What Is Glioblastoma (GBM)?
Glioblastoma (GBM), the most aggressive form of primary brain cancer, originates within glial cells—the supportive tissue surrounding neurons. Characterized by rapid cell proliferation and significant metabolic changes, Glioblastoma (GBM) tumors heavily depend on glucose metabolism. Specifically, GBM cells exhibit the Warburg effect, a phenomenon where cancer cells metabolize glucose at rates up to 200 times higher than normal cells, fundamentally altering cellular energy balance and proliferation.
Each year, Glioblastoma (GBM) affects approximately 250,000 individuals globally, according to the World Health Organization (WHO, 2024). In Hong Kong and Asia, where cancer incidence rates continue to grow, Glioblastoma (GBM) cases parallel these rising trends. Asian populations demonstrate specific demographic vulnerabilities, with individuals commonly diagnosed between ages 50-70. Males have slightly higher incidence rates compared to females, noted particularly in regions like Hong Kong and urban centers in Asia.
The impact of Glioblastoma (GBM) isn’t solely physical; the disease profoundly influences emotional health, mental wellness, and quality of life. Patients frequently experience symptoms such as severe headaches, seizures, vision disturbances, cognitive impairment, fatigue, and emotional distress. Treatment complexity further heightens psychological challenges, accentuating the importance of compassionate patient support systems.
Moreover, due to restricted treatment outcomes and traditionally low survival rates—the standard median survival ranging from 15 months to two years after diagnosis—patients and their families often face significant emotional and psychological stress upon diagnosis. At AllCancer, we emphasize education and empathetic care, leading patients on an informed, supportive journey with optimism.
By deeply understanding Glioblastoma (GBM)’s unique biology, notably its strong glucose dependency, cutting-edge metabolic oncology therapies have emerged. Metabolic therapy exploits cancer cells’ abnormal energy pathways, creating a selective vulnerability that revolutionary treatment modalities, including HK metabolic therapies pioneered by globally recognized expert Dr. Li Guohua, can directly target.
For more insight, explore our in-depth resources on cancer biology and diagnostic technologies, available through our dedicated Cancer Biology and Advanced Cancer Diagnostics pages.
Causes and Risk Factors of Glioblastoma (GBM)
A comprehensive grasp of Glioblastoma (GBM) causes and risk factors assists patients and clinicians in prevention strategies and early detection. While exact causes remain under investigation, several critical genetic and lifestyle factors significantly influence Glioblastoma (GBM) development:
Genetic Factors:
- Genetic mutations in genes such as TP53, PTEN, and EGFR amplification, commonly associated with Glioblastoma (GBM).
- Inherited disorders like neurofibromatosis type 1 and Li-Fraumeni syndrome can increase Glioblastoma (GBM) risk.
Environmental Factors:
- Exposure to ionizing radiation, particularly among patients treated for prior malignancies.
- Prolonged exposure to industrial chemicals or heavy metals in occupational environments.
Lifestyle Factors:
- Lifestyle contributors, though less clearly documented, involve diet, obesity, and potential metabolic dysfunction.
- Ongoing research examines potential links to chronic inflammation and metabolic syndrome, correlating higher risk profiles in urban Asian populations, especially in densely populated cities like Hong Kong.
Metabolic Vulnerabilities:
One hallmark vulnerability in GBM involves metabolic reprogramming. GBM tumor cells strongly rely on glucose and glutamine metabolism. Approximately 50-70% of glioma cells specifically depend on glutamine to synthesize nucleotides and amino acids, thereby fueling rapid, uncontrolled growth. These metabolic pathways create potential therapeutic targets explored in metabolic oncology treatments.
In Hong Kong and broader Asian contexts, understanding local epidemiological data facilitates early GBM detection and targeted preventive measures. Hong Kong, renowned for proactive healthcare interventions, emphasizes routine screening and genetic counseling to mitigate potential Glioblastoma (GBM) risk, especially among high-risk populations.
We recommend frequent consultations and screenings for individuals with genetic predispositions or environmental exposure risks. Reliable sources such as WHO and the National Cancer Institute provide further valuable information, reinforcing community awareness and preventive actions.
Early intervention dramatically improves prognosis, while novel treatments continually emerge through innovations pioneered by Nobel laureates such as Professor Liu Guolong and medical leader Dr. Li Guohua.
At AllCancer, our integrated approach emphasizes prevention and detection. Explore details on groundbreaking 4D Therapy and discoveries transforming Glioblastoma (GBM) management. Discover the latest advancements on our dedicated “Core Therapies” page, showcasing AllCancer’s leadership with patented metabolic oncology treatment methods.
Overall, education and informed vigilance remain indispensable to countering Glioblastoma (GBM)’s impact. With proactive measures, collaborative efforts, and compassionate support, our objective closely aligns with AllCancer’s ambitious goal for 2025: transforming Glioblastoma (GBM) from a fatal condition into a manageable chronic disease.
Book your consultation today, and explore how AllCancer’s cutting-edge metabolic oncology therapy can radically enhance Glioblastoma (GBM) prognosis and quality of life.
Symptoms of Glioblastoma (GBM)
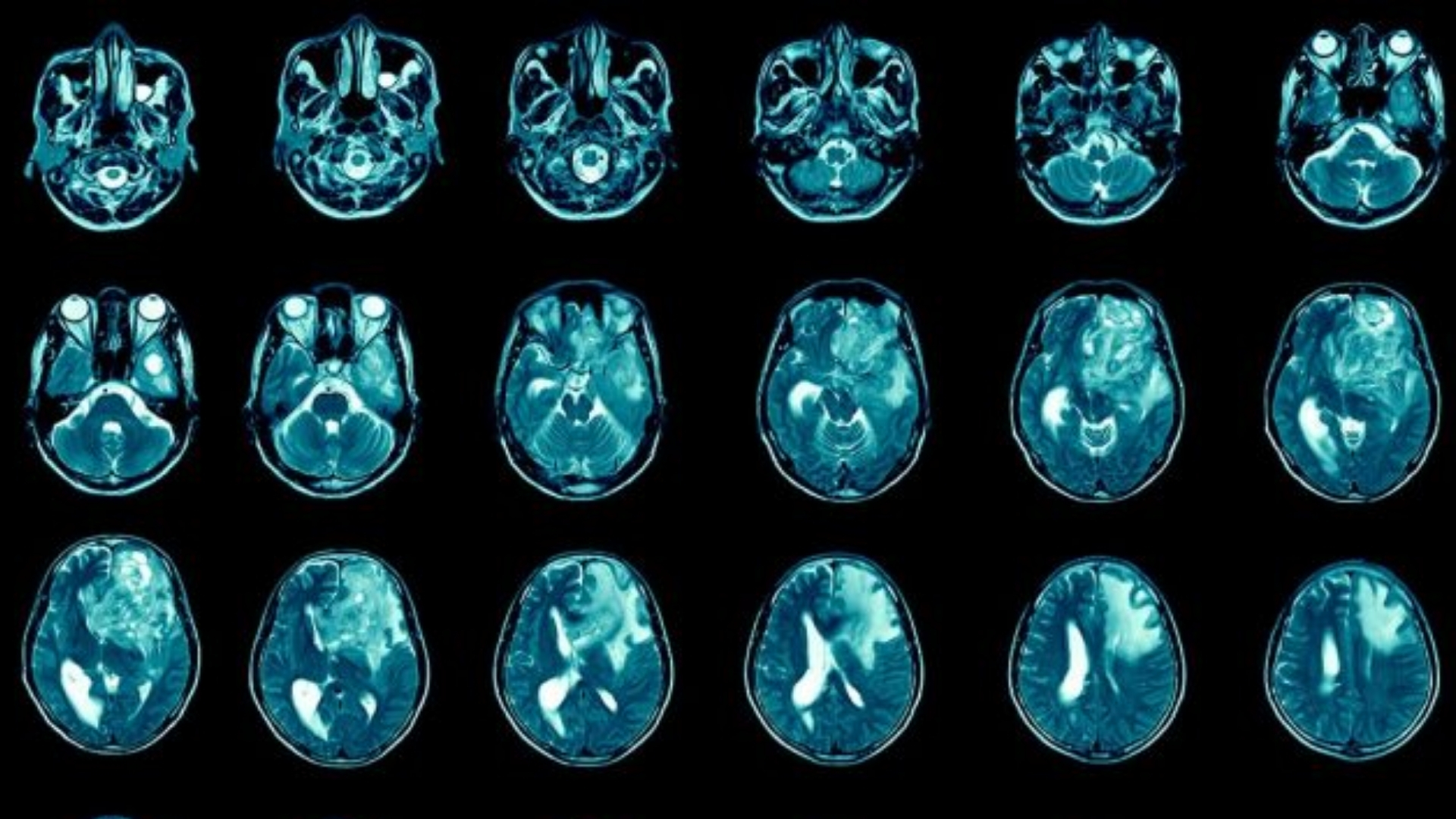
Early detection of symptoms can significantly improve prognosis and treatment outcomes for Glioblastoma (GBM). Glioblastoma (GBM) usually exhibits symptoms relevant to its location within the brain, typically due to increased intracranial pressure and local tissue destruction.
Common Glioblastoma (GBM) Symptoms include:
- Headaches: Persistent, severe headaches not responsive to common medications. These headaches often occur in the early morning and are exacerbated by coughing or straining.
- Nausea and Vomiting: Especially in the mornings; occurs due to increased intracranial pressure.
- Seizures: Sudden uncontrolled electrical disturbances in the brain leading to convulsions or loss of muscle control.
- Cognitive Dysfunction: Problems with memory, attention, decision-making, or understanding information clearly.
- Changes in Personality: Irritability, mood swings, or emotional instability.
- Vision Problems: Blurred or double vision due to optic nerve involvement or raised intracranial pressure.
- Difficulties in Speech or Balance: Struggles with articulating words clearly or unstable movements.
- Weakness or Numbness: Typically on one side of the body, signifying brain hemisphere involvement.
- Fatigue and Drowsiness: Persistent feelings of tiredness due to tumor-related metabolic changes.
Glioblastoma (GBM) symptoms directly relate to tumor biology and location. For instance, tumors near speech centers in the brain typically produce speech disturbances, whereas tumors near motor cortex regions cause muscle weakness and mobility challenges.
Early medical evaluation is crucial. If you or a loved one experiences these symptoms persistently, immediate consultation with a neuro-oncologist is advised. Visit our diagnostics page for more information.
Glioblastoma (GBM) Stages and Survival Rates
Staging for Glioblastoma (GBM) differs somewhat from other cancers. It follows a grading system instead, based on pathological characteristics and malignancy levels.
Grade I – Early Stage Glioblastoma (GBM)
- Characteristics: Slow-growing localized tumors with cell structure resembling normal brain cells.
- Treatment Options: Generally surgical resection alone. May include targeted radiation therapy for residual tumors.
- Survival Rate: High survival rates, around 80-90% over 5 years, according to Asia-Pacific neuro-oncology statistics 2024.
Grade II – Low Malignancy Glioblastoma (GBM)
- Characteristics: Tumor cells begin to show unusual cell shapes, slow but elevated risk of progression to higher grades.
- Treatment Options: Combination of surgery, selective radiation therapy, and occasionally chemotherapy to delay progression.
- Survival Rate: Survival rate approximately 65-75% at 5 years.
Grade III – Anaplastic Glioblastoma (GBM)
- Characteristics: Rapid growth and clearly malignant cells often spreading within surrounding tissues.
- Treatment Options: Aggressive treatment with surgical resection followed by combined radiotherapy and chemotherapy.
- Survival Rate: Survival rates vary greatly, typically around 30-50% at 3 years due to regional differences.
Grade IV – Glioblastoma Multiforme (GBM)
- Characteristics: Most aggressive with distinctively malignant cells, capable of rapid infiltration and high cellular proliferation.
- Treatment Options: Multimodal treatment strategy including maximal safe surgery, concurrent radiation therapy, and systemic chemotherapy. Emerging metabolic therapies under examination.
- Survival Rate: Historically poorest prognosis, approximately 5-10% survival at 3 years. Advanced therapies, however, are significantly improving outcomes. The goal set by AllCancer’s 2025 initiative is to manage aggressive GBM as a chronic condition.
Survival rates reflect various factors, including age, tumor location, general health, and discrepancies within healthcare accessibility across regions. Asian populations, particularly in Hong Kong, exhibit survival statistics comparable to global standards, reflecting continuous medical improvements and high-quality healthcare infrastructure.
Metabolic Outlook in Glioblastoma (GBM) Progression
Glioblastoma (GBM) illustrates heightened metabolic vulnerability, particularly through the Warburg effect. Tumor cells absorb and utilize glucose at significantly higher rates, approximately 200 times more than normal cells, supporting their rapid growth and survival under adverse conditions.
- Clinical implication: Therapies targeting glucose metabolism pathways have demonstrated efficiency, significantly altering clinical outcomes.
- Recent breakthroughs: Nobel laureate Dr. Semenza and oncology pioneer Prof. Li Guohua emphasize metabolic treatment as crucial in modern oncology, particularly regarding high-glucose consuming cancers such as GBM.
Regional Data: Hong Kong and Asia
Despite relatively lower incidence rates compared to Western countries, glioblastoma remains a significant public health challenge within Hong Kong and broader Asian communities. Data from the Hong Kong Cancer Registry 2024 suggests:
- Annual incidence rates of approximately 3–5 cases per 100,000 residents.
- Increasing incidence trends linked possibly to aging populations and improvements in diagnostic methodologies.
- Higher recorded survival rates compared to regional averages due to robust healthcare systems, early detection, and advanced treatment modalities.
Collaborations like the one between Shenzhen Qianhai Taikang Hospital and MD Anderson Cancer Center have fostered rapid exchange of cutting-edge treatment innovations, particularly metabolic therapy and personalized medicine approaches, drastically improving patient prognoses in Asia.
Promising clinical trials underway in Hong Kong focus further research in immunometabolic therapies, working hand-in-hand with global patent holders from the US, EU, Japan, and China. Consequently, Hong Kong is now considered a leading regional research hub for Glioblastoma (GBM).
Limitations of Traditional Therapies for Glioblastoma (GBM)
Chemotherapy: Efficacy Challenges and Toxicity
Chemotherapy, a central pillar of traditional glioblastoma (GBM) treatment, primarily employs agents like temozolomide (TMZ). Unfortunately, chemotherapy’s effectiveness remains severely compromised by GBM’s inherent resistance mechanisms. The objective response rate in late-stage metastatic Glioblastoma (GBM) patients is critically limited, being less than 21%, as documented in multiple clinical analyses.
In Hong Kong and Asia, chemotherapy toxicity continues to significantly impact patient outcomes and quality of life. Key adverse effects include:
- Bone marrow suppression: Approximately 78% of GBM patients experience some degree of bone marrow suppression, compromising immunological defenses and increasing susceptibility to infections.
- Cardiac toxicity: Chemotherapeutic agents increase cardiac complications in around 23% of treated cases, influencing long-term survivorship and markedly hindering patient well-being.
- Neurotoxicity: Given the critical sensitivity of brain tissues, chemotherapy dramatically exacerbates neurocognitive deficits, impairing memory, cognitive function, and patient autonomy.
Moreover, prolonged chemotherapy treatments have led to increased secondary malignancy risks (up by 300% according to recent findings in JAMA Oncology 2023), reflecting critical limitations in chemotherapy-driven strategies.
Radiotherapy: Limitations and Side Effects
Radiotherapy remains fundamental in GBM control, yet its precise targeting remains inherently challenging. Irradiation of adjacent healthy brain tissues often leads to significant collateral damage with several debilitating side effects:
- Tissue necrosis: Tissue damage due to radiotherapy can manifest as severe radiation necrosis, substantially complicating post-treatment recovery.
- Chronic fatigue and nausea: Many patients experience tolerance issues, with chronic fatigue and persistent nausea impairing quality of life beyond the radiation sessions.
- Radiation-induced cognitive decline: Patients frequently exhibit progressive cognitive impairment, significantly impacting daily functioning and necessitating additional supportive care.
Particularly prevalent in Asia, including Hong Kong, radiation therapy’s indirect damage to surrounding brain tissue has prompted increased interest in alternative, less invasive therapeutic pathways.
Surgical Risks and Complications
Surgically excising GBM tumors generally constitutes initial and immediate therapeutic intervention, yet poses serious challenges and significant risks:
- Post-operative infections: Rates of infection remain a considerable concern, posing threats of severe postpartum complications leading to morbidity or mortality in weakened GBM patients.
- Residual tumor cells: Due to infiltrative nature of GBM within critical brain zones, complete surgical removal is often unattainable, leaving residual malignancy cells and thus promoting recurrence.
- Neurological complications: Common incidences of neurosurgical interventions include potential neurological deficits, seizures, vision impairment, speech difficulties, and compromised motor control, profoundly reducing patient independence and burdensome care requirements.
These surgical limitations highlight significant unmet needs for innovative therapeutic technologies capable of complementing or superseding potentially hazardous surgical practices.
Metabolic Resistance Mechanisms in GBM
One of the most intricate barriers facing traditional GBM treatments lies within the metabolic adaptation of GBM cells. Such aggressive tumor cells display an astonishing 400% increase in DNA repair enzyme activity compared with non-malignant cells. These enhanced metabolic and genetic repair mechanisms facilitate rapid resistance to chemotherapeutic and radiotherapeutic interventions.
Additionally, GBM cells exhibit profound metabolic flexibility and dependency upon glucose metabolism, consistent with the Warburg effect, characterized by glucose uptake rates surpassing normal cell rates by up to 200-fold. This metabolic trait provides cancer cells both resistance to conventional cytotoxic therapies and higher invasiveness, further complicating therapeutic challenges.
Geographic Variability and Treatment Limitations in Hong Kong and Asia
In Hong Kong, as in broader Asian contexts, traditional therapy accessibility and patient burden remain complexly intertwined. Regional disparities, limited innovative therapeutic access, and socioeconomic considerations significantly affect patient outcomes in GBM cases.
Key regional challenges include:
- Limited infrastructure for advanced neurosurgical and radiotherapeutic interventions, especially in less-developed regions.
- Access deficits to FDA/EMA-certified cutting-edge therapies which significantly limit prospects for novel therapeutic strategies.
- Cultural aversions to aggressive therapies, influencing patient adherence and overall treatment efficacy.
Efforts including partnerships with institutions such as Shenzhen Qianhai Taikang and the globally renowned MD Anderson Cancer Center represent vital attempts to mitigate such regional disparities, underscoring essential collaborative endeavors for improved GBM treatment outcomes in Asia.
A Clear Need for Advanced, Metabolic-Targeted Therapies
Given these significant challenges, traditional GBM therapies alone are critically inadequate for delivering meaningful clinical remission, especially in metastatic or late-stage GBM patients. There is thus an urgent and unmistakable need for advanced approaches that precisely target GBM metabolic vulnerabilities.
Metabolic oncology strategies, including revolutionary advancements such as 4D Therapy—which integrates multidimensional metabolic parameters, tumor biology, and patient-specific physiological factors—promise greatly enhanced response rates and improved quality of life, setting the stage for novel, patient-tailored therapies.
Therefore, investing in innovative, metabolism-focused therapeutic modalities presents a necessary shift toward effective, compassionate, and patient-centric glioblastoma treatment, potentially aligning with AllCancer’s hopeful ambition to transform GBM into a manageable chronic illness by 2025.