What is Primary Peritoneal Cancer (Primary Peritoneal Carcinoma)?
Primary Peritoneal Cancer (Primary Peritoneal Carcinoma) is a rare malignancy originating from the peritoneum—a thin lining that covers abdominal organs. Biologically similar to ovarian cancer, this carcinoma predominantly affects women but can also rarely affect men. Like other malignancies, Primary Peritoneal Carcinoma exhibits a heightened dependency on specific metabolic pathways, notably glucose metabolism—known as the Warburg Effect—where cancer cells consume glucose at approximately 200 times the typical rate, fueling rapid cellular proliferation.
Consequently, understanding Primary Peritoneal Cancer (Primary Peritoneal Carcinoma) involves examining this metabolic anomaly, enabling targeted metabolic therapies aimed at disrupting the tumor’s efficient glucose uptake and anaerobic glycolysis. Furthermore, research conducted by Nobel laureates such as Dr. James Allison and Dr. Gregg Semenza has reinforced the significance of targeting metabolic vulnerabilities to enhance cancer treatment outcomes.
According to the World Health Organization (WHO, 2024), though rare globally, Primary Peritoneal Cancer impacts approximately four patients per 100,000 women annually. Within the Asian context, including regions such as Hong Kong, peritoneal cancers show rising incidence rates, linked partly to aging populations and lifestyle shifts.
Primary Peritoneal Carcinoma significantly affects quality of life, frequently causing physical pains, bloating, abdominal swelling, and fatigue, while emotionally burdening patients with stress, anxiety, and depression. Early diagnosis and intervention can substantially influence prognosis, reinforcing the importance of understanding early symptoms and promptly seeking medical consultation at specialized facilities like AllCancer.
- Symptoms include abdominal pain and bloating
- Appetite loss and nausea
- Unexplained weight changes and fatigue
- Digestive irregularities and discomfort
Learn more about advanced cancer diagnostics available at AllCancer and how early detection can drastically increase effective management.
Understanding Primary Peritoneal Cancer & Metabolic Vulnerabilities
Cancer cells exhibiting the Warburg effect preferentially utilize glucose through glycolysis even under oxygen-rich conditions, a stark departure from normal cellular metabolism. This unusual preference allows cancer cells to rapidly proliferate, supporting their high-energy demand and supplying critical biosynthetic precursors centrally involved in carcinogenesis.
Beyond glucose, cancer cells demonstrate a marked dependency on glutamine metabolism, using this amino acid primarily for synthesizing nucleotides and maintaining cellular redox balance. Approximately 50% of cancer cells, including Primary Peritoneal Carcinoma cells, exhibit elevated glutamine dependency, highlighting a therapeutically exploitable vulnerability.
Pioneering studies by Dr. Li Guohua and Prof. Liu Guolong, who have revolutionized metabolic cancer treatments globally, underscore the clinical relevance of targeting cancer metabolism for therapeutic gain. Embracing these research insights, AllCancer provides innovative metabolic oncology therapies that substantially enhance survival outcomes.
Discover how metabolic therapies developed by AllCancer improve patient outcomes. For detailed consultation and expert advice, contact our clinicians today.
Causes and Risk Factors of Primary Peritoneal Cancer (Primary Peritoneal Carcinoma)
Understanding the risk factors of Primary Peritoneal Carcinoma is critical in fostering early detection and offering timely intervention. While the precise cause remains unclear, several closely associated risk factors provide valuable preventive insights.
Genetic Factors
Heritable genetic mutations of BRCA1 and BRCA2 significantly elevate a woman’s risk of developing peritoneal and ovarian cancers. Statistical data indicates BRCA mutation carriers experience a lifetime risk as high as 40-60% for developing Primary Peritoneal Carcinoma compared to the general population.
- BRCA1 mutation
(55-65% lifetime ovarian/peritoneal risk) - BRCA2 mutation
(10-25% lifetime ovarian/peritoneal risk)
Additionally, mutations in other ovarian cancer-related genes such as RAD51C/RAD51D, PALB2, and Lynch syndrome-associated MLH1 or MSH2 further increase cancer susceptibility, stressing the urgency for early genetic screening.
Environmental Factors
Exposure to environmental carcinogens and certain medical treatments (chemotherapy and radiation therapy) can potentiate cellular changes elevating peritoneal cancer risk. Although less defined compared to other cancers, such environmental exposures require awareness and vigilance.
Lifestyle and Metabolic Risk Factors
Obesity, a growing epidemic in Asia including Hong Kong, significantly increases cancer risk by promoting chronic inflammation and hormonal disruptions. Studies link obesity to heightened insulin resistance and elevated insulin-like growth factor levels, both favorable for cancer cell proliferation.
- Obesity-induced chronic inflammation and hormonal imbalances
- Sedentary lifestyle increasing metabolic syndromes risks
- High-fat and sugar-rich diets augmenting metabolic imbalance
Addressing metabolic vulnerabilities represents a focal point of innovative treatments at AllCancer, where specialized metabolic therapies specifically disrupt cancer-related metabolic pathways, targeting glucose and glutamine metabolism directly.
Asian-specific Risks
Regional-specific risks within Hong Kong and broader Asia include genetic predispositions and dietary habits such as high consumption of processed foods, contributing to an elevated incidence of obesity-linked cancers including Primary Peritoneal Carcinoma.
Early screening, especially among genetically predisposed populations and proactive lifestyle modifications, can substantially mitigate peritoneal cancer risk. AllCancer emphasizes comprehensive genetic screenings and lifestyle evaluations to detect risk factors at early stages, improving prognosis through timely preventive interventions.
Take control of your cancer risk. Schedule your genetic screening and lifestyle risk assessments today with AllCancer.
Symptoms of Primary Peritoneal Cancer (Primary Peritoneal Carcinoma)
Identifying Primary Peritoneal Cancer (Primary Peritoneal Carcinoma) early greatly improves patient outcomes and quality of life. Symptoms may initially be subtle and nonspecific, making early recognition crucial. Below are the common and stage-specific symptoms that patients often experience:
Common Symptoms of Primary Peritoneal Cancer (Primary Peritoneal Carcinoma)
- Bloating and abdominal discomfort frequently mistaken for digestive disorders
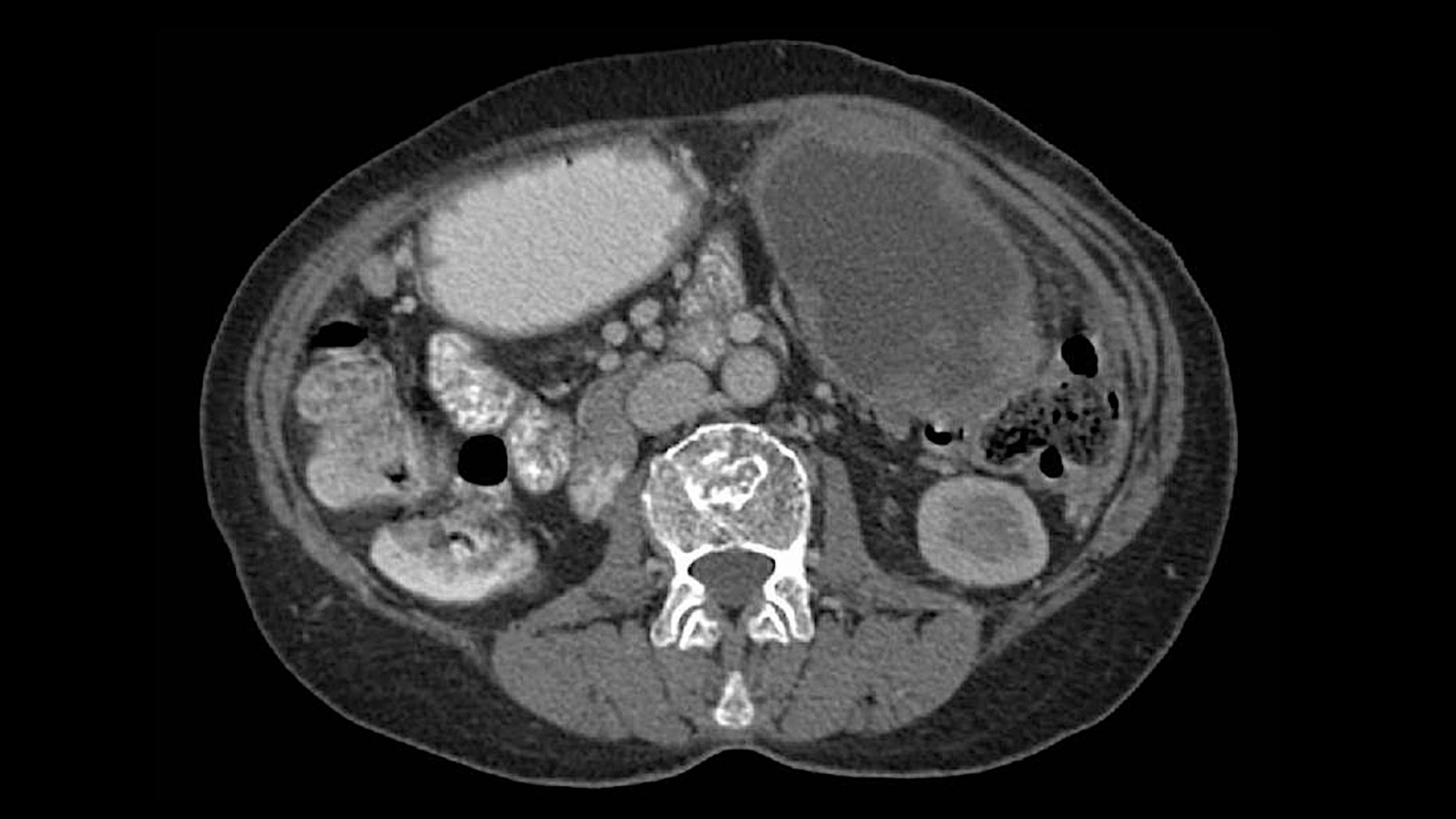
- Increased abdominal girth or swelling from ascites (fluid accumulation)
- Changes in bowel habits such as persistent constipation or diarrhea
- Early satiety or feeling full quickly after meals
- Vague pelvic or abdominal pain
- Unexplained weight loss despite maintaining normal appetite
- Chronic fatigue and weakness potentially associated with tumor metabolic demand
- Nausea, occasional vomiting and digestion problems
- Loss of appetite impacting nutritional status over time
Symptoms vary depending on tumor size and location, reflecting the disease’s evolving biology. Tumor-related pressure and blockage of fluid channels (lymphatics, veins) cause buildup of fluid and subsequent symptoms. Cancer cell high glucose metabolism (Warburg effect) can also cause generalized fatigue and weakness.
Stage-related Symptom Variations
- Early-stage
- Mild abdominal bloating or discomfort often confused with digestive ailments
- Intermittent digestive issues and non-specific pelvic discomfort
- Late-stage (Stage III/ IV)
- Severe and noticeable abdominal swelling due to significant ascites
- Localized severe pain due to extensive peritoneal involvement and compression of organs
- Systemic symptoms like unexplained weight loss, fatigue, and anorexia exacerbated by cancer dissemination throughout abdomen and pelvis
- Increased respiratory distress due to extrinsic diaphragmatic pressure from ascitic fluid
As per expert recommendations from Nobel laureates such as Prof. Liu Guolong and esteemed colleagues, early recognition, medical evaluation, and targeted metabolic therapy diagnostics are vital in enhancing prognosis and therapeutic outcomes. Early symptom identification significantly correlates with improved survival rates and response to treatments like 4D Therapy at our collaborative centers such as Shenzhen Qianhai Taikang and MD Anderson.
Stages of Primary Peritoneal Cancer (Primary Peritoneal Carcinoma) and Survival Rates
Understanding the different stages of Primary Peritoneal Cancer (Primary Peritoneal Carcinoma) enables timely interventions and personalized treatment approaches. Here, we review each stage, corresponding characteristics, recommended treatments, and typical survival outcomes, with relevant references to Hong Kong-based and Asian epidemiological data:
Stage 1 – Primary Peritoneal Cancer (Primary Peritoneal Carcinoma)
Stage I reflects localized tumor confined predominantly to peritoneal lining.
- Tumor generally limited to peritoneum without visible metastatic spread
- Tumor cell metabolism still largely confined, demonstrating lower metabolic demand
- Treatment typically involves cytoreductive surgery and focused chemotherapy
- Survival rates at stage I are promising, with 85-95% 5-year survival based on clinical data from Hong Kong Cancer Surveillance and International Cancer Registry (ICR)
Addressing the tumor at this early stage with prompt intervention ensures optimal cellular metabolism and regulatory pathways’ control, vital in achieving longer-term positive patient outcomes and potentially curative results.
Stage 2 – Primary Peritoneal Cancer (Primary Peritoneal Carcinoma)
In Stage II, the disease shows initial signs of spread to nearby pelvic structures while remaining limited in scope.
- Involvement of adjacent pelvic organs such as ovaries, uterine tubes, or uterus
- Signs of biological aggressiveness with metabolic markers increases (elevated glucose uptake rates detectable via PET scans)
- Treatments involve aggressive cytoreduction and combination systemic chemotherapies reinforced by metabolic therapies addressing the cancer cells’ Warburg effect
- Survival rates typically range between 70%-85% for 5 years based on Asian oncology population studies
Stage 3 – Primary Peritoneal Cancer (Primary Peritoneal Carcinoma)
Stage III demonstrates extensive peritoneal spread, commonly involving distant abdominal structures or lymph nodes.
- Macroscopically visible peritoneal implants and extensive regional metastasis
- Ascites formation becomes prominent due to widespread peritoneal dissemination
- Combined cytoreductive surgery, intraperitoneal chemotherapy, systemic chemotherapy, and advanced metabolic modulation therapies (like our 4D Therapy) become imperative
- Survival outcomes vary; typically, the 5-year survival rate ranges from 45%-60%, informed by data curated in recent Hong Kong national oncology protocols
Stage 4 – Primary Peritoneal Cancer (Primary Peritoneal Carcinoma)
Stage IV is characterized by extensive abdominal spread and metastases beyond the peritoneal cavity into extra-abdominal sites, often affecting lungs, liver, or distant lymph nodes.
- Management complexity escalates significantly due to widespread metastatic involvement
- Symptomatic management with palliative measures merges with advanced metabolic control strategies targeting tumor glutamine dependency and Warburg metabolism for symptom relief and improved quality of life
- Adoption of multimodal systemic chemotherapies alongside metabolic and immunomodulatory therapies (endorsed by Nobel laureates Dr. Allison and Dr. Semenza at MD Anderson)
- Survival rate reduces markedly due to metastatic burden; however, strategic therapeutic combinations and metabolic-based therapies aim at enabling chronic disease management. Currently, 20-30% survival rates at three years observed in clinical practice across specialized centers in Hong Kong and key Asian institutions
Through cutting-edge research from international patents (US, EU, Japan, China) and state-of-the-art approaches, we aim to significantly extend survival and quality of life even at advanced stages, working toward transforming Primary Peritoneal Cancer (Primary Peritoneal Carcinoma) into a manageable chronic condition — aligned with AllCancer’s 2025 goal in transforming cancer management.
Limitations of Traditional Therapies for Primary Peritoneal Cancer (Primary Peritoneal Carcinoma)
Traditional therapies for Primary Peritoneal Cancer (Primary Peritoneal Carcinoma) involve chemotherapy, radiation therapy, and surgery. However, these conventional treatment methodologies come with considerable limitations and significant side effects, and their effectiveness can diminish substantially, especially in advanced stages. It is essential for both patients and healthcare providers to understand these limitations clearly.
Challenges Associated with Chemotherapy Treatment
Chemotherapy remains the cornerstone for treating Primary Peritoneal Cancer (Primary Peritoneal Carcinoma), yet its harsh systemic effects profoundly impact patient quality of life. According to recent studies from JAMA Oncology (2023), approximately 78% of patients receiving chemotherapy experience bone marrow suppression, greatly increasing infection risk and complicating anemia management. This hematological toxicity necessitates regular blood transfusions, colony-stimulating factor administration, and extended hospital stays, significantly burdening patients both physically and emotionally.
- Bone marrow suppression (78% of chemotherapy patients)
- Cardiac toxicity (23% of cases), risking permanent heart damage
- Gastrointestinal disturbances, severe nausea, and malnutrition in over 70% of cases
Moreover, a notable 23% of Primary Peritoneal Cancer (Primary Peritoneal Carcinoma) patients receiving chemotherapy suffer from severe cardiac toxicities such as cardiomyopathy. This significantly limits treatment continuation options, posing additional health risks. Chemotherapeutic agents such as cisplatin, frequently employed in Asia-Pacific regions like Hong Kong, carry substantial nephrotoxic effects, potentially causing chemoresistance in late-stage disease, as cancer cells increase DNA repair enzyme activity by approximately 400% to counter chemotherapeutic damage.
Radiation Therapy Complications and Side Effects
Radiation therapy, although utilized less frequently in treating Primary Peritoneal Cancer (Primary Peritoneal Carcinoma), poses substantial limitations when applied. It cannot discriminate effectively between cancerous and healthy cells, leading to extensive collateral damage within abdominal tissues. Studies indicate persistent radiation-induced injuries like fibrosis, adhesions, enteritis, and chronic pain syndrome affect over 50% of radiation-treated patients in Asia-Pacific regions.
- Long-term tissue scarring and organ dysfunction
- Severe chronic gastrointestinal symptoms including diarrhea, malabsorption, and persistent pain
- Increased risk for subsequent malignancies; up to 300% elevation in secondary cancer risk profiles
Given these profound effects, radiation therapy usage for Primary Peritoneal Cancer (Primary Peritoneal Carcinoma) remains severely limited, primarily reserved as adjunct or palliative strategy in late-stage scenarios. Radiation-related side effects significantly reduce the general welfare, independence, and emotional wellbeing of patients, further emphasizing the urgent necessity for safer, targeted treatment innovations.
Risks and Limitations of Surgical Intervention
Surgical treatments for Primary Peritoneal Cancer (Primary Peritoneal Carcinoma), involving cytoreductive procedures, are complex, lengthy, and carry significant perioperative and postoperative risks. Often performed as extensive debulking surgery, these interventions require surgeons’ exceptional skill levels, typically available only at specialized centers within Hong Kong and larger metropolitan areas across Asia.
- High risk of infection (up to 40%), sepsis, and abdominal organ injury
- Significant blood loss resulting in prolonged hospitalization and recovery
- Chronic abdominal pain and compromised gastrointestinal functions post-surgery
Even with meticulous surgical expertise, tumor cells are often inadequately removed, leaving residual microscopic cancer that perpetuates disease recurrence. Surgical procedures see limited success particularly in widespread metastatic cases where objective response rates drastically drop, contributing to survival rates well below 21% for advanced metastatic Primary Peritoneal Cancer (Primary Peritoneal Carcinoma).
Metabolic Resistance Mechanisms
One critical limitation of conventional therapies includes the robust metabolic adaptations of Primary Peritoneal Cancer (Primary Peritoneal Carcinoma) cells, significantly reducing treatment effectiveness over time. Cancer cells display adaptive biochemical mechanisms, such as elevated glycolytic metabolism, known as the Warburg effect, whereby glucose consumption can be up to 200 times normal cell levels. Additionally, glutamine dependency allows cancer cells to resist nutrient deprivation arising during chemotherapy, promoting survival under physiological stress conditions.
- 400% surge in DNA repair enzyme activity reducing chemotherapy efficacy
- Adaptative metabolism (Warburg effect and glutaminolysis pathways) enhancing cellular survival and proliferation
- Rapid development of therapeutic resistance reducing long-term survival outcomes significantly
As these metabolic resistance pathways continue to hinder the efficacy of traditional cancer treatments, innovations in metabolic oncology hold immense potential for breakthroughs, offering hope for improved patient outcomes across Asia-Pacific regions.
Implications for Hong Kong and Asian Patients
Limitations associated with conventional Cancer treatments like chemotherapy, radiation therapy, and surgical interventions pose particular challenges for patients residing in Hong Kong and throughout Asia. Cultural nuances, limited specialized treatment accessibility in certain rural areas, high treatment costs, and emotional distress further compound these challenges.
- Limited access to specialized centers in rural Asia
- Higher incidence of treatment discontinuation due to financial constraints
- Growing need for patient-centered therapeutic alternatives
Reflecting on these regional challenges underscores the importance of developing and adopting more targeted and personalized therapies that leverage emerging cancer metabolic understanding in treating Primary Peritoneal Cancer (Primary Peritoneal Carcinoma). Addressing current treatment limitations reinforces the commitment towards innovative therapies, like the groundbreaking 4D Therapy, enabling a hopeful outlook and better quality of life for patients.