and thrombocytosis, triggering disease development and progression.
Furthermore, cancer cells, including those in MPNs, exhibit specialized metabolic vulnerabilities beyond the Warburg effect. They rely heavily on glutamine metabolism, essential for generating numerous building blocks (like nucleotides and amino acids) required in rapid cell replication. This dependency presents innovative opportunities for targeted metabolic therapies, transforming cancer management possibilities.
Prevalence and Impact of Myeloproliferative Neoplasms (MPNs), particularly in Hong Kong and Asia
Globally, MPNs are relatively rare, yet their incidence is incrementing, primarily due to better diagnostic methods and aging populations. Annually, approximately 2.5-3 cases of MPNs per 100,000 individuals are diagnosed worldwide, translating to thousands of cases each year. In Asia and notably Hong Kong, MPN cases show steady trends, largely aligning with global rates, and primarily affecting older adults aged 50 years or above. Certain subtypes, like essential thrombocythemia and primary myelofibrosis, show further elevated incidence in older Asian demographics, highlighting a critical need within regional medical strategies.
- The median age of MPN diagnosis is approximately 60-65 years.
- While men and women both face MPN risks, essential thrombocythemia slightly skews towards female patients.
- In Hong Kong, exposure to specific environmental factors like pollution, lifestyle influences, and dietary habits might intersect creating slightly variable local epidemiology compared to Western populations.
Understanding Myeloproliferative Neoplasms (MPNs) from a broader epidemiological viewpoint helps medical experts tailor specific screening and management programs, optimizing patient prognosis and quality of life.
Physical and Emotional Impact of Myeloproliferative Neoplasms (MPNs)
Living with MPNs often means managing complex physical symptoms such as fatigue, splenomegaly (enlarged spleen), weight loss, night sweats, and bone pain. These symptoms significantly impair quality of life, daily functioning, and overall wellness. Concurrently, emotional stress from a cancer diagnosis can profoundly affect patients, instigating anxiety, depression, and feelings of isolation.
At AllCancer, we understand that comprehensive treatment involves addressing psychosocial dimensions, not just physical symptoms. Our approach ensures personalized, compassionate care to enhance coping strategies and patient empowerment, creating positive health trajectories.
Causes and Risk Factors of Myeloproliferative Neoplasms (MPNs)
Genetic Risk Factors
Several genetic mutations predispose individuals to MPNs. The JAK2 mutation is most prevalent, but mutations in CALR and MPL genes also appear frequently. These genetic abnormalities trigger aberrant activation of the JAK-STAT signaling pathways, leading to uncontrolled blood cell growth. Early identification of these mutations improves patient monitoring and treatment approaches significantly.
- JAK2 V617F mutation prevalent in Polycythemia Vera (>95% occurrence).
- CALR mutations found predominantly in Essential Thrombocythemia and Primary Myelofibrosis patients without JAK2 mutations.
- MPL mutations relatively rarer but significant for diagnostic differentiation and treatment decisions.
Environmental and Lifestyle Factors
Though largely genetically driven, environmental and lifestyle factors might contribute indirectly to MPN risks through cumulative exposure to various stressors:
- Exposure to radiation and chemical toxins such as benzene increases susceptibility to hematological malignancies, potentially impacting MPN risks.
- Long-term smoking and excessive alcohol consumption may amplify molecular and cellular damages, indirectly promoting MPN pathology and progression.
- Lifestyle influences like obesity, diet changes, and chronic inflammation have shown correlations with general cancer risk, implicating potential links with MPN cases requiring deeper regional studies.
Metabolic Vulnerabilities and Emerging Strategies for Prevention
Cancer cells possess unique metabolic vulnerabilities. They heavily depend on glucose and glutamine metabolism, significantly more than normal cells. Glucose fuels rapid cell proliferation (Warburg effect), and glutamine provides essential nutrients for nucleotide synthesis required by rapidly dividing malignant cells.
Emerging studies suggest targeted dietary adjustments and precise metabolic interventions may proactively address cellular metabolism vulnerabilities, thereby slowing or controlling disease progression.
Hong Kong and Asian-specific Risks and Prevention Initiatives
Given the unique epidemiological profile in Hong Kong, public education promoting early symptom recognition and routine health checks can dramatically improve early MPN detection. Personalized screening programs and genetic counseling services facilitate risk identification and preemptive strategies, significantly reducing burdens associated with advanced-stage diagnoses.
At AllCancer, we continually emphasize preventive education and early detection approaches for MPN management, aiming to reinforce health resilience, increasing treatment effectiveness and patient empowerment across Hong Kong and Asia.
Symptoms of Myeloproliferative Neoplasms (MPNs)
By understanding early signs and characteristic symptoms of Myeloproliferative Neoplasms (MPNs), patients in Hong Kong and across Asia can seek timely medical evaluation, significantly improving prognosis and life expectancy. Symptoms reflect underlying cancer biology, influencing diagnostic and therapeutic decisions.
Common Symptoms Across All Types of Myeloproliferative Neoplasms (MPNs)
- Fatigue and generalized weakness (due to anemia and altered metabolism)
- Unexplained weight loss despite normal appetite
- Night sweats unrelated to room temperature
- Persistent low-grade fever or recurrent infections
- Bone pain, typically affecting the ribs and the lower back region
- Splenomegaly (enlarged spleen), causing abdominal discomfort or fullness
- Easy bruising or bleeding due to alterations in platelet counts
- Headaches, dizziness, or visual disturbances from restricted blood flow
- Itching, particularly after a warm shower or bath due to cytokine release
Symptom Variations by Specific MPN Subtypes
Polycythemia Vera (PV)
- Facial flushing and redness due to increased red blood cell production
- Erythromelalgia, a burning pain in the hands or feet accompanied by redness and warmth
- High blood pressure, headaches, and tinnitus (ringing in the ears)
- Increased risk of thrombosis (blood clots) particularly in cerebral or coronary arteries
Essential Thrombocythemia (ET)
- Increased platelet counts leading to abnormal blood clotting tendencies
- Numbness or tingling sensations in the extremities due to impaired blood flow
- Difficulty concentrating, fatigue, and slight cognitive impairment
Myelofibrosis (MF)
- Severe splenomegaly, causing noticeable abdominal enlargement and significant discomfort
- Anemia causing persistent fatigue, shortness of breath, and pallor
- Intractable bone and joint pain due to marrow fibrosis
- Marked weight loss and cachexia (severe muscle wasting)
Early medical evaluation at the onset of even mild symptoms can greatly improve outcomes, particularly given the current therapeutic innovations present in Asia and Hong Kong, including advanced metabolic therapies targeting the metabolic vulnerabilities specific to MPNs.
Stages of Myeloproliferative Neoplasms (MPNs) and Survival Rates
Stage 1 – Myeloproliferative Neoplasms (MPNs)
Early-stage Myeloproliferative Neoplasms present as mild abnormalities in blood cell counts, with minimal symptoms often detectable only through routine screening or a health check-up. The disease remains localized mainly to the bone marrow and the bloodstream without notable organ involvement.
- Treatment options include vigilant monitoring (“watchful waiting”), targeted metabolic therapies, and supportive care.
- Survival rates for stage 1 MPN patients exceed 90% at 5 years, provided timely intervention is employed.
Stage 2 – Myeloproliferative Neoplasms (MPNs)
During stage 2 of Myeloproliferative Neoplasms, disease progression manifests in more pronounced symptoms and increasing abnormalities in blood counts, occasionally involving minimally enlarged spleen or liver.
- Treatment escalates to incorporate targeted metabolic drugs, advanced biological agents, and precise symptom management strategies.
- The recorded five-year survival rate at this stage ranges from approximately 75% to 85%.
Stage 3 – Myeloproliferative Neoplasms (MPNs)
At stage 3, Myeloproliferative Neoplasms exhibit clear regional spread marked by substantial enlargement of the spleen or liver and notable bone marrow fibrosis. Physical symptoms become considerably more impactful on daily activities.
- Treatments involve multi-modal approaches, including targeted therapies, immunomodulators, potential surgical management to alleviate symptomatic splenomegaly, and comprehensive supportive care.
- The survival rate for stage 3 patients in Hong Kong and Asian populations typically ranges between 50% to 70% at five years, influenced by rapid and effective therapy implementation.
Stage 4 – Myeloproliferative Neoplasms (MPNs)
Stage 4 Myeloproliferative Neoplasms characterize advanced disease, manifesting significant extramedullary hematopoiesis and systemic impact. It often entails transformation into acute leukemia in late-stage cases, posing significant therapeutic challenges.
- Treatment predominantly prioritizes systemic approaches, including cutting-edge targeted therapies and cellular therapies, managing quality of life, and applying the latest metabolic-based treatments intended to control disease progression.
- Stage 4 patients exhibit reduced survival rates in Asia, with typical figures averaging between 20% to 40% over three-to-five-year periods. However, advancements in personalized metabolic oncology strategies increasingly enable chronic management of Myeloproliferative Neoplasms even at advanced stages.
Highlighting the potential for chronic management through innovative treatments such as AllCancer’s globally patented 4D Therapy, patients even at advanced stages have improved outpatient care experiences. Ongoing research and innovative collaborations, particularly through partnerships in Hong Kong and Shenzhen Qianhai Taikang, aim to sustainably transform Myeloproliferative Neoplasms into chronic manageable conditions rather than terminal diagnoses.
Treatment Options for Myeloproliferative Neoplasms (MPNs)
Effectively managing Myeloproliferative Neoplasms (MPNs) involves a strategic multifaceted approach customized to individual patient needs. Standard therapies include pharmacologic treatments, targeted therapies, and emerging metabolic strategies, each tailored to optimize patient outcomes while mitigating adverse effects.
Standard Pharmacological Treatments
Currently, pharmacological therapies are frontline treatments for MPN. Common medications include:
- Hydroxyurea (HU): Widely used to reduce elevated blood counts and prevent vascular thrombosis in patients with polycythemia vera (PV) or essential thrombocythemia (ET).
- Interferon-alpha: Immunomodulatory effects beneficial especially for younger patients because it avoids leukemia-inducing risks of other agents.
- Anagrelide: Primarily employed in ET for platelet reduction, often in combination or alternatively to Hydroxyurea.
Pharmacological therapies aim at symptom relief, disease stabilization, and prevention of complications such as thrombosis or bleeding episodes. They provide significant benefits but require meticulous monitoring to balance efficacy and potential side effects in Asian patient populations, who may vary in pharmacodynamics and pharmacokinetics.
Targeted Therapies for MPNs
Understanding the genetic underpinnings of MPNs has catalyzed the development of powerful targeted therapies. Primary among these are:
- JAK inhibitors (e.g., Ruxolitinib, Fedratinib): Specifically counteract the pathogenic JAK-STAT signaling pathway, abnormally activated in MPNs. They improve symptoms, spleen size reduction, and significantly enhance quality of life for patients, particularly those with myelofibrosis. Advanced-generation inhibitors are demonstrating further promise.
- BCL-2 inhibitors (e.g., Venetoclax): Demonstrating potential in combination treatments for advanced myelofibrosis, particularly in patients showing resistance to traditional therapy.
In Hong Kong and across Asia, specialized genetic testing platforms at leading oncology centers help identify the precise mutations involved, strongly enhancing patient-specific treatment efficacy.
Metabolic Therapies: A Promising Frontier
Recent research underscores metabolic reprogramming as a hallmark of malignant cell proliferation in MPNs, characterized particularly by the Warburg Effect. Cancer cells preferentially utilize glucose and glutamine, which has triggered therapeutic interest focused on metabolic vulnerabilities:
- Glucose transport inhibitors targeting GLUT1/3: Cutting off the excessive glucose supply cancer cells need at roughly 200 times normal rates, drastically reducing proliferation.
- Targeting glutamine metabolism: Inhibiting glutaminase enzymes that cancer cells heavily rely upon, thwarting key energy and biosynthetic pathways in tumor development.
Institutions like Shenzhen Qianhai Taikang and partnerships with MD Anderson are significantly advancing these metabolic therapeutic innovations, adding a groundbreaking dimension to the treatment landscapes in Asia.
Personalized Treatment: A Necessity, Not an Option
Patient-specific treatment strategies informed by tumor biology and patient health status represent the state-of-art approach recommended by global guidelines. Genetic profiling combined with metabolic analysis empowers clinicians to formulate precisely targeted treatments. Early clinical trials reveal that personalized therapies improve response rates substantially, enhancing both survival outcomes and quality of life among MPN patients.
Limitations of Traditional Therapies for Myeloproliferative Neoplasms (MPNs)
High Toxicity and Side Effects of Conventional Treatments
Despite their widespread use, traditional therapies for MPNs have significant limitations. Chemotherapeutic agents like Hydroxyurea, although beneficial, present notable adverse effects including:
- Hematological toxicity: High (approximately 78%) risk of bone marrow suppression potentially causing severe anemia, leukopenia, and thrombocytopenia.
- Infective complications: A substantial increase in susceptibility to infections significantly impacting patient management and hospital admission rates.
- Cardiac toxicities and gastrointestinal distress: Documented occurrence reaching nearly 23%, impacting patient survival and treatment compliance.
These profound side effects necessitate careful patient monitoring and frequently influence long-term treatment adherence among patients in Asian regions with limited healthcare infrastructure for management of complex treatment toxicities.
Reduced Efficacy in Progressive Disease Stages
Conventional therapies typically exhibit substantially diminished effectiveness in advanced stages of MPNs, particularly myelofibrosis or leukemic transformation where response rates plummet below 21%. Traditional treatment regimens face resistance mechanisms, rendering them insufficient for patients in advanced disease phases, thus creating urgent demand for novel treatments effective even in late stages.
Emergence of Treatment Resistance Mechanisms
Cancer cells often adapt to conventional treatments, developing resistance pathways that significantly limit long-term therapeutic effectiveness. Specific genetic and metabolic changes characterize MPN resistance, such as:
- Enhanced DNA repair mechanisms: Over 400% increased activity observed in enzymes responsible for repairing DNA damage, posing critical challenges to chemotherapy and radiation effectiveness.
- Metabolic plasticity and nutrient adaptation: Tumor cells rapidly adapt metabolic pathways, limiting the sustained efficacy of single-agent treatments, increasing tumor survival, and promoting disease progression.
In densely populated regions like Hong Kong, these resistance mechanisms exacerbate treatment limitations, underscoring the necessity to design versatile, metabolically-driven, and mutation-informed treatment combinations.
Secondary Malignancies and Long-term Risks
Long-term use of conventional treatments is associated with an approximately 300% increased risk of secondary malignancies, such as acute leukemia, underscoring significant limitations in prolonged chemotherapy usage. Furthermore, radiation therapy, while beneficial, introduces complications including secondary cancers, tissue fibrosis, and impaired organ functioning—all potentially reducing patient quality of life and survival rates.
Need for Innovative Treatments
Given the complexity and challenges identified with traditional therapies, there remains an urgent global and particularly regional need for innovative, personalized therapies. Collaborative partnerships and advancements in metabolic oncology promise groundbreaking transformations in MPN treatment capabilities—propelling Asia towards improved patient outcomes and cancer becoming a chronic, controllable disease.