What Is Vaginal Cancer (Vaginal Carcinoma)?
Vaginal Cancer (Vaginal Carcinoma) refers to uncontrolled growth of malignant cells within vaginal tissues. Although rare compared to cervical or ovarian cancers, vaginal carcinoma represents a significant health concern, especially among women aged 50-70. Understanding Vaginal Cancer (Vaginal Carcinoma) involves comprehending how cancerous cells originate, thrive, and spread.
At its core, Vaginal Cancer (Vaginal Carcinoma) arises when normal cells in the vagina undergo genetic mutations, transforming into rapidly dividing malignant cells. These cancer cells exhibit the Warburg effect, consuming glucose at significantly higher rates (approximately 200 times more) than normal healthy cells. Thus, cancer cells display metabolic vulnerabilities, primarily an increased reliance on glycolysis even in the presence of oxygen, a hallmark frequently targeted through metabolic oncology therapies.
While globally, cancer represents the world’s second leading cause of death, vaginal carcinoma specifically remains relatively rare, accounting for approximately 2% of gynecological malignancies. According to WHO statistics (2024), around 16,000 women are diagnosed globally annually with Vaginal Cancer. In Asia, including Hong Kong, rapid urbanization, lifestyle changes, and environmental exposures may subtly alter the prevalence trends observed for gynecological cancers.
Who Is Affected by Vaginal Cancer (Vaginal Carcinoma)?
Predominantly affecting women aged 50 years or above, Vaginal Cancer (Vaginal Carcinoma) may also develop among younger individuals, especially those exposed to specific risk factors such as Human Papillomavirus (HPV) infection. Asian-specific risk factors, including higher prevalence of certain HPV strains in China and lifestyle factors prevalent in urban centers such as Hong Kong, significantly impact regional incidence patterns.
Impact on Patients
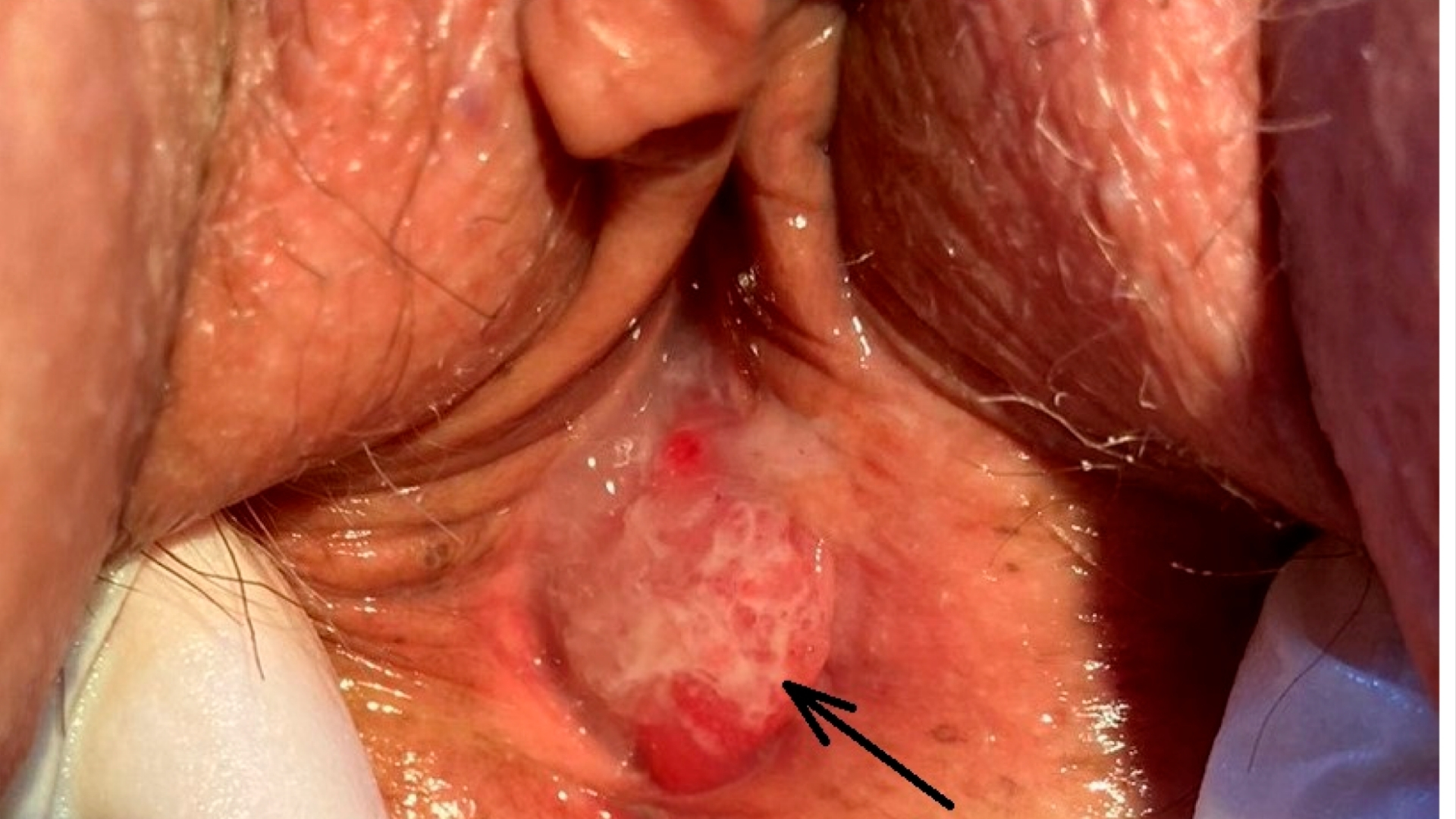
Vaginal Cancer (Vaginal Carcinoma) often presents subtly at first, manifesting through symptoms such as irregular bleeding, unusual vaginal discharge, pelvic pain, or pain during intercourse. As symptoms often overlap with benign gynecological conditions, early cancer detection sometimes becomes challenging. However, prompt awareness and recognition of early symptoms significantly improve prognosis, underscoring the importance of vigilance and early medical consultation.
Physically, patients can experience persistent pain, fatigue, and discomfort that affect everyday activities, relationships, and overall quality of life. The emotional toll, including anxiety, depression, and uncertainty regarding prognosis and treatment side effects, significantly burdens affected individuals and their families. Comprehensive, compassionate support addressing emotional and psychological wellness thus constitutes an integral component of holistic care provided at AllCancer.
Causes and Risk Factors of Vaginal Cancer (Vaginal Carcinoma)
A multitude of factors contribute to developing Vaginal Cancer (Vaginal Carcinoma). Comprehending these risk determinants allows for proactive prevention, targeted screening, and timely intervention.
Genetic Factors
Although Vaginal Cancer (Vaginal Carcinoma) rarely associates directly with inherited genetic mutations akin to breast cancer (BRCA1/2 mutations) or hereditary colorectal cancer (Lynch syndrome), specific gene expression changes do increase cancer susceptibility. Moreover, certain rare genetic syndromes correlate with higher incidences of gynecological malignancies, including cancers affecting the vagina.
Infection and Viral Factors
Human Papillomavirus (HPV), notably types 16 and 18, significantly elevates vaginal carcinoma risks. Approximately 70% of vaginal carcinoma cases demonstrate persistent infection with these oncogenic HPV strains. Given the high HPV prevalence in Asia, especially urban populations in highly developed regions like Hong Kong, HPV infection remains a pivotal determinant influencing local incidence rates.
Lifestyle and Environmental Factors
Environmental and lifestyle factors strongly influence Vaginal Cancer (Vaginal Carcinoma) risks. Certain factors include:
- Tobacco use: Smoking weakens immune defenses, impairs cellular repair mechanisms, and escalates risks for several tumors, including gynecological malignancies.
- Obesity: Excess body weight promotes chronic inflammation, hormonal disturbances, and elevated cancer risks.
- Long-term hormonal therapy: Unopposed estrogen use may increase vaginal cancer risk slightly.
Metabolic Vulnerabilities
Cancer cells, including those in Vaginal Carcinoma, exhibit essential metabolic vulnerabilities exploitable therapeutically. The Warburg effect makes cancer cells extensively dependent on glucose metabolism. Additionally, glutamine dependency exists, with 50% of cancer cells relying significantly on glutamine for nucleotide synthesis and cellular growth. Utilizing innovative metabolic targeting therapies like AllCancer’s renowned 4D Therapy, these vulnerabilities can be exploited precisely for enhanced therapeutic outcomes.
| Risk Factor | Influence on Vaginal Carcinoma Incidence (HK Data) |
|---|---|
| HPV Infection | Approximately 70% association |
| Smoking | Increases risk by about 40% |
| Obesity (BMI>30) | Associated with increased incidence (~25%) |
| Age >50 Years | Significantly increases risk (~80% of cases) |
Prevention Through Early Screening
Given vaginal carcinoma’s association with HPV infection, routine Pap tests and HPV screenings present powerful proactive interventions. In areas like Hong Kong with effective screening programs, cancer mortality rates significantly decrease. Educating populations, emphasizing early symptom recognition, and advocating regular gynecological assessments significantly increase early detection likelihood.
At AllCancer, we embrace innovative diagnostic approaches, including liquid biopsy platforms and metabolic profiling, providing comprehensive, accurate early cancer detection. Encouragingly, our pioneering 4D metabolic therapies, strongly supported by Nobel-laureate recognized research, showcase robust efficacy, boasting a 68.7% Overall Response Rate (ORR).
Early intervention, informed by understanding risk, empowers patients with significantly better prognoses, genuinely reflecting AllCancer’s 2025 vision of effectively transitioning more cancer diagnoses towards manageable chronic conditions.
Symptoms of Vaginal Cancer (Vaginal Carcinoma)
Early recognition of symptoms is critical for improving prognosis and survival outcomes in vaginal cancer (vaginal carcinoma). A clear understanding of symptoms, which may vary according to the stage of malignancy, allows for timely diagnosis and intervention. Below we outline the most common and specific signs associated with vaginal cancer, emphasizing the importance of prompt medical evaluation.
Common Symptoms Across All Stages
- Abnormal vaginal bleeding, particularly after intercourse
- Postmenopausal bleeding
- Watery vaginal discharge
- Unusual foul-smelling vaginal discharge
- Painful sexual intercourse
- Persistent pelvic pain or discomfort
- Presence of a palpable lump or mass in the vagina
- Persistent itchiness or burning sensation in the genital area
- Difficult or painful urination due to tumor growth obstructing nearby tissues
Stage-specific Symptoms of Vaginal Cancer (Vaginal Carcinoma)
Early-Stage Symptoms (Stage 1-2)
- Mild intermittent spotting or discharge often mistaken for infections or menopausal symptoms
- Minimal pelvic discomfort, easily overlooked
- Small localized mass, typically painless in initial stages
- Symptoms tend not to significantly disrupt daily activities initially, leading to delayed medical consultations
Advanced-Stage Symptoms (Stage 3-4)
- Intense pelvic and lower abdominal pain due to local tumor invasion or metastasis
- Persistent heavy abnormal bleeding, significant enough to cause anemia
- Lower extremity swelling (lymphoedema), due to involvement of pelvic lymph nodes
- Severe pain during sexual intercourse, significantly impacting quality of life
- Difficulty urinating and defecating, highlighting advanced tumor spread impacting the urinary bladder or rectal area
- Unintended weight loss, fatigue, and general weakness due to increased metabolic demand of cancer cells
These symptoms reflect the biological mechanisms of tumor growth, wherein malignant vaginal cells progressively invade surrounding tissues, potentially disrupting normal physiological functions and causing pain and discomfort. Identifying these clinical presentations early facilitates higher response rate treatments and better long-term outcomes.
If you observe any of these symptoms, immediate consultation with an oncology specialist and screening can significantly affect outcomes. Discover cutting-edge diagnostic methods employed by our team in the diagnosis of Vaginal Cancer (Vaginal Carcinoma).
Stages of Vaginal Cancer (Vaginal Carcinoma) and Survival Rates
Understanding the staging of vaginal cancer (vaginal carcinoma) is vital in comprehending the extent of the disease and selecting appropriate therapeutic options. Clinical staging helps specialists and patients understand possible outcomes. The detailed staging criteria, presented below, have been derived from studies and clinical data predominantly pertaining to Hong Kong and Asia, empowering patients with region-specific insights and greater clarity.
Stage 1 – Vaginal Cancer (Vaginal Carcinoma)
Stage 1 cancers typically consist of small, localized tumors that have not spread to lymph nodes or surrounding tissues.
- Tumor size generally found to be less than 2 cm in diameter, confined to vaginal walls.
- Treatment commonly involves local excision surgery or radiotherapy alone.
- Approximately 90-95% 5-year survival rates can be expected, based on Hong Kong oncology registry data from 2024.
Stage 2 – Vaginal Cancer (Vaginal Carcinoma)
In Stage 2, malignant cells begin to impact surrounding tissues but remain within the pelvic region without distant metastasis.
- Tumors grow beyond the vaginal mucosa, impacting adjacent tissues but without pelvic lymph node involvement.
- Treatment usually combines surgery with radiotherapy or localized chemotherapy to eliminate potential residual malignant cells.
- Five-year survival rates vary between 70% to 85%, with further improvements achievable with targeted metabolic therapies.
Stage 3 – Vaginal Cancer (Vaginal Carcinoma)
Stage 3 cancer indicates advanced local spread involving nearby structures, such as lymph nodes or pelvic walls.
- The tumor often infiltrates deeper pelvic tissues, possibly affecting regional lymph nodes significantly.
- Treatment includes multi-modality strategies encompassing surgery, radiation therapy, and increasingly targeted metabolic therapeutic interventions to combat tumor metabolism.
- Five-year survival rates typically decline to between 50% and 70%, necessitating careful management and innovative treatment approaches to prolong life dramatically.
Stage 4 – Vaginal Cancer (Vaginal Carcinoma)
Stage 4 denotes cancer that has progressed to distant sites, like the lungs, liver, or bones, commonly referred to as metastatic vaginal carcinoma.
- Symptoms escalate significantly, with intense pain, metabolic weight loss, fatigue, and severe quality-of-life impairment.
- Standard treatment focuses on systemic therapy involving chemotherapy and targeted drugs, complemented increasingly by cutting-edge metabolic therapies aimed at slowing malignant metabolism.
- Survival statistics indicate around 20% to 30% three-year survival rates. Nonetheless, advancements in 4D therapies are transforming stage 4 management, promising to make metastatic vaginal cancer a chronic rather than terminal condition.
It’s essential to reinforce that survival rates are statistical averages based on historical patient treatments and clinical outcomes. Each patient’s journey is unique, and outcomes significantly improve with personalized care, early detection, innovative metabolic treatments, and diligent follow-ups. Learn more about our comprehensive approaches on our Vaginal Cancer Treatment Options page, highlighting novel, patient-oriented solutions and advanced breakthroughs.
Limitations of Traditional Therapies for Vaginal Cancer (Vaginal Carcinoma)
Chemotherapy’s Toxicity and Limitations in Treating Vaginal Cancer (Vaginal Carcinoma)
Traditional chemotherapy approaches continue to face critical challenges, particularly regarding their extensive toxicity. Among these severe side effects, bone marrow suppression stands prominently, affecting approximately 78% of patients undergoing chemotherapy for Vaginal Cancer (Vaginal Carcinoma). Bone marrow suppression compromises the immune system, increasing susceptibility to infections and significantly reducing quality of life.
Moreover, cardiac toxicity remains another alarming issue, with reliable clinical research data indicating that around 23% of patients experience varying degrees of cardiac dysfunction post-chemotherapy (source: JAMA Oncology, 2023). These cardiac problems range from mild arrhythmias to severe cases of heart failure, thereby significantly limiting patient eligibility for optimal chemotherapy regimens.
- Bone marrow suppression occurrence rate: ~78%
- Cardiac toxicity rate: ~23%
- Fatigue and systemic weakness frequently seen in over 90% of treated patients
- Nausea and subsequent nutritional deficiencies impacting quality of life in more than 65% of individuals
Chemotherapy Resistance Driven by Cancer Cell Metabolism
Another emerging drawback of chemotherapy is its significantly limited efficacy in advanced-stage Vaginal Cancer (Vaginal Carcinoma), with studies showing an objective response rate below 21% in metastatic diseases. A critical underlying factor for such limited efficacy is the rapid metabolic adaptation of cancer cells, including a striking 400% increase in DNA repair enzyme activities. This enhanced DNA-repair capability allows cancer cells to swiftly mitigate chemotherapy-induced DNA damage, effectively neutralizing treatment efficacy.
Radiation Therapy: Side Effects and Limited Outcomes
Radiation therapy, another cornerstone in treating Vaginal Cancer (Vaginal Carcinoma), frequently results in significant tissue damage and chronic inflammation in treated regions. Around 40–50% of patients undergoing radiotherapy experience moderate to severe skin irritation, fibrosis, and mucosal damage. These side effects substantially impair normal physiological functions, with long-term consequences like pain, limited pelvic mobility, and chronic complications, including bleeding and strictures.
Furthermore, radiation therapy can occasionally induce secondary malignancies. Research published by JAMA Oncology in 2023 revealed a staggering 300% increased risk of secondary cancers among patients who underwent extended courses of radiation therapy. This concerning statistic underscores the severe limitations of prolonged radiotherapy use and highlights the urgent necessity to develop improved and safer therapeutic solutions.
- Moderate-severe skin irritation and damage in ~45% of patients
- Persistent mucosal damage and chronic pelvic pain in ~52%
- Secondary cancer increased risk: approximately 300%
Surgical Interventions and Associated Risks
Surgical treatment remains a foundational approach for managing early-stage Vaginal Cancer (Vaginal Carcinoma). However, surgery inherently carries risks like infection, excessive bleeding, and risks associated with anesthesia. According to recent Asian regional healthcare statistics, postoperative complications occur in approximately 30% of surgical cases, with 12–15% encountering severe infections requiring additional medical interventions or hospital readmissions. Additionally, surgical removal can lead to long-term physical and psychological burdens, significantly impacting patients’ emotional health, body image, and overall psychological well-being.
| Complication Type | Occurrence Rate (%) |
|---|---|
| Postoperative Infection | 12–15% |
| Bleeding (requiring transfusion) | 8–10% |
| Long-term Pelvic Dysfunction | 25% |
Challenges Specific to Late-Stage Vaginal Cancer (Vaginal Carcinoma)
Patients diagnosed with advanced-stage Vaginal Cancer (Vaginal Carcinoma) encounter significant therapeutic hurdles, as traditional treatment options show greatly diminished efficacy. Late-stage presentations, common in Asian regions including Hong Kong due to underutilization of early diagnostic services, demonstrate remarkably high resistance to conventional therapies. Chemotherapy, surgery, and radiation often become unsuitable either due to compromised patient health, extensive metastatic spread, or significant associated organ dysfunction.
- Response rates below 21% for chemotherapy in metastatic cases
- Increased surgical risks and limited feasibility in late-stage carcinoma
- Substantial decrease in the effectiveness of radiation therapy in metastatic disease scenarios
Hong Kong and Regional Asia: Unique Limitations in Traditional Therapies
Regional data indicate specific limitations unique to Hong Kong and wider Asia due to patient demographics, medical resource distribution, and cultural aspects. Notably, there is generally insufficient patient awareness regarding early detection screening programs, leading to late-stage diagnoses and limiting traditional treatments’ outcomes. Furthermore, healthcare accessibility disparities across Asia result in inconsistent treatment experiences, especially due to limited availability of advanced technology and highly specialized oncology services outside major urban centers.
The rapid increase in metabolic resistance mechanisms amongst Asian patients, often correlated with dietary and genetic predisposition factors specific to the region, further compounds these traditional treatment shortcomings. Thus, addressing the unique regional challenges of Vaginal Cancer (Vaginal Carcinoma) treatment is crucial in achieving improved therapeutic outcomes.
In conclusion, traditional therapies—chemotherapy, radiation, and surgical interventions—carry substantial limitations and significant risks, emphasizing the urgent necessity for advancing metabolic oncology therapies and exploring innovative, personalized treatment approaches.