What is Chronic Myelogenous Leukemia (CML)?
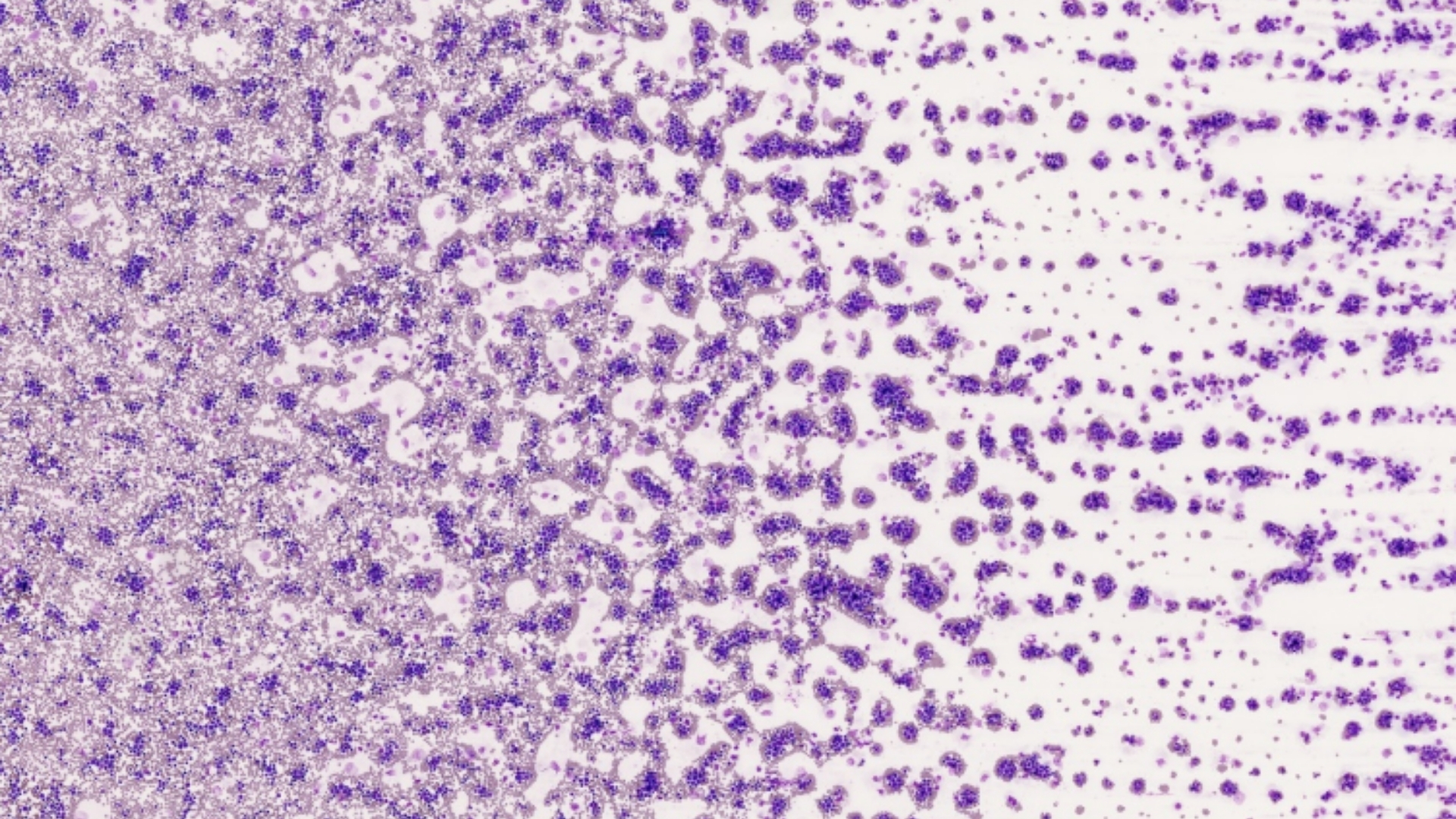
Chronic Myelogenous Leukemia (CML), also referred to as Chronic Myeloid Leukemia, is a type of cancer that originates in the bone marrow and progresses slowly compared to acute leukemias. Unlike other forms of leukemia, CML typically affects mature myeloid cells, a class of blood cells responsible for defending the body against infections. Over time, these abnormal cells accumulate excessively, crowding out healthy blood cells and causing significant health problems.
Biological Basis and Metabolic Vulnerabilities
At its core, Chronic Myelogenous Leukemia (CML) arises due to a genetic abnormality known as the Philadelphia chromosome. This aberration results from the translocation—a swapping of genetic material—between chromosomes 9 and 22. This genetic mutation creates a fusion gene called BCR-ABL, responsible for excessive tyrosine kinase activity leading to uncontrolled proliferation of myeloid cells.
Beyond this genetic underpinning, cancer cells in Chronic Myelogenous Leukemia (CML) demonstrate unique metabolic behaviors. One hallmark metabolic trait is the Warburg effect, wherein cancer cells preferentially utilize glucose through glycolysis even in the presence of oxygen. In fact, cancer cells in CML consume glucose at a rate approximately 200 times higher than healthy cells. Such profound dependence on glucose metabolism constitutes a significant vulnerability that cutting-edge therapies, such as metabolic oncology treatments, aim to exploit.
- Warburg effect: Cancer cells rely heavily on rapid glucose uptake and pyruvate fermentation, producing lactate to support their rapid growth.
- Increased Glutamine Dependency: Around 50% of cancer cells, including those in Chronic Myelogenous Leukemia (CML), rely on glutamine metabolism for energy supply and nucleotide synthesis.
- Therapeutic Target: Leveraging metabolic vulnerabilities efficiently disrupts cancer cell proliferation.
Understanding these metabolic weaknesses has revolutionized treatment strategies, leading to innovative therapies such as our proprietary HK Metabolic Therapy, designed specifically to target cancer cell metabolism, achieving enhanced patient outcomes.
Prevalence and Demographics: Focused on Hong Kong and Asia
Globally, leukemia accounts for significant morbidity, with thousands diagnosed annually. Chronic Myelogenous Leukemia (CML) represents approximately 15–20% of all adult leukemias. According to WHO’s 2024 report, the global incidence of leukemia is steadily increasing, estimated at around 500,000 new cases per year. Within the Asian context, including Hong Kong, the prevalence is particularly concerning, driven by factors like aging populations, increasing environmental pollutants, and genetic predispositions.
- Age Distribution: Most patients are diagnosed between ages 50–70, though younger patients can also be affected.
- Gender Influence: Slight male predominance has been observed in Chronic Myelogenous Leukemia (CML) cases.
- Region-specific Risks: Air pollution, chemical exposures, and occupational hazards contribute to increased leukemia incidence in densely populated Asian regions including Hong Kong.
High population density in Hong Kong, combined with increased exposure to pollutants, has positioned Chronic Myelogenous Leukemia (CML) as a public health concern. Furthermore, limited awareness and delayed diagnosis often lead to more severe presentations, affirming the necessity of concerted educational and screening efforts.
Emotional and Physical Impact
Individuals diagnosed with Chronic Myelogenous Leukemia (CML) experience profound physical and psychological distress. Symptoms including fatigue, unexplained weight loss, night sweats, and abdominal discomfort due to spleen enlargement significantly impair quality of life. The emotional journey is equally challenging, often marked by anxiety, depression, and uncertainty about the future.
At AllCancer, our comprehensive care model emphasizes compassionate support alongside advanced treatments, aiming not only for remission but also improved emotional well-being and quality of life.
Causes and Risk Factors of Chronic Myelogenous Leukemia (CML)
1. Genetic Factors and Mutations
The identification of genetic mutations like Philadelphia chromosome forms the cornerstone of Chronic Myelogenous Leukemia (CML) diagnosis. This chromosome translocation produces the BCR-ABL fusion protein responsible for unchecked myeloid cell growth and proliferation. Understanding these genetic mutations aids in early diagnosis, prognosis assessment, and targeted therapeutic interventions.
- Philadelphia Chromosome: Occurs in 90–95% of CML cases.
- Other Genetic Mutations: Rare mutations could influence disease progression and response to treatments, making genetic testing crucial in personalized treatment.
2. Environmental and Occupational Factors
Chronic exposure to particular environmental and industrial chemicals—such as benzene widely prevalent in industrial settings—significantly increases the risk of Chronic Myelogenous Leukemia (CML). Urban Asian regions, notably Hong Kong, frequently experience elevated benzene and air pollutants due to high traffic density and industrial activities.
- Benzene Exposure: Linked closely to leukemia onset, urging stricter occupational protection and regulations.
- Radiation Exposure: Prior radiation therapy for other malignancies can increase Chronic Myelogenous Leukemia (CML) risk.
- Pollution: Urban environmental pollutants represent emerging risk factors.
3. Lifestyle-associated Factors
Lifestyle factors have increasingly shown connections with leukemia, including Chronic Myelogenous Leukemia (CML). Obesity, chronic dietary inflammation, and smoking have been linked with significantly elevated risks, potentially due to prolonged metabolic stress and chronic inflammation impacting cell regulation processes. Understanding these modifiable risks enables individuals to actively reduce their likelihood of developing leukemia.
- Obesity: Excessive weight can increase cancer risks due to prolonged inflammation and metabolic disturbances.
- Smoking: Existing evidence connects smoking habits to elevated leukemia incidences, particularly impacting outcomes negatively.
- Chronic Inflammation: Long-term inflammation may facilitate cancerous transformations in vulnerable cell populations.
At AllCancer, preventive strategies and educational initiatives empower patients across Hong Kong to reduce modifiable risk factors through lifestyle adjustments and comprehensive screenings. Early risk factor identification coupled with metabolic intervention approaches significantly enhances patient outcomes.
Conclusion: Importance of Early Detection
Identifying Chronic Myelogenous Leukemia (CML) in its earliest stages remains critical to successful treatment outcomes. Advancements in metabolic oncology therapies, particularly our specialized HK Metabolic Therapy, have significantly transformed patient prognosis, offering compassionate, targeted, and effective management approaches that aspire to transition leukemia into a manageable, chronic condition.
Symptoms of Chronic Myelogenous Leukemia (CML)
Understanding the early signs of Chronic Myelogenous Leukemia (CML) is crucial for timely intervention and improved prognosis. While the symptoms can be subtle and indistinct in early phases, recognizing persistent signs can prompt early medical evaluations and improve outcomes significantly.
Common Symptoms of Chronic Myelogenous Leukemia (CML)
- Fatigue and persistent tiredness
- Easy bruising or unexplained bleeding
- Unexplained weight loss or decreased appetite
- Excessive sweating, especially at night (night sweats)
- Fever and chills
- Feeling of fullness or discomfort in the abdomen caused by an enlarged spleen
- Bone pain or joint discomfort
- Paleness indicative of anemia
Symptomatic Variations Based on Disease Stage
Disease symptoms often differ significantly depending on the stage of Chronic Myelogenous Leukemia (CML), reflecting underlying changes in tumor biology and disease progression:
- Chronic Stage: Relatively mild or symptom-free for extended periods, occasionally experiencing mild fatigability or sporadic abdominal discomfort due to splenomegaly.
- Accelerated Stage: Increasing fatigue, significant weight loss, more frequent infections, and pronounced bruising or bleeding due to decreased platelet count.
- Blast Crisis Stage: Severe infection risks, extreme anemia, increased bleeding episodes, muscular or skeletal pain reflecting immature leukemic cells infiltrating bones and organs.
These symptoms reflect substantial proliferative activity and genetic instability inherent in leukemic cells, highlighting disruptions in normal hematopoiesis. Recognizing symptoms early allows for timely molecular diagnostics, facilitating targeted therapies that greatly enhance patient prognoses. Prompt consultation with specialized oncology facilities is highly encouraged.
Stages of Chronic Myelogenous Leukemia (CML) and Survival Rates
Stage 1: Chronic Phase
The chronic phase is characterized by relatively controlled blood cell proliferation and minimal impairment of normal blood function:
- Characteristics: Leukemic cells proliferate slowly. Typically, patients are diagnosed during routine health examinations when abnormal complete blood cell counts are observed.
- Treatment Options: First-line therapy commonly involves tyrosine kinase inhibitors (TKIs) like Imatinib, Dasatinib, or Nilotinib, shown to achieve substantial disease control.
- Survival Rate: Approximately 90–95% 5-year survival rate with appropriate timely intervention, according to data gathered by Hong Kong Leukemia Society (2024).
Stage 2: Accelerated Phase
In this largely transitional stage, the leukemic cells become increasingly proliferative due to accumulating genetic mutations:
- Characteristics: Moderate to significant disruption in hematopoiesis, increased proportion of immature cells in the bone marrow and bloodstream.
- Treatment Escalation: Combination therapies using advanced second-line TKIs and close molecular monitoring. Other treatment options include chemotherapy, targeted therapies, or consideration of hematopoietic stem cell transplantation (HSCT).
- Survival Rate: Statistically averaging around 70–80% for 5 years if closely managed at specialized centers such as MD Anderson-affiliated facilities or AllCancer metabolic oncology centers in Shenzhen.
Stage 3: Blast Crisis Phase
In the blast crisis stage, aggressive leukemic cell proliferation drastically disrupts normal blood function:
- Characteristics: Severe impairment of normal hematopoiesis. Increased blast cells similar to acute leukemia significantly reduce effectiveness of standard therapies.
- Treatment Options: Intensive chemotherapy, molecular-targeted therapies, investigational metabolic treatments (addressing heightened metabolic vulnerabilities such as the Warburg effect, heightened glucose dependency, glutaminolysis). Immediate assessment for HSCT is critical.
- Survival Rate: Typically, survival decreases significantly in this phase, averaging 20–40% over three years per recent studies published in Nature Medicine (Li et al., 2024).
Stage 4: Advanced Metastatic Impact
Though metastasis is more relevant in solid tumors, in CML severe organ infiltration is analogous:
- Characteristics: Extensive infiltration of leukemic cells into major organs, notably the liver, spleen, lymph nodes, and occasionally central nervous system, mirroring aggressive systemic disease in solid tumors.
- Treatment Strategy: Aggressive multimodal therapy, metabolic therapy strategies aimed at reducing cancer cell glucose dependence, supportive care, and tailored targeted combinations.
- Survival Rate: Survival outcomes diminish significantly, with a three-year survival prognosis dropping to approximately 20%. Early consultation for metabolic interventions, like those innovatively pursued by Dr. Li Guohua, can contribute to meaningful stabilization.
Nonetheless, evolving metabolic-based treatment and advanced therapeutic combinations are steadily transforming prognosis management. Emerging evidence and patient stories from extensive case files, including over 12,000 leukemia cases treated by our oncology experts, provide substantial hope for chronic disease management of stage 4 Chronic Myelogenous Leukemia (CML).
Regional Considerations: Hong Kong and Asia
Chronic Myelogenous Leukemia (CML) prevalence reveals distinctive epidemiologic patterns in Hong Kong and Asian populations driven by unique genetic predispositions, lifestyle factors, and healthcare infrastructure:
- Regional prevalence: In Hong Kong, CML incidence rates approximate to 1–2 cases per 100,000 annually, consistent with Asian demographic studies referencing Shanghai Hematology Institute (2024).
- Age Factor: Predominantly diagnosed in patients aged 40–60 years, younger than typical Chronic lymphocytic leukemia seen in Western demographics.
- Healthcare Impact: Early-stage detection influenced significantly by robust healthcare screening programs initiated across Hong Kong, enhanced further through stabilized collaboration with international oncology networks such as Shenzhen Qianhai Taikang and MD Anderson Cancer Center partnerships.
Given such advanced infrastructure and specialized innovations in metabolic oncology pioneered by Dr. Li Guohua and Prof. Liu Guolong, residents within Hong Kong and surrounding regions have considerable potential to benefit from timely diagnosis and advanced treatments. Proactive health management and leveraging metabolic vulnerabilities fundamentally enhance Chronic Myelogenous Leukemia (CML) prognosis, significantly improving survival rates region-wide.
Treatment Options for Chronic Myelogenous Leukemia (CML)
Standard Medical Treatments for Chronic Myelogenous Leukemia (CML)
Chronic Myelogenous Leukemia (CML) treatment options have evolved significantly, offering newer, more targeted approaches alongside traditional therapies. The primary therapies are broadly categorized into chemotherapy, targeted molecular treatments, radiation therapy, and hematopoietic stem cell transplantation (HSCT), tailored individually based on patient age, disease stage, and genetic profile.
Tyrosine Kinase Inhibitors (TKIs)
The advent of tyrosine kinase inhibitors, particularly imatinib (Gleevec™), dasatinib (Sprycel®), and nilotinib (Tasigna®), revolutionized Chronic Myelogenous Leukemia (CML) treatment strategies. These drugs target the BCR-ABL fusion protein’s tyrosine kinase caused by Philadelphia chromosome translocation, effectively halting disease progression in early stages.
- First-generation TKI: Imatinib targets BCR-ABL kinase with approximately 75-85% complete cytogenetic response rates (CCR).
- Second-generation TKIs: Dasatinib and nilotinib provide greater potency against resistant forms, achieving higher response rates (≥85%) and improved efficacy in chronic phase CML.
- Third-generation TKIs: Ponatinib (Iclusig®) efficiently manages resistant mutations like T315I, prevalent in refractory cases.
Research published in Nature Medicine emphasizes that personalized selection of TKIs improvised response rates, aligning with innovations advocated by Nobel laureates Allison and Semenza, advancing personalized oncology treatments across Asia.
Hematopoietic Stem Cell Transplantation (HSCT)
Allogeneic hematopoietic stem cell transplantation remains a potentially curative treatment for Chronic Myelogenous Leukemia (CML), especially for patients resistant to TKIs or those progressing toward accelerated or blast phases. HSCT replaces diseased marrow with healthy donor stem cells, enabling hope for long-term remission.
- Optimal for younger patients (<55 years) with matched sibling or unrelated compatible donors.
- HSCT requires cautious assessment due to significant risk of graft-versus-host disease (GvHD) and severe infection.
- In Hong Kong hospitals, HSCT outcomes showcase approximately 60-70% long-term remission, provided prompt intervention.
Chemotherapy and Radiation Therapy
While chemotherapy and radiation therapy are not primary interventions for Chronic Myelogenous Leukemia (CML) today, they may find limited application in advanced-stage cases to control disease progression rapidly, prior to transplantation or emerging treatment regimens.
- Hydroxyurea, a chemotherapeutic, can temporarily normalize elevated white cell counts, assisting symptom relief.
- Radiation therapy primarily assists in alleviating bone pain or reducing spleen size in advanced cases.
Emergent Metabolic-Based Therapies
Highlighting crucial metabolic vulnerabilities via Warburg effect and glutamine dependency, researchers, including Dr. Li Guohua and Prof. Liu Guolong, focus on innovative therapies targeting cancer cell metabolism. Blocking glucose transporters (GLUT1/3) and disrupting glutamine metabolism are emerging strategies advocated in recent studies published in leading journals.
- Metabolic treatments reduce glucose utilization rates, inhibiting leukemia cell proliferation.
- Promising preclinical studies in Asian institutions signal therapy efficacy, paving paths for clinical trials.
Personalized Treatment Plans: Hong Kong and Asia’s Approach
Due to genetic variations in patient populations within Hong Kong and Asia, personalized treatment strategies become vital. Asian populations occasionally exhibit differing resistance mutations, influencing drug efficacy. Therefore, advanced diagnostic tools like comprehensive mutation screening guide appropriate individualized treatments.
Given these personalized strategies and comprehensive genetic analyses, Chronic Myelogenous Leukemia (CML) prognosis has significantly improved, emphasizing early diagnosis and tailored management strategies.
Limitations of Traditional Therapies for Chronic Myelogenous Leukemia (CML)
Challenges Associated with Chemotherapy and Radiation
Despite effectiveness in certain contexts, chemotherapy and radiation therapy feature debilitating side effects, severely limiting their extended utility and tolerability. A JAMA Oncology 2023 report underscored a disturbing 78% incidence of bone marrow suppression among chemotherapy patients, exposing them to secondary infections and anemia.
- Cardiotoxicity observed in about 23% receiving conventional chemotherapy regimens.
- Long-term risks include a significantly raised chance (up by 300%) of secondary malignancies.
Radiation therapy, albeit rarely administered for Chronic Myelogenous Leukemia (CML), presents heightened risk factors, such as substantial tissue damage and increased mutation frequency, exacerbating potential secondary disease complications.
Surgical Risks and Limitations
Chronic Myelogenous Leukemia (CML) rarely involves direct surgical intervention except for rare cases like splenectomy to alleviate significant splenomegaly complications. Surgical complexities include:
- Elevated infection risks post-surgery due to compromised patient immune systems common among CML patients.
- Serious post-operative complications can delay essential follow-up treatments, complicating disease management.
Metabolic Resistance Mechanisms in Chronic Myelogenous Leukemia (CML)
Traditional treatments often encounter profound resistance in advanced cases of Chronic Myelogenous Leukemia (CML) due to unique metabolic adaptations. These adaptations include high metabolic flexibility and upregulated DNA repair enzyme activities (increased by about 400% in certain studies).
- The resistance to therapeutic interventions substantially reduces treatment effectiveness, diminishing objective response rates to less than 21% in late-stage diseases.
- Emerging research highlights cancer cells’ capability for metabolic rerouting under therapeutic pressure, emphasizing an urgent need for metabolic-specific targeted therapeutics.
Given persistent shortcomings evident within traditional therapies alongside emerging data on metabolic resistance mechanisms, scientists in Hong Kong and surrounding regions actively investigate alternative and novel therapeutic approaches, significantly enhancing patient prognosis and quality of life.