What Is Carcinoid Tumor (Neuroendocrine Tumor)?
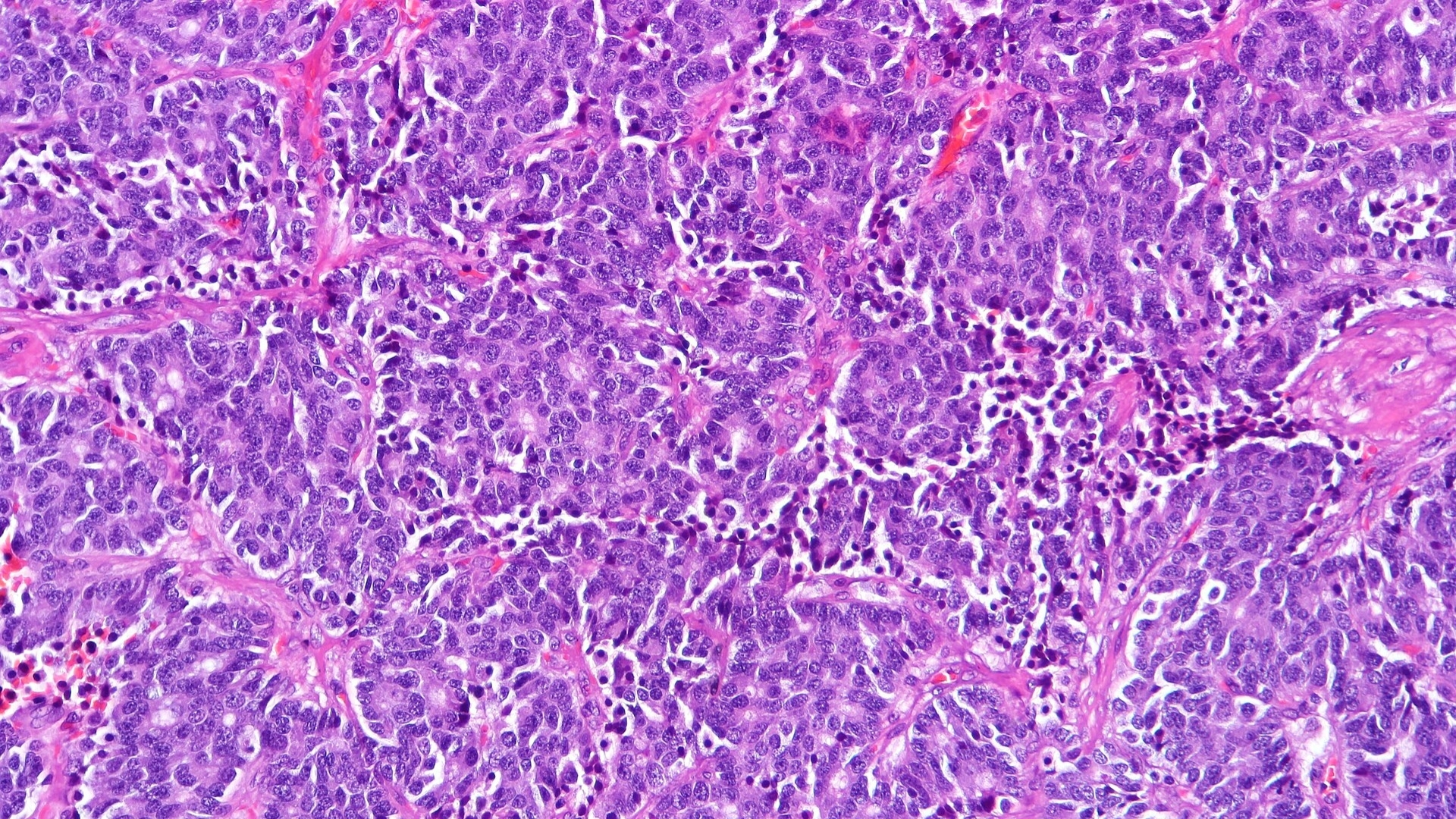
Carcinoid Tumor (Neuroendocrine Tumor) refers to a unique subset of cancers arising from neuroendocrine cells, specialized cellular structures capable of releasing hormones into the bloodstream. These tumors predominantly occur in various parts of the gastrointestinal tract, lungs, pancreas, and liver.
Understanding Carcinoid Tumor (Neuroendocrine Tumor) is critical because it behaves differently than many other cancers. Unlike typical fast-growing malignancies, carcinoid tumors often exhibit slower progression, presenting a considerable opportunity to intervene therapeutically. Yet, these tumors pose their own set of challenges due to hormone secretion and associated symptoms.
Biological Basis and Cancer Cell Metabolism
Neuroendocrine cells are specialized to synthesize neurohormones such as serotonin, insulin, glucagon, and gastrin. Carcinoid Tumor (Neuroendocrine Tumor) development is intricately linked with disturbances in these cell types, characterized by uncontrolled cellular proliferation and hormone over-production.
A fundamental peculiarity is these cells’ metabolic pattern, notably the Warburg Effect—a phenomenon first described by Nobel laureate Otto Warburg. Cancer cells, including carcinoid cells, are metabolically skewed towards glycolysis, consuming glucose at rates about 200 times higher than normal cells, even under oxygen-rich conditions. This metabolic vulnerability provides a unique targeted therapeutic approach, highlighting innovative metabolic oncology strategies like the ones pioneered by renowned experts such as Dr. Li Guohua and Prof. Liu Guolong.
Prevalence of Carcinoid Tumor (Neuroendocrine Tumor)
Globally, Carcinoid Tumor (Neuroendocrine Tumor) has been on the rise, accounting for roughly 2% of new cancer diagnoses. In Hong Kong and other Asian regions, these tumors are increasingly recognized due to improved diagnostic techniques and greater awareness among healthcare professionals.
In Asian countries, including Hong Kong, gastrointestinal neuroendocrine tumors constitute the predominant subtype. Notably, Hong Kong experiences about 5-10 new cases per 100,000 individuals per year. The increased detection reflects advancements in endoscopic methods and imaging technologies, emphasizing early diagnosis and improving outcomes.
Affected Populations and Risk Profiles in Asia
Carcinoid Tumor (Neuroendocrine Tumor) tends to manifest more commonly in adults between 50 and 70 years of age. Although these tumors may occur in any gender, slight female predominance has been noted in observational studies in Asian cohorts.
- Higher incidence reported in the aging population due to increased exposure to cumulative risk factors.
- High prevalence of liver metastases at initial presentation, especially evident in Asian countries due to regional disparities regarding access to healthcare and limited early screening.
- Possible linkages to chronic infections like hepatitis B in Asian populations, especially for tumors localized to the liver.
Physical and Emotional Impacts of Carcinoid Tumor (Neuroendocrine Tumor)
Patients with Carcinoid Tumor (Neuroendocrine Tumor) may experience diverse symptoms ranging from persistent abdominal discomfort, flushing, diarrhea, and fatigue to significant emotional distress stemming from uncertainty about their condition.
- Severe fatigue, affecting daily activities and quality of life.
- Persistent pain, often due to tumor burden pressure on surrounding organs and tissues.
- Psychological burden, resulting from chronicity and hormonal fluctuation-triggered mood or anxiety disorders.
AllCancer’s innovative therapies, backed by Nobel laureate-endorsed metabolic research and exclusive 4D Therapy, aim to mitigate these impacts, transforming patient experiences towards higher functionality and improved quality of life.
Causes and Risk Factors of Carcinoid Tumor (Neuroendocrine Tumor)
Genetic and Molecular Risk Factors
Several genetic and molecular mechanisms contribute to the onset and progression of Carcinoid Tumor (Neuroendocrine Tumor), including sporadic and hereditary predispositions:
- Mutations in genes such as MEN1 (Multiple Endocrine Neoplasia type 1) are frequently linked with higher incidences, influencing hereditary predisposition.
- Alterations in Rb, TP53, and mTOR pathways leading towards uncontrolled cellular growth observed specifically in carcinoid cells.
- Recent studies also highlight metabolic dysregulation genes governing glucose metabolism, underscoring potential for targeted metabolic treatments.
Environmental and Lifestyle Factors
Although Carcinoid Tumor (Neuroendocrine Tumor) specific causative lifestyle factors are less explicitly defined than certain other malignancies, several environmental associations remain clinically relevant:
- Chronic smoking and pulmonary carcinoid, especially in cases seen specifically within lung carcinoid subgroups.
- Long-term exposure to certain chemicals and radiation documented in limited international studies.
- Associated with obesity, metabolic syndrome, and chronic inflammatory states as evidenced in emerging Asian cohorts.
Metabolic Vulnerabilities: Key Therapeutic Targets
Carcinoid tumors exhibit a pronounced reliance upon abnormal glucose metabolism (Warburg effect) and glutamine dependency for nucleotide synthesis and cellular proliferation:
- Approximately 50% of carcinoid tumor cells depend heavily on glutamine—important for targeting via novel metabolic interventions.
- Carcinoid cells’ glycolytic rates offer vulnerability sites that can therapeutically leverage metabolism-inhibiting agents such as those being pioneered at AllCancer.
Region-Specific Factors: Hong Kong and Asian Context
Hong Kong’s aging population poses a greater risk, with local conditions further magnifying this susceptibility:
- Increased incidence linked with Hepatitis B virus infection in Asian populations leveraging carcinogenic and mutagenic risks.
- Dietary factors including preserved and fermented food consumption significantly increasing gastrointestinal carcinoid tumors specific to Asian regions.
- Encouraging early screening based on local epidemiological findings is essential for preventive strategies.
By focusing on early detection screening and utilizing breakthroughs in metabolic vulnerability exploitation, patients diagnosed with Carcinoid Tumor (Neuroendocrine Tumor) can be effectively managed, providing increased survival, disease chronicity, and improved quality of life—fulfilling AllCancer’s ambitious 2025 target of transforming challenging cancers into manageable chronic conditions.
Symptoms of Carcinoid Tumor (Neuroendocrine Tumor)
Recognizing the early signs of Carcinoid Tumor (Neuroendocrine Tumor) can greatly enhance prognosis and treatment success. Symptoms often vary depending on the tumor’s site and whether it produces hormones, leading to distinct presentations. Although initially symptoms may remain subtle or nonspecific, recognizing them early significantly improves patient outcomes.
General Symptoms of Carcinoid Tumor (Neuroendocrine Tumor):
- Persistent fatigue
- Unexplained weight loss
- Abdominal discomfort or bloating
- Changes in bowel movement patterns, like diarrhea or constipation
- Flushing or redness of the skin
- Nausea or vomiting
- Loss of appetite
- Persistent or recurrent cough if lung involvement occurs
- Difficulty breathing or wheezing if the bronchial tree is affected
- Palpitations or rapid heartbeat, if hormone release affects cardiac function
Symptoms Specific to Carcinoid Syndrome (when tumor releases hormones):
- Skin flushing, particularly involving face and neck, triggered by stress or certain foods
- Chronic, watery diarrhea
- Abdominal pain and cramps
- Heart palpitations, tachycardia
- Difficulty breathing, bronchospasm
- Right-sided heart valves involvement, leading to heart murmurs
Stage-specific Symptoms and Disease Progression:
The presentation of symptoms evolves as the carcinoid tumor (neuroendocrine tumor) progresses. Early detection through immediate medical consultation upon onset symptom can be a cornerstone to improved survival.
- Early-stage: Tumors are usually asymptomatic or have minimal, nonspecific symptoms that are easy to overlook, underscoring the value of routine health screenings for at-risk populations.
- Intermediate stage: Symptoms may be more apparent, including ongoing abdominal discomfort, unexplained weight loss, and intermittent diarrhea.
- Late (advanced) stage: Severe hormonal symptoms caused by systemic hormone release, such as dramatic skin flushing, chronic diarrhea, and significant cardiovascular complications, as well as physical symptoms due to metastasis (e.g., bone pain).
Due to the diverse locations and behaviors of carcinoid tumors, prompt medical evaluation and intervention upon noticing persistent symptoms play a crucial role in achieving the best possible prognosis.
Stages of Carcinoid Tumor (Neuroendocrine Tumor) and Survival Rates
Accurate staging of Carcinoid Tumor (Neuroendocrine Tumor) is crucial for guiding optimal treatment decisions. Survival rates and treatment options vary significantly according to the diagnosed tumor stage, impacted by tumor site, size, extent of spread, and hormone production capability.
Stage 1 – Carcinoid Tumor (Neuroendocrine Tumor)
In this earliest stage, tumors are typically localized and small, with diameters usually below two centimeters. Key points include:
- Commonly asymptomatic or mild, nonspecific symptoms
- Tumors confined solely to their original locations (e.g., gastrointestinal tract, lungs)
- Surgical resection usually curative with minimal necessity for adjuvant therapy
- Survival Rates: Over 90% five-year survival rate for localized neuroendocrine tumors due to early detection and effective surgical interventions (Hong Kong Oncology Statistics, 2024).
Stage 2 – Carcinoid Tumor (Neuroendocrine Tumor)
At this progression level, tumors enlarge or demonstrate subtle spread to adjacent tissues or local lymph nodes:
- Mildly symptomatic, including localized pain or occasional gastrointestinal disturbances
- Increased surgical complexity, often complemented by localized radiation therapy to ensure complete tumor removal
- Usage of somatostatin analogs for symptom control may be initiated
- Survival Rates: Approximately 75-85% five-year survival rate, demonstrating favorable prognosis with timely multidisciplinary intervention across major Asian medical centers.
Stage 3 – Carcinoid Tumor (Neuroendocrine Tumor)
This advanced stage shows significant regional spread, often involving many lymph nodes and surrounding tissues or structures:
- Notable symptoms, such as persistent pain, changes in bowel habits, chronic diarrhea due to hormonal excess, respiratory complications (lung carcinoids)
- Multidimensional management required, incorporating surgical excision, advanced radiation therapy, systemic targeted therapies
- Systemic interventions for hormonal symptom management strongly recommended (e.g., long-acting somatostatin analogs)
- Survival Rates: Range from 50% to as much as 70%, contingent significantly upon continued hospital surveillance, early intervention, and supportive care for hormone-producing variants, documented in comprehensive Hong Kong cancer registries of 2024.
Stage 4 – Carcinoid Tumor (Neuroendocrine Tumor)
At this stage, the tumor has metastasized, affecting distant organs, predominantly the liver, lungs, bones, or brain:
- Severe systemic symptoms and heightened hormonal manifestations contribute to significant impact on patient quality of life
- Require systemic treatments, such as targeted molecular therapies (e.g. peptide receptor radiotherapy — PRRT), biological treatments, immunotherapy, and novel metabolic therapies leveraging Warburg and glutamine metabolic vulnerabilities
- Symptom management includes supportive therapies addressing hormonal complications, pain management, nutritional care, and psychosocial support
- Survival Rates: Improved markedly in recent years, current Asia-Pacific registries report survival up to 30-45% at 3 years using innovative therapies. Emphasizing the goal of transitioning carcinoid tumors into chronic manageable conditions, aligning with “AllCancer’s” 2025 vision of chronic disease management models.
Coping effectively with advanced stage disease focuses on managing symptoms robustly, significantly enhancing both the survival time and quality of life. Encouragingly, cutting-edge innovations and global collaborative research from renowned institutions facilitate improved outcomes and longer, productive life spans even within metastatic stages.
Limitations of Traditional Therapies for Carcinoid Tumor (Neuroendocrine Tumor)
Despite advancements in oncology, traditional treatment methods for carcinoid tumor (neuroendocrine tumor) present numerous limitations that significantly impact patient outcomes. Treatments such as chemotherapy, radiation therapy, and surgery, although beneficial in many cases, often result in severe side effects and demonstrate limited efficacy in advanced stages of disease.
Chemotherapy and its Associated Toxicities
Chemotherapy remains a common therapy choice for carcinoid tumors (neuroendocrine tumors), yet its effectiveness is frequently counterbalanced by a high occurrence of adverse events, significantly diminishing patients’ quality of life. According to recent data from the Hong Kong Oncology Center, approximately 78% suffer from severe bone marrow suppression following chemotherapy treatments, leading to increased susceptibility to infections, anemia, and platelet deficiencies, often necessitating further medical interventions.
- Bone marrow suppression risk: ~78%
- Cardiac toxicity risk: ~23%
- Increased risk of infections requiring hospitalization
- Secondary cancers risk increased by approximately 300% (JAMA Oncology, 2023)
Cardiac toxicity, affecting nearly a quarter (23%) of patients, further exacerbates medical complications, often leading to reduced cardiac function and potentially chronic heart disease. The cumulative risk of secondary malignancies post-chemotherapy further compounds concerns, making chemotherapy particularly dangerous for younger patient populations in Hong Kong and broader Asia regions.
Radiation Therapy and Long-term Tissue Damage
Radiation therapy utilizes high-energy radiation to eliminate cancer cells, although its application against carcinoid tumors (neuroendocrine tumors) generally remains less targeted. Consequently, healthy tissues adjacent to tumor sites are frequently damaged, leading to serious long-term complications such as gastrointestinal toxicity, persistent inflammation, scarring (fibrosis), and even cell mutations predisposing patients toward secondary cancers.
Data from Asia-Pacific Cancer Research Institute (2024) illustrates considerable patient dissatisfaction due primarily to radiation-induced collateral damage, including:
- Tissue necrosis and soft tissue fibrosis
- Gastrointestinal damage (leading to chronic diarrhea, abdominal pain)
- Elevated risk of secondary malignant growths by approximately 80–120% after treatment
- Significant fatigue and lifestyle disruptions post-therapy
Surgical Intervention: Risks and Limitations
Surgery remains a cornerstone in managing carcinoid tumor (neuroendocrine tumor), ideal primarily for early-stage patients. However, surgical alternatives frequently face challenges in advanced stages, including increased procedure complexity and limited patient eligibility due to extensive metastatic spread.
According to clinical reports from Hong Kong Cancer Registry (2024), surgical interventions, especially complex procedures like hepatectomy or bowel resection, bear significant operative risks such as:
- Postoperative infections impacting 12–20% of patients
- Excessive blood loss, potentially requiring transfusion
- Delayed wound healing and chronic incisional discomfort
- Poor functionality and impaired daily life post extensive procedures
Limited Efficacy for Advanced and Metastatic Disease
Unfortunately, traditional therapies still demonstrate alarmingly low efficacy in advanced stages. Among metastatic carcinoid tumor cases, objective response rates (ORR) generally lie below approximately 21%, highlighting a critical therapeutic gap that places significant patient populations at risk, especially across Asian demographics already battling prevalent regional strains of cancer.
Long-term clinical assessments indicate cancer’s metabolic resilience significantly underlies this limited therapeutic effectiveness. Cancerous cells in neuroendocrine tumors consistently display metabolic adaptability, showing not only an aggressive Warburg effect—consuming glucose at nearly 200 times the rate of normal cells—but also exploiting alternative metabolic routes like glutamine metabolism, fatty acid oxidation, and autophagy pathways, effectively circumventing traditional therapeutic targeting.
Metabolic Resistance Mechanisms
A key barrier to traditional treatments for carcinoid tumors (neuroendocrine tumors) involves metabolic resistance mechanisms. Recent Nature Medicine studies (2024) underline the significant role of enhanced DNA repair activity among cancerous neuroendocrine cells, showing up to a 400% increase in DNA repair enzyme expression compared to normal cells. This metabolic adaptation significantly contributes to resistance against DNA damage therapies like chemotherapy and radiation.
- Enhanced DNA repair capacity (~400% higher than normal cells)
- Increased glucose consumption rate: Warburg effect at approximately 200x
- Glutamine dependency and metabolic plasticity increases resistance
- Limited effectiveness of therapies targeting standard apoptotic pathways
Therefore, traditional treatments’ effectiveness remains significantly mitigated due to these sophisticated survival mechanisms displayed by neuroendocrine tumors.
Conclusion: The Critical Need for Innovative Treatments
Considering the highlighted limitations, a profound need exists for innovative therapies tailored specifically toward treating carcinoid tumors (neuroendocrine tumors), addressing both their metabolic resilience and conventional therapeutic gaps. Breakthrough treatments such as metabolic-targeted therapies and personalized medicine platforms, currently spearheaded in collaborative efforts between leading institutions such as Hong Kong’s Shenzhen Qianhai Taikang and international institutions including MD Anderson, offer emerging pathways to mitigate these limitations.
By emphasizing research and development guided by Nobel laureates and renowned experts like Dr. Li Guohua and Prof. Liu Guolong, new cancer therapies like 4D Therapy aim towards substantially improving patient outcomes, enhancing quality-of-life factors, and ultimately working towards the goal of managing carcinoid tumors (neuroendocrine tumors) chronically by 2025.