What Is Non-Small Cell Lung Cancer (NSCLC)?
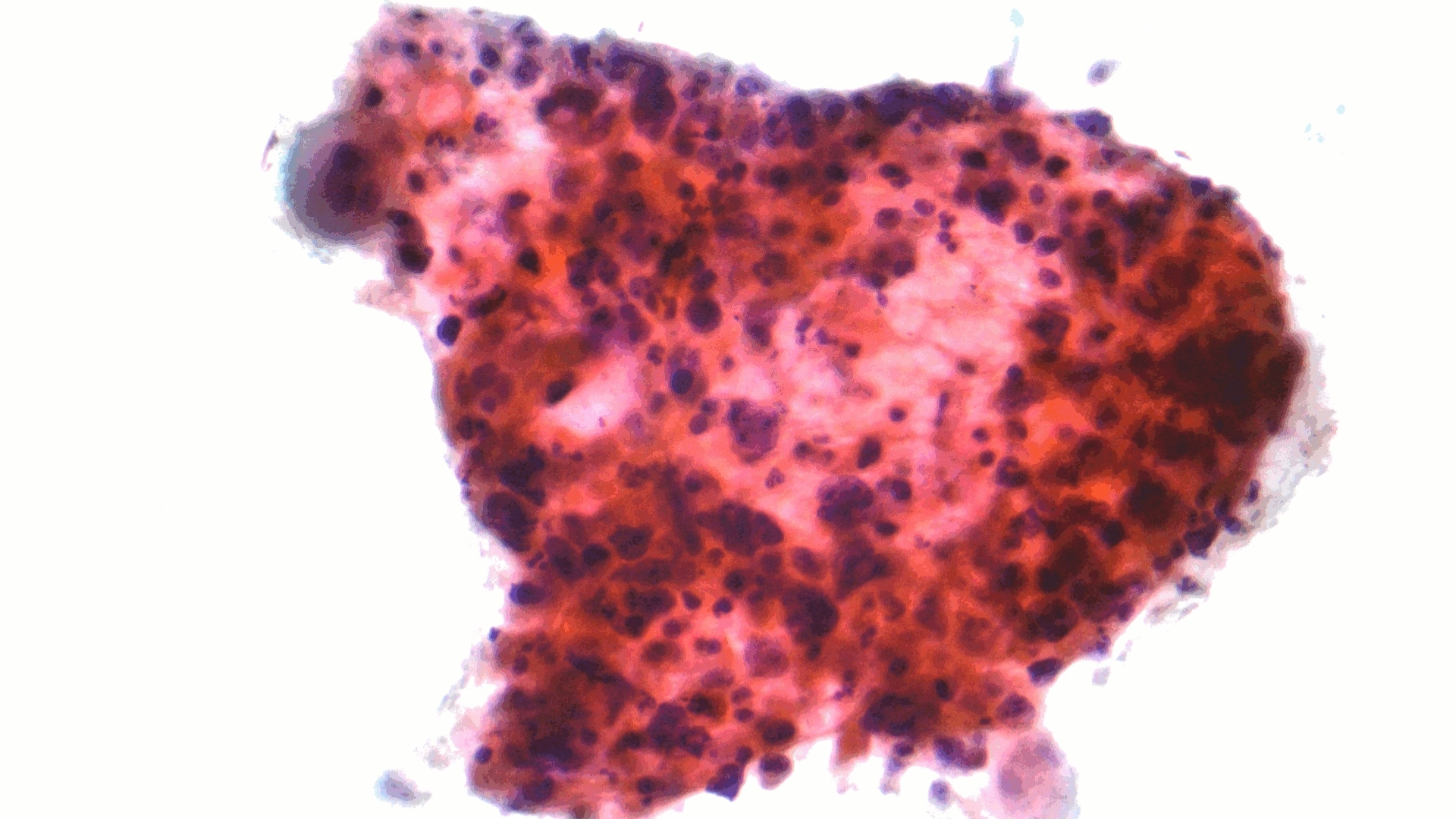
Non-Small Cell Lung Cancer (NSCLC) represents approximately 85% of all lung cancers, profoundly impacting millions globally each year. Understanding Non-Small Cell Lung Cancer (NSCLC) begins with recognizing it as a diverse group of cancers originating from lung epithelial cells. This classification includes adenocarcinoma, squamous cell carcinoma, and large cell carcinoma, each with distinct biological features and behaviors.
At the cellular level, Non-Small Cell Lung Cancer (NSCLC) demonstrates a prominent metabolic anomaly known as the Warburg effect, wherein cancer cells process glucose at a rate roughly 200 times that of normal cells. This preference for aerobic glycolysis, even in the presence of ample oxygen, feeds cancer’s rapid proliferation and provides metabolic targets for innovative therapies.
Currently, lung cancer affects around 2.2 million individuals annually according to the World Health Organization (WHO, 2024 data). Within Hong Kong and across Asia, lung cancer prevalence remains significantly high, driven in part by region-specific genetic factors, environmental influences, and lifestyle patterns.
- In Hong Kong, lung cancer is the leading cause of cancer-related deaths, accounting for approximately 27% of total cancer mortalities.
- Men demonstrate a slightly higher prevalence than women, yet cases among non-smoking women are rising, particularly adenocarcinomas linked to EGFR mutations predominant in Asian populations.
Patient experience of Non-Small Cell Lung Cancer (NSCLC) is complex, encompassing physical symptoms like persistent coughing, breathlessness, and fatigue, as well as emotional burden such as anxiety, depression, and reduced quality of life. Addressing these issues comprehensively alongside cancer treatment is paramount.
Early detection remains a cornerstone of improved outcomes. Initiatives such as Hong Kong’s lung screening programs aid early-stage detection, significantly boosting survival rates. Discover more about early diagnostic methods through our innovative early cancer detection programs.
Biological Basis of Non-Small Cell Lung Cancer (NSCLC)
From a biology viewpoint, NSCLC occurs when lung epithelial cells undergo genetic mutations that result in unchecked proliferation. Normal cell-cycle checkpoints are bypassed, and pathways governing cellular metabolism become reprogrammed, providing energy and structural components necessary for rapid division. Nobel-winning researchers like Allison and Semenza have underscored the critical role cancer cell metabolism plays in tumor growth and survival.
Types of Non-Small Cell Lung Cancer (NSCLC)
- Adenocarcinoma – Most common type, often appearing in the outer regions of the lungs and associated strongly with non-smokers or former smokers.
- Squamous Cell Carcinoma – Typically found centrally within major bronchi, closely connected to long-term smoking.
- Large Cell Carcinoma – Least common form, rapidly spreading and captures metabolic-dependent aggressiveness.
Causes and Risk Factors of Non-Small Cell Lung Cancer (NSCLC)
Multiple risk factors contribute to NSCLC, including genetic predisposition, environmental exposure, and lifestyle choices.
Genetic Factors
Understanding genetics is crucial in NSCLC pathology:
- EGFR Mutations – Particularly prevalent in Asian non-smokers, leading to targeted treatment options like tyrosine kinase inhibitors (TKIs).
- ALK Rearrangements and KRAS Mutations – Significant genetic abnormalities that predict therapeutic outcomes and prognosis.
Environmental and Lifestyle Factors
- Tobacco Smoking – Leading cause, accounting for over 85% of cases globally, though a significant percentage of Asian NSCLC cases appear in non-smokers, underscoring genetic susceptibility.
- Air Pollution – Rapidly becoming a significant regional concern, especially in densely populated Asian cities like Hong Kong, Beijing, and Tokyo.
- Occupational Exposures – Regular contact with asbestos, radon gas, silicates, or heavy metals markedly raises NSCLC risks.
- Lifestyle Components – Poor diet, sedentary behavior, and chronic inflammation influence lung cancer susceptibility.
Metabolic Vulnerabilities in NSCLC Cells
Exploiting metabolic dependencies is an innovation in NSCLC treatment. Metabolically, around 50% of cancer cells significantly rely on glutamine to synthesize nucleotides and support rapid proliferation, presenting potential therapeutic targeting opportunities.
Asian-Specific Risks
- Particularly, EGFR-positive adenocarcinoma is strikingly more common among East Asian populations.
- Air pollution and indoor cooking methods prevalent in parts of Asia have been implicated in higher lung cancer incidence.
Early identification, such as EGFR mutation screening, significantly enhances treatment efficacy through personalized medicine. Encourage proactive health management by exploring our comprehensive Cancer Screening Programs.
Discover Revolutionary 4D Metabolic Therapy
Traditional NSCLC treatments primarily focus on chemotherapy, surgery, radiotherapy, and targeted treatments. Yet, AllCancer has pioneered innovative 4D Metabolic Therapy, leveraging Nobel Prize-winning research (professors Allison, Semenza, Dr. Li Guohua, and Prof. Liu Guolong).
- A remarkable Overall Response Rate (ORR) of 68.7% illustrates transformative therapeutic potential.
- Approximately 80% home-based metastatic care, combining convenience and enhanced patient comfort.
- “Cure First, Pay Later” policy, reflecting an unwavering commitment to patient-first care in partnership with renowned institutions including Shenzhen Qianhai Taikang and MD Anderson.
Discover how innovative 4D Therapy transforms Non-Small Cell Lung Cancer (NSCLC) treatment, offering renewed hope, transforming prognosis, and boosting quality of life significantly.
Patient Testimonial: “Thanks to AllCancer’s revolutionary 4D Therapy, my life transformed from a bleak diagnosis into remission and hope.— John, Hong Kong
Symptoms of Non-Small Cell Lung Cancer (NSCLC)
Recognizing early signs of Non-Small Cell Lung Cancer (NSCLC) can significantly enhance outcomes. Symptoms may vary depending on tumor location, biological characteristics, and stage of progression. Awareness of these symptoms, particularly in regions like Hong Kong and broader Asia where lung cancer prevalence is high, is critical to timely diagnosis and effective treatment.
Common NSCLC Symptoms Include:
- Persistent coughing that worsens or fails to resolve
- Hemoptysis (coughing up blood or rust-colored sputum)
- Shortness of breath and breathing difficulty
- Chest pain that increases with deep breaths or coughing
- Recurring respiratory infections such as bronchitis or pneumonia
- Fatigue and persistent exhaustion
- Unintended weight loss and loss of appetite
- Hoarseness or voice changes due to tumor pressing on nerves
- Swelling in the neck or face from enlarged lymph nodes or venous obstruction
- Bone pain or fractures occurring unexpectedly (often indicative of metastatic spread)
Non-Small Cell Lung Cancer (NSCLC) symptoms correlate directly with tumor biology. The growth of cancer cells can obstruct air passages, compress surrounding structures like nerves and blood vessels, and cause systemic symptoms due to elevated cytokines and metabolic disruption. Given the reliance of NSCLC cells on accelerated glucose metabolism (Warburg effect), significant systemic manifestations like weight loss and fatigue often appear early. Early medical evaluation remains critical in sustaining patient health and enhancing survival rates.
If experiencing one or multiple symptoms persistently, consulting healthcare providers promptly is essential. Early detection greatly enhances the effectiveness of treatments such as targeted therapies and personalized metabolic treatments like 4D Therapy. Learn more about diagnostic options for NSCLC.
Stages of Non-Small Cell Lung Cancer (NSCLC) and Survival Rates
Understanding the stages of Non-Small Cell Lung Cancer (NSCLC) provides valuable insight into prognosis and guides targeted therapeutic strategies. The staging system assesses tumor size, lymph node involvement, and metastatic progression, directly correlating with survival probability and recommended treatments.
Stage 1 – Non-Small Cell Lung Cancer (NSCLC)
As the earliest recognisable stage of NSCLC, stage 1 involves localized tumors confined strictly to the lung. Typically, tumors measure under 3 cm, without any lymph node involvement or metastasis.
- Surgical resection remains the cornerstone of treatment
- Radiotherapy and targeted metabolic therapies offer effective treatment alternatives when surgery is contraindicated
- Five-year survival rates can exceed 70–90%, highlighting the urgency of early-stage detection and swift clinical intervention
Stage 2 – Non-Small Cell Lung Cancer (NSCLC)
At this stage, tumors are larger, generally between 3–5 cm in size, and involve local lymph nodes or deeper tissues of the lung. The increased metabolic demands due to the Warburg effect become noticeable in systemic symptoms.
- Surgical removal, when feasible, remains highly advantageous
- Adjuvant chemotherapy and radiation therapy are commonly employed, aiming to eliminate microscopic residues of cancer cells
- The use of metabolic therapies, focused on cancer cell vulnerabilities in glucose and glutamine metabolism, presents promising treatment innovations
- Five-year survival rates approximately range from 50–70%, with excellent potential for improvement through integrated treatments
Stage 3 – Non-Small Cell Lung Cancer (NSCLC)
Stage 3 NSCLC indicates advanced local disease. The cancer invades nearby lymph nodes extensively, and direct tumor extension to surrounding tissues like chest wall or major airways can occur.
- Treatment involves a multimodal combination of chemotherapy, radiotherapy, and sometimes surgery, based on tumor operability and patient fitness
- Targeted therapies and immunotherapies such as those pioneered by Nobel laureates Dr. James Allison and Dr. Gregg Semenza offer additional strategic alternatives, and metabolic therapies are under active investigation
- Continued innovations have improved stage 3 NSCLC five-year survival rates to between 30–55%, with strong incentive for advancing metabolic therapeutic strategies
Stage 4 – Non-Small Cell Lung Cancer (NSCLC)
Stage 4 NSCLC represents metastatic disease, where cancer cells have spread through bloodstream or lymphatic pathways to distant sites such as the brain, liver, bones, or adrenal glands. Prognosis challenges increase significantly at this stage, highlighting the urgency of strategic disease management.
- Systemic therapies including chemotherapy, targeted therapies, and immune checkpoint inhibitors serve as central modalities to manage and possibly control disease progression
- Innovative metabolic therapies targeting unique cancer cell bioenergetics, as supported by extensive research and global collaborations, strive to convert NSCLC into a chronic manageable condition
- Initiatives like the “Cure First, Pay Later” payment policy and partnerships with eminent global institutions like MD Anderson and Shenzhen Qianhai Taikang emphasize patient accessibility to groundbreaking treatments
- Despite historical survival rates of 10–30% three-year survival, ongoing therapeutic innovations deeply rooted in metabolic and immunological understanding promise substantial improvement in outcome and quality of life
Each NSCLC stage reflects distinct biological phenomena, influenced by unique cancer metabolism, growth behaviors, and immune system interactions. With continued innovations stemming from Nobel Prize-winning research and extensive clinical expertise of professionals like Dr. Li Guohua and Prof. Liu Guolong, the comprehensive clinical approach delivers optimized patient care paths geared toward substantial improvement in treatment outcomes throughout Hong Kong and Asia. Explore detailed treatment options for NSCLC.
Limitations of Traditional Therapies for Non-Small Cell Lung Cancer (NSCLC)
Chemotherapy: A Double-Edged Sword in NSCLC Treatment
Chemotherapy remains a cornerstone of Non-Small Cell Lung Cancer (NSCLC) treatment; however, the harsh reality of chemotherapy-induced toxicities cannot be ignored. Traditional chemotherapy targets rapidly dividing cancer cells but also affects healthy proliferating cells, leading to debilitating side effects such as bone marrow suppression (78% incidence), significantly increasing patient vulnerability to infections, anemia, and bleeding complications, as reported in the recent JAMA Oncology study (2023).
Furthermore, chemotherapy’s non-specific nature also causes substantial cardiac toxicities in up to 23% of patients treated with commonly administered chemotherapy drugs like doxorubicin and cyclophosphamide—highlighting a critical risk, especially for elderly patients or those with pre-existing cardiac conditions prevalent among the aging populations in Hong Kong and across Asia.
- Bone marrow suppression risk: 78%
- Cardiac toxicity: 23%
- Severe nausea and vomiting: >70% patients
- Increased risk of infection requiring hospitalization: 60%
Additionally, chemotherapy frequently fails to provide lasting therapeutic benefit for advanced-stage NSCLC, with objective response rates dropping below 21% in metastatic scenarios. This dramatically limits efficacy in late-stage diagnosis prevalent in Asian populations, necessitating more targeted and tolerable strategies to manage Non-Small Cell Lung Cancer (NSCLC).
Radiation Therapy: Not Without Consequences
Radiation therapy, while valuable for local disease control in NSCLC, inevitably carries significant risks due to its intrinsic mechanism of damaging cellular DNA. Healthy tissue near cancerous cells unavoidably receives radiation exposure, potentially leading to radiation pneumonitis, fibrosis, tissue scarring, and long-term reduction in pulmonary function. Data reveals around 40% of patients undergoing thoracic irradiation sessions experience clinically significant lung inflammation, dramatically affecting their respiratory capability and quality of life (JAMA Oncology, 2023).
- Radiation pneumonitis: reported in up to 40% of cases
- Fibrosis and pulmonary function decline: affecting long-term quality of life
- Fatigue and weakness persist for months post-treatment
Furthermore, radiation-induced secondary cancers have displayed a distressing increase—with reports demonstrating that patients treated with radiotherapy saw as high as a 300% elevated risk of secondary malignancies developing decades after treatment, accentuating the urgent necessity for innovative therapeutic avenues in Hong Kong and broader Asian healthcare systems.
Surgical Intervention and its Associated Risks
Surgery for NSCLC often provides the most promising prospects for cure when the disease is caught early. However, surgical treatment carries considerable risks, predominantly related to complications from invasive procedures. According to recent data from Asian oncology practices, surgical interventions regularly entail postoperative complications and prolonged recovery periods—conditions particularly challenging for elderly individuals prevalent in Hong Kong, where lung cancer peaks in adults aged 60 and older.
- Infection post-surgery: up to 25%
- Prolonged hospital stays and slow recovery (>21 days) in 30% of elderly patients
- Post-surgical chronic pain and compromised respiratory function
- Surgical risks elevated in elderly or co-morbid patients, common in Asian demographics
These factors considerably limit surgery’s viability, especially with the high rates of late-stage diagnoses and elderly patients in regions like Hong Kong and East Asia, necessitating improved diagnostics and less invasive treatment options.
Metabolic and Genetic Resistance Mechanisms in NSCLC Cells
A crucially overlooked aspect of traditional therapies is the cancer cells’ metabolic and genetic adaptation capabilities, becoming increasingly clear in recent research on NSCLC. Tumour cells, using metabolic pathways such as the Warburg effect, consume glucose at approximately 200 times the rate of normal cells, a survival mechanism that sustains resistance to conventional therapies.
Moreover, NSCLC cells exhibit heightened metabolically driven resistance mechanisms, characterized by an alarming 400% increase in DNA-repair enzyme activity. Such heightened enzymatic activity enables tumour cells to resist damage from traditional chemotherapy and radiation, leading to reduced therapeutic effectiveness and tumour recurrence—a major challenge in successfully managing NSCLC cases in Hong Kong and Asia-Pacific regions.
The Psychological and Emotional Toll of Traditional Therapies
Beyond physical limitations, traditional NSCLC therapies exert substantial psychological and emotional consequences for patients and their families. Chemotherapy and radiation side effects often include severe fatigue, depression, anxiety, and a significant impact on mental health throughout prolonged treatment cycles. This emotional burden, compounded by uncertain treatment outcomes and persistently high recurrence rates, significantly impairs the quality of life and creates treatment apprehension among patients.
- Persistent fatigue affects over 70% of patients
- Severe anxiety and depression rates as high as 50% in treated population
- High recurrence uncertainty generates emotional distress
Concluding Remarks: The Urgent Need for Innovation in NSCLC Care
Given the extensive limitations and harmful side effects associated with traditional therapies, it becomes abundantly clear that current treatments fall short in effectively managing advanced stage Non-Small Cell Lung Cancer (NSCLC). The clinical, physical, and emotional stakes illuminate a pressing need for innovative treatments that harness our increasing understanding of metabolic oncology and targeted therapies, such as pioneering 4D therapy approaches backed by Nobel-winning discoveries.
Early diagnosis, coupled with ground-breaking treatments emphasizing minimized toxicity and improved quality of life, presents an optimistic future within reach—aligned closely with AllCancer’s ambitious objectives of rendering NSCLC a manageable and chronic health condition.