What Is Hepatocellular Carcinoma (Liver Cancer)?
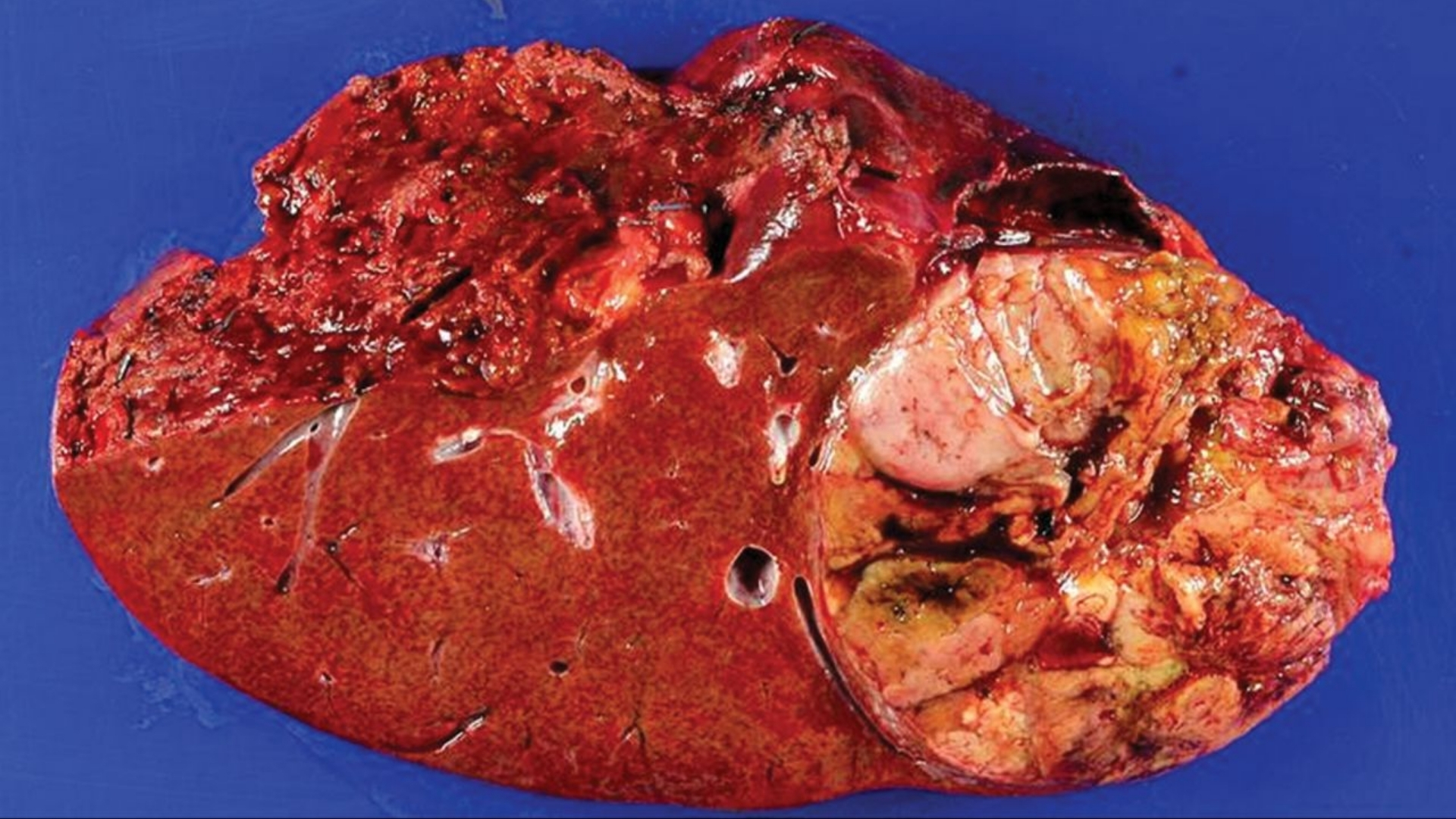
Hepatocellular Carcinoma (Liver Cancer), widely known as primary liver cancer, initiates within hepatocytes—the functional cells of the liver. This cancer represents an abnormal growth of cells that invade surrounding tissues and often metastasize to distant organs. Liver cancer, particularly Hepatocellular Carcinoma, poses significant challenges worldwide, notably prevalent across Asia and particularly within regions such as Hong Kong.
The biological basis of Hepatocellular Carcinoma is rooted deeply in abnormal metabolic pathways. Almost all liver cancer cells showcase an extraordinary phenomenon known as the Warburg effect, whereby cancerous hepatocytes consume glucose at approximately 200 times the normal metabolic rate. Cancer cells adopt aerobic glycolysis even when sufficient oxygen is present, favoring rapid cell proliferation and growth.
Hepatocellular Carcinoma (Liver Cancer) ranks as the fifth most common malignancy internationally, accounting annually for over 850,000 diagnoses and approximately 800,000 deaths per WHO 2024 statistics. Asia accounts for more than 70% of all liver cancer cases, driven largely by regionally specific factors such as high hepatitis B and hepatitis C virus prevalence.
In Hong Kong specifically, liver cancer represents the fourth leading cause of cancer-related mortality, laying considerable burden upon families, healthcare systems, and the affected individuals themselves. Men are disproportionately affected within the Asia-Pacific region; the male-to-female ratio is approximately 3:1, predominantly due to lifestyle and environmental determinants unique to the population.
Emotionally and physically, Hepatocellular Carcinoma significantly impacts an individual’s quality of life. Patients often grapple with persistent fatigue, abdominal pain, reduced appetite, unexplained nausea, cachexia, and psychological distress. Supportive care addressing both emotional and physical symptoms is crucial in managing the patient journey compassionately.
Understanding Hepatocellular Carcinoma (Liver Cancer) facilitates early detection and effective management, significantly enhancing patient prognosis. Discover more about cancer biology, diagnostics, and other related educational resources here.
Causes and Risk Factors of Hepatocellular Carcinoma (Liver Cancer)
Defining and understanding the causes and risk factors of Hepatocellular Carcinoma (Liver Cancer) serve as essential components of effective disease prevention and management. These risk factors encompass a complex interplay of genetic, environmental, lifestyle, and metabolic components specific to populations in Hong Kong and the broader Asian region.
Genetic Factors
Genetic predisposition significantly contributes to liver cancer susceptibility. Notably, somatic mutations in genes such as TP53, CTNNB1, and TERT promoter mutations have been found predominantly in Hepatocellular Carcinoma patients. Specific inherited genetic conditions, including hemochromatosis and Wilson’s disease, further amplify individual risk factors.
- TP53: tumor suppressor gene mutated in approximately 30% of cases.
- CTNNB1 mutations occurring in approximately 20% of liver cancer cases.
- TERT promoter mutations implicated in maintaining telomere length associated with cell immortality and tumorigenesis.
Environmental Factors
Environmental influences are critical to the onset and progression of liver cancer. Chronic exposure to aflatoxins, environmental contaminants produced by fungi growing chiefly on peanuts and corn improperly stored, is prevalent across many Asian and African nations, greatly exacerbating Hepatocellular Carcinoma prevalence.
Moreover, environmental conditions like chronic viral hepatitis B and C are significant triggers. Hepatitis B infection alone increases liver cancer risk up to 100-fold; in Hong Kong, chronic hepatitis B infection prevalence remains high, contributing substantially to Hepatocellular Carcinoma cases.
Lifestyle-Related Factors
Lifestyle choices also profoundly impact Hepatocellular Carcinoma occurrence. Chronic alcohol consumption accelerates liver cirrhosis, which commonly precedes hepatic malignancies. Furthermore, obesity-associated nonalcoholic fatty liver disease (NAFLD) increasingly contributes to liver cancer incidence. With urbanization and shifts toward Western dietary habits in Hong Kong, obesity-related Hepatocellular Carcinoma rates have surged, becoming a serious public health concern.
Metabolic Dependencies & Vulnerabilities
Cancer cell metabolism signifies vital therapeutic targets for Hepatocellular Carcinoma. Tumor cells exhibit a marked dependence on glucose and glutamine metabolism. An estimated 50% of cancer cells rely predominantly on glutamine for their nucleotide synthesis and energy demands, presenting unique metabolic vulnerabilities to innovative treatments like HK Metabolic Therapy aimed at disrupting tumor survival pathways.
Asian-Specific Risks & Prevalence Data
Asian populations, particularly within Hong Kong and surrounding geographies, exhibit region-specific risk factors influencing Hepatocellular Carcinoma prevalence rates. The high prevalence of hepatitis B, augmented by genetic susceptibility, lifestyle adjustments, and increased environmental toxin exposure (aflatoxin), marks Hong Kong as a regional hotspot for Hepatocellular Carcinoma.
Encouraging Early Screening & Prevention Measures
Proactive and early screening programs substantially decrease the risk and improve treatment outcomes in Hepatocellular Carcinoma management. Regular ultrasound scans and alpha-fetoprotein (AFP) level checks are recommended for high-risk groups, particularly those with chronic hepatitis or liver cirrhosis history. Early identification can vastly enhance survival rates and treatment response.
Discover comprehensive guidelines on Hepatocellular Carcinoma prevention and screening methodology through authoritative sources like WHO and the National Cancer Institute.
Explore how groundbreaking HK Metabolic Therapy enables innovative, patient-centered treatments transforming liver cancer prognosis. Book your consultation today.
Symptoms of Hepatocellular Carcinoma (Liver Cancer)
Recognizing the symptoms of Hepatocellular Carcinoma (Liver Cancer) early can significantly improve treatment outcomes. Early stage symptoms often present subtly, and patients may initially mistake them for general illnesses or aging effects. However, as the cancer progresses, clear signs related directly to impaired liver function emerge and demand immediate medical attention.
Early-stage symptoms of Hepatocellular Carcinoma (Liver Cancer)
- Unexplained weight loss and appetite reduction
- Mild right upper quadrant abdominal discomfort
- Tiredness or persistent fatigue without clear cause
- Mild jaundice (yellowing of eyes and skin), though rare initially
Advanced-stage symptoms of Hepatocellular Carcinoma (Liver Cancer)
- Noticeable abdominal swelling, due to fluid accumulation (ascites)
- Significant jaundice and itchy skin (pruritus)
- Upper abdominal pain, radiating to right shoulder or back
- Persistent nausea or vomiting
- Pale stools and dark-colored urine
- Unexplained fever, particularly persistent or recurrent
- Easy bruising or bleeding, reflecting impaired liver function
These symptoms often correspond biologically with impaired hepatic functionality and tumor growth obstructing normal hepatocyte activities. For instance, jaundice typically occurs due to tumor blockage of bile ducts or impaired liver metabolism. Abdominal swelling results directly from impaired liver blood flow (portal hypertension) causing fluid build-up around abdominal organs.
Prompt medical evaluation upon noticing such symptoms can greatly improve prognosis, making intervention highly effective and efficient. Don’t delay seeking help. Early detection is key to successful outcomes.
Stages of Hepatocellular Carcinoma (Liver Cancer) and Survival Rates
Understanding the stages of Hepatocellular Carcinoma (Liver Cancer) assists patients, caregivers, and medical teams in making informed decisions regarding treatment strategies tailored individually for best outcomes. Here we explore specific disease stages, prevalent treatments, and survival rates often observed in Hong Kong and Asian medical contexts:
Stage 1: Early-Stage Hepatocellular Carcinoma (Liver Cancer)
Stage 1 characterizes very localized disease limited strictly within liver tissue:
- A single tumor smaller than 2 centimeters in diameter, entirely confined to liver parenchyma.
- No spread to regional lymph nodes or distant organs.
- Liver function typically remains normal or mildly compromised.
At this initial stage, surgical resection, radiofrequency ablation (RFA), or stereotactic body radiotherapy (SBRT) are highly effective treatments. Currently, outcomes in Hong Kong and major Asian oncology centers reflect survival exceeding 70% five-year rates, highlighting tremendous benefits of early detection.
Stage 2: Intermediate Hepatocellular Carcinoma (Liver Cancer)
Marked by increased tumor size and potential liver-based progression, Stage 2 exhibits following characteristics:
- Single tumor exceeding 2 centimeters, but restricted within liver tissue without regional or distant spread, or multiple small tumors still localized within liver tissues.
- Liver function moderately impaired but patient relatively stable overall.
- Surgical removal remains favorable when liver functionality permits; alternatively, minimally invasive procedures like radiofrequency ablation become optimal.
Five-year survival rates usually fluctuate between 50% to 60% across major hospitals in Hong Kong and prominent Asian oncology facilities, influenced by specific patient conditions and treatment responsiveness.
Stage 3: Advanced Regional Hepatocellular Carcinoma (Liver Cancer)
Disease progression involves regional tissue spread but still remains without distant metastatic dissemination:
- Tumor has begun to invade local blood vessels, hepatic veins, or nearby anatomical structures.
- Regional lymph node involvement may or may not be present.
- Clinical evidence often involves severely compromised liver functionality, impacting treatment eligibility.
Treatment at this stage commonly involves multimodal therapies including targeted therapy (sorafenib, lenvatinib), external beam radiation, and selective internal radiation therapy (SIRT), tailoring approaches according to patient tolerance. With integrated multimodal treatments, 5-year survival rates commonly approach 30% to 40% regionally, reflecting ongoing advancements and providing substantial hope.
Stage 4: Metastatic Hepatocellular Carcinoma (Liver Cancer)
Stage IV represents the advanced metastatic condition, indicating tumor spread beyond the liver into distant regions:
- Distant metastases to lungs, bones, brain, or abdominal organs.
- Multiple large tumors extensively diffuse throughout liver tissue.
- Severely compromised liver and overall systemic functionality, significantly impacting quality of life.
Managing metastatic liver cancer effectively incorporates systemic therapies such as immune checkpoint inhibitors, targeted agents, personalized chemotherapy regimens, advanced metabolic therapies (utilizing Nobel-recognized Warburg principle interventions), and comprehensive supportive care. Although curative interventions remain challenging at Stage 4, emerging research and discoveries in metabolic oncology continue demonstrating improvements in chronic disease management and long-term survival potential. Average three-year survival rates currently range approximately between 10% to 25% in highly specialized Asian oncology treatment centers, reflecting continual advancement in treatment methods and chronic disease management goals set for 2025.
It’s crucial to understand that survival statistics offer general insights. Each patient’s treatment response varies significantly based on overall health, genetic factors, disease burden, and therapy selection. Innovations from Nobel laureates such as Professors Semenza and Allison inspire ongoing breakthroughs, providing compelling hope to manage Hepatocellular Carcinoma chronically beyond predicted survival periods.
Taking immediate action towards understanding your specific case through advanced diagnostics helps in crafting personalized, effective treatments. Remember, every step towards timely intervention substantially increases the opportunity to transform Hepatocellular Carcinoma (Liver Cancer) into a chronic, manageable condition. Consider scheduling your consultation today for detailed evaluation and tailored care strategies.
Limitations of Traditional Therapies for Hepatocellular Carcinoma (Liver Cancer)
Chemotherapy’s Limited Efficacy and High Toxicity in Hepatocellular Carcinoma (Liver Cancer)
Chemotherapy remains one of the traditionally used treatments for Hepatocellular Carcinoma (Liver Cancer). However, this method has considerable drawbacks. Notably, clinical data have consistently shown relatively poor efficacy in advanced stages, often failing to achieve substantial tumor shrinkage. For example, the objective response rate (ORR) of chemotherapy for patients with advanced or metastatic Hepatocellular Carcinoma is less than 21%. This limited success translates into reduced overall survival and prolonged suffering for affected individuals.
Moreover, chemotherapy regimens frequently induce significant toxicities, severely impairing quality of life. Common adverse drug effects observed in Hong Kong oncology clinics include:
- Severe bone marrow suppression (78%), leading to increased susceptibility to severe infections
- Cardiac toxicity (23%), significantly elevating cardiovascular morbidity risks
- Fatigue and profound weakness, drastically impacting daily living activities and emotional well-being
- Persistent nausea and vomiting, requiring additional supportive medications
- Neurological impairments such as peripheral neuropathy affecting sensory and motor functions, reducing patients’ quality of life considerably
Ultimately, these challenges highlight the pressing need for more refined, less damaging therapies, especially in advanced cases commonly observed across Asia, including in Hong Kong.
Radiation Therapy and Associated Limitations for Liver Cancer Treatment
Radiation therapy (RT), although widely utilized to manage various cancer types, confronts inherent limitations when applied to Hepatocellular Carcinoma (Liver Cancer). Radiation’s destructive capability is not exclusive to cancer cells but also damages surrounding healthy tissues and vital liver structures, exacerbating organ dysfunction. The liver is especially vulnerable, given its crucial functional roles like detoxification, metabolism, and protein synthesis.
Radiation-induced complications frequently encountered include:
- Permanent liver tissue damage and fibrosis, potentially leading to progressively decreasing liver function and liver failure
- Radiation hepatitis characterized by significant increases in liver enzymes and jaundice
- Alarming rates of gastrointestinal toxicity, including ulceration or uncontrollable gastrointestinal bleeding, further complicating patient management strategies
- Fatigue, anorexia, and weight loss resulting from compromised liver function and reduced nutrient absorption
In further concern, radiation-induced secondary malignancies or cancer recurrence after treatment can emerge at much higher rates, with recent studies published in JAMA Oncology (2023) demonstrating that RT increases secondary cancer risk substantially by up to three-fold compared to non-irradiated patients.
Surgical Risks and Considerations in Hepatocellular Carcinoma (Liver Cancer)
Surgical intervention, including hepatectomy or partial liver resection, is a cornerstone of standard therapy for Hepatocellular Carcinoma. Nonetheless, procedures involve inherent risks, especially significant in patients with compromised liver function, prevalent in Asia owing to high chronic hepatitis B infection rates and cirrhosis prevalence.
Specific risks attributed widely to surgical interventions include:
- Postoperative infections, occurring frequently in patients as immunocompromised states associated with chronic liver disorders create ideal conditions for pathogens
- Severe bleeding complications during surgery, potentially necessitating blood transfusions and extended hospitalization periods
- Liver failure post-surgery due to reduced hepatic reserve capacity, significantly elevating mortality rates
- Risk of recurrence remains alarmingly high, affecting as many as 50%-70% of patients within 5 years post-operation
Such operative complications underline an urgent need to develop effective and minimally invasive interventions, particularly beneficial for populations burdened heavily with liver-associated disorders, such as those in Hong Kong and neighboring Asian regions.
Metabolic Resistance Mechanisms Complicating Conventional Treatment Approaches
An underestimated aspect hampering treatment success in Hepatocellular Carcinoma is the inherent metabolic resistance mechanisms typical of cancer cells. Liver cancer cells frequently exhibit metabolic flexibility, substantially altering their glucose and glutamine metabolism pathways to survive harsh therapeutic environments induced by chemotherapy and radiation.
With an enhancing propensity, findings indicate that cancer cells in Hepatocellular Carcinoma notably exhibit:
- A significantly increased glycolytic rate, known as the Warburg effect, making them metabolically robust (cancer cells consume glucose up to 200 times faster compared to normal cells)
- Elevations exceeding 400% in DNA repair enzyme activity post-chemotherapy or radiotherapy administration, facilitating rapid cellular recovery and resistance to therapeutic approaches
- Highly effective antioxidant generation capacities, allowing advanced cancer cells to neutralize oxidative stresses induced by conventional therapies, thus heightening resistance and survival mechanisms
Such metabolic adaptability significantly thwarts therapeutic effectiveness, emphasizing the critical requirement for novel interventions targeting cancer cells’ distinctive metabolic vulnerabilities effectively, which traditional treatments often overlook.
Overcoming Limitations: Emerging Therapeutic Pathways in Hepatocellular Carcinoma (Liver Cancer)
Recognizing traditional therapeutic limitations, significant strides have been made towards innovative, precision-based treatments targeting specific molecular vulnerabilities within cancer cells. Advances in fields like metabolic oncology, immunotherapy endorsed by Nobel laureates Allison and Semenza, and novel multi-modal integrated therapies present appealing new solutions to address traditional therapy constraints effectively.
As the Asia-Pacific region continues to experience disproportionately higher incidences of liver cancer, pioneering centers (e.g., collaborating institutes like Shenzhen Qianhai Taikang and MD Anderson) endeavor to evolve treatments aligned with the “Cure First, Pay Later” policy, ensuring patient-centric innovations significantly improving outcomes.
In conclusion, given the explicit therapeutic challenges faced by conventional chemotherapy, radiation, and surgical interventions, embracing innovative solutions addressing Hepatocellular Carcinoma’s metabolic peculiarities provides a promising, less toxic, and potentially more effective route for transforming this lethal cancer into a manageable chronic condition, one of AllCancer’s ambitious therapeutic goals by 2025.