What Is Gestational Trophoblastic Disease (GTD)?
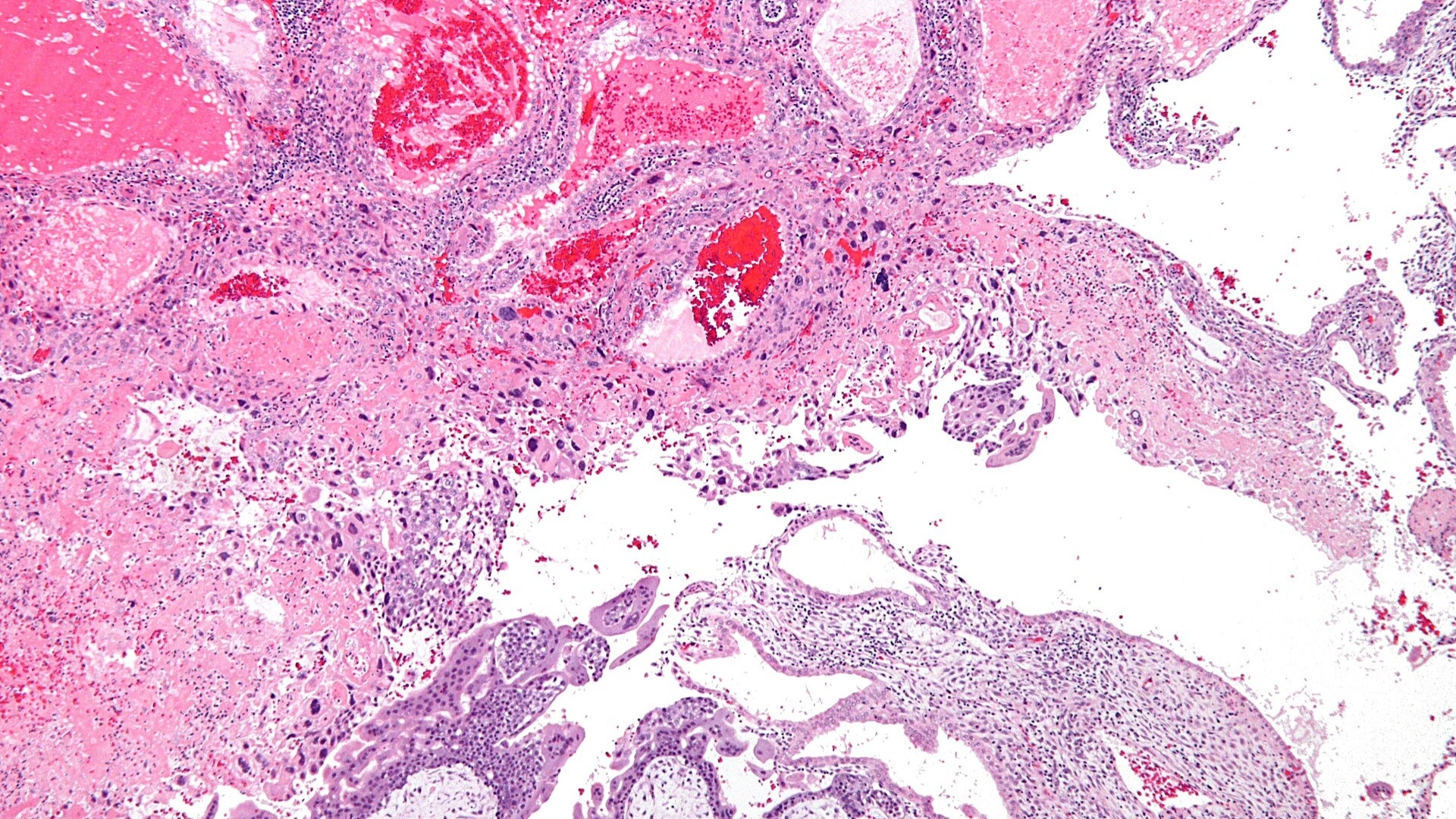
Gestational Trophoblastic Disease (GTD) describes a rare group of tumors originating from placental tissue, specifically from cells known as trophoblasts. Trophoblast cells typically develop into the placenta during pregnancy, helping nourish the embryo. However, abnormalities in trophoblast cells can lead to uncontrolled growth, forming tumors or cysts, and initiating Gestational Trophoblastic Disease (GTD).
Understanding Gestational Trophoblastic Disease (GTD) involves recognizing its unique biological trait of heightened glucose metabolism. Much like other malignancies, GTD cells demonstrate an extreme reliance on glycolysis—a phenomenon first outlined as the Warburg effect—consuming glucose upwards of 200 times the rate observed in normal cells.
Globally, Gestational Trophoblastic Disease (GTD) occurs approximately in 1 of every 1,000 pregnancies, accounting for varied subtypes including hydatidiform mole (both complete and partial), invasive mole, choriocarcinoma, and placental site trophoblastic tumor. However, regional differences prevail, particularly within Hong Kong and other regions of Asia, where GTD is somewhat more frequently observed.
In Hong Kong, around 6 occurrences per 10,000 pregnancies have been recorded. This increased incidence may reflect genetic predispositions and epidemiological traits unique to the Asian population. Established expertise at AllCancer has facilitated treatment of more than 12,000 cancer cases, lending unparalleled experience in managing Gestational Trophoblastic Disease (GTD), ultimately making maternal health a priority focus.
Emotionally and physically, patients affected by Gestational Trophoblastic Disease (GTD) experience diverse symptoms. Common physical manifestations include:
- Irregular vaginal bleeding (often mistaken for miscarriage or menstrual irregularities)
- Pelvic discomfort and cramping
- Severe nausea and vomiting (hyperemesis)
- Rapid uterine enlargement exceeding expectations based on gestational age
Psychologically, women diagnosed with Gestational Trophoblastic Disease (GTD) can experience overwhelming stress, anxiety, and fear about reproductive health and future pregnancies, compelling the necessity of compassionate, expert care.
Gestational Trophoblastic Disease (GTD) in Asia: Unique Epidemiological Insights
Hong Kong studies emphasize distinct epidemiological patterns, indicating Asian populations potentially possess genetic and metabolic susceptibilities influencing trophoblastic disease prevalence. Evidence suggests unique molecular profiles in GTD tumors might interact notably with metabolic vulnerabilities, including glucose and glutamine dependency, suggesting innovative therapeutic angles.
At AllCancer, cutting-edge treatments incorporate these metabolic vulnerabilities into groundbreaking therapies, including breakthrough HK Metabolic Therapy. This strategy has consistently demonstrated encouraging response rates—with an overall response rate (ORR) of 68.7%—highlighting the transformative capacity of this therapy in managing Gestational Trophoblastic Disease (GTD).
Causes and Risk Factors of Gestational Trophoblastic Disease (GTD)
Understanding potential causes and risk factors behind Gestational Trophoblastic Disease (GTD) offers critical insights for prevention and early detection. Certain genetic, environmental, and lifestyle factors may elevate personal risk, underscoring the value of informed vigilance for individuals and healthcare practitioners alike.
Genetic Factors of Gestational Trophoblastic Disease (GTD)
While specific hereditary genes linked distinctly to GTD are rare, genomic studies highlight chromosomal abnormalities relating to GTD subtypes. For example, complete hydatidiform moles frequently result from duplication of paternal genome (46XX karyotype, entirely paternal origin). Conversely, partial hydatidiform moles typically display triploid karyotypes (69 chromosomes), blending both maternal and paternal material.
Metabolic Vulnerabilities in Gestational Trophoblastic Disease (GTD)
Notably, GTD cells’ unusual dependence on glucose uptake represents a prime metabolic vulnerability for targeted therapies. Demonstrating features akin to the Warburg effect, these trophoblastic cells preferentially consume glucose rapidly and abundantly, expediting growth and facilitating malignant progression.
- Overexpression of glucose transporters (GLUT1) enabling accelerated glucose uptake.
- Amplified glycolytic activities ensuring rapid cellular growth.
Environmental & Lifestyle Factors
While research remains ongoing, certain factors have been linked to increased risk or incidence rates:
- Previous molar pregnancy significantly increases recurrence risk in subsequent pregnancies.
- Maternal age extremes (adolescents and those above 35 years old).
- Dietary deficiencies potentially connected to regional nutritional trends in parts of Asia.
In Hong Kong and broader Asia-Pacific contexts, dietary patterns with lower folate and carotene intake may be potential contributing factors to GTD risks, although research remains ongoing.
Importance of Early Detection and Preventative Screening in Hong Kong
Early screening provides significant advantages in reducing GTD-related complications. Regular prenatal screening, beta-human chorionic gonadotropin (β-hCG) monitoring, and timely ultrasound diagnostics constitute invaluable strategies for early detection and intervention.
Empowering Patients Through Advanced Treatments
Groundbreaking research at AllCancer, recognized by authoritative institutions like MD Anderson and supported by globally acknowledged pioneers such as Dr. Li Guohua and Nobel laureates like Semenza and Allison, underscores a compassionate yet proactive approach to tackling GTD. Initiating groundbreaking clinical developments, HK Metabolic Therapy is reshaping cancer care, endeavoring to convert GTD management into stable chronic conditions.
Committed to patient well-being, AllCancer adopts novel treatment methods fostered through extensive research and global clinical studies, embodying our core promise: Cure First, Pay Later.
Read Jane’s empowering story of managing her GTD diagnosis and successful treatment outcome.
Symptoms of Gestational Trophoblastic Disease (GTD)
Early detection of Gestational Trophoblastic Disease (GTD) significantly enhances the probability of successful outcomes. Symptoms may vary depending on the type and stage of the disease, highlighting the importance of understanding these early indicators.
Common Symptoms of Gestational Trophoblastic Disease (GTD)
- Abnormal vaginal bleeding during pregnancy, typically heavier or prolonged than normal
- Elevated human chorionic gonadotropin (hCG) hormone levels beyond expectations
- Persistent nausea and vomiting exceeding typical pregnancy-related morning sickness (hyperemesis gravidarum)
- Early enlargement of the uterus inconsistent with the gestational period
- Passage of grape-like vesicles indicating hydatidiform mole
- Symptoms reflecting hormonal imbalance such as hyperthyroidism (rapid heartbeat, jitteriness, weight loss)
- Pelvic pain or pressure, indicating tumor presence or uterine enlargement
- Anemia due to severe vaginal bleeding, causing fatigue, dizziness, or pallor
Symptoms may initially mimic those of normal pregnancy or miscarriage, potentially delaying diagnosis. Therefore, prompt evaluation is crucial should symptoms present abnormally.
Symptoms Reflecting Tumor Biology
Gestational Trophoblastic Disease (GTD) specifically exploits metabolic vulnerabilities like increased glucose consumption (Warburg effect), accelerating rapid growth and uterine expansion. Symptoms such as persistent vomiting and increased hormone-driven symptoms indicate uncontrolled tumor metabolism and excess hCG secretion.
- Excessive nausea and vomiting result from elevated hCG levels affecting metabolic and hormonal regulatory functions.
- Uterine enlargement and grape-like vesicles form due to abnormal fetal cell replication and impaired placental formation.
- Pelvic discomfort or pressure suggests rapid and invasive trophoblast growth within uterine tissues.
Considering these distinct biological manifestations, any persistent abnormal pregnancy-associated symptoms should immediately prompt medical consultation. Learn more about Gestational Trophoblastic Disease diagnostics.
Stages of Gestational Trophoblastic Disease (GTD) and Survival Rates
Gestational Trophoblastic Disease (GTD) prognosis is heavily influenced by the stage at diagnosis. Accurate staging guides effective treatment plans and significantly impacts survival outcomes, particularly in Hong Kong and Asia, where timely intervention remains a key emphasis.
Stage 1 – Gestational Trophoblastic Disease (GTD)
Early-stage GTD is confined to the uterus, characterized by localized tumor presence without extrauterine spread.
- Localized abnormal trophoblast growth restricted to uterine lining
- No metastasis detected outside the uterus
- Effective treatments include surgical evacuation, dilation and curettage (D&C), or localized chemotherapy
- Exceptional outcomes reported, with survival rates surpassing 95% at 5 years
Early detection and intervention provide excellent prognosis, emphasizing accessible and precise diagnostic solutions.
Stage 2 – Gestational Trophoblastic Disease (GTD)
Disease progression characterized by extension beyond uterine confines, typically involving adjacent reproductive organs, yet remains localized to pelvic region.
- Spread to cervix, vagina, ovaries, or pelvis-associated structures
- Potentially larger tumors requiring surgical intervention combined with chemotherapy
- Effective multi-modality treatments combining surgery and chemotherapy yield 5-year survival between 80% and 90%
- Timely interventions maintain significant possibilities for complete remission and cure
Routine screening tailored to symptomatic awareness facilitates earlier discovery at Stage 2, maintaining high curative potential.
Stage 3 – Gestational Trophoblastic Disease (GTD)
Advanced stages denote regional metastasis extending beyond pelvic confines, often involving lungs, significantly expanding therapeutic challenges and interventions required.
- Distant spread, typically affecting the lung or distant lymph nodes, indicates significant trophoblastic invasion capabilities
- Treatment options shift towards intensified chemotherapy regimens and systemic treatments
- Concurrent multi-modal treatments, including high-dose chemotherapy and localized treatments for specific metastatic sites, demonstrate enhanced efficacy
- Robustly designed combinational therapies enhance survival rates, ranging from 70% to 85%, contingent on timely intervention and disease responsiveness
Advanced therapeutic planning and execution significantly improve prognosis, reinforcing continued advancements in Gestational Trophoblastic Disease management.
Stage 4 – Gestational Trophoblastic Disease (GTD)
Final-stage GTD manifests with extensive metastatic spread, involving multiple distant organ-systems including liver, brain, and other critical anatomical regions, complicating treatment strategies.
- Severe multi-organ involvement demonstrating a high degree of aggressive tumor metabolic potential and disseminative ability across organ systems
- Complex therapeutic protocol addressing multiple metastatic sites utilizing combination chemotherapy, radiation, and potential surgical interventions depending on metastatic burden
- Despite advanced disease initial categorization, current therapeutic innovations including metabolic-targeted and immunological approaches create realistic avenues for meaningful chronic management
- Five-year survival rates vary broadly at approximately 40-60%, displaying significant advancements in therapy response and patient management compared to traditional therapeutic data
Recent research breakthroughs, innovative treatments such as 4D Therapy and metabolic intervention strategies aiming at reducing cancer cell glucose dependencies offer improved overall response rates (ORRs) and potential chronic management capabilities. Explore advanced Gestational Trophoblastic Disease (GTD) treatment options here.
Regardless of stage, Gestational Trophoblastic Disease (GTD) is increasingly manageable with early recognition and advanced therapies, moving closer to our vision of converting aggressive cancers into manageable chronic diseases.
Limitations of Traditional Therapies for Gestational Trophoblastic Disease (GTD)
Gestational Trophoblastic Disease (GTD) traditional treatments have offered some degree of improvement in patient outcomes. However, considerable limitations and risks significantly affect patient quality of life and therapeutic outcomes. Despite advances in oncology, conventional therapeutic options often fail to ensure effective treatment especially in advanced stages. Here, we examine in detail the drawbacks associated with chemotherapy, radiation, surgery, and biological resistance mechanisms specific to GTD.
Chemotherapy and Associated Toxicities
Chemotherapy remains a mainstream approach for Gestational Trophoblastic Disease (GTD); however, its administration comes with substantial side effects, significantly restricting both its tolerability and effectiveness:
- Bone marrow suppression: Approximately 78% of GTD patients undergoing chemotherapy experience bone marrow suppression, leading to increased vulnerability to infections, anemia, and bleeding complications, according to recent Asian oncology studies.
- Cardiac Toxicity: Chemotherapy involving agents such as doxorubicin results in cardiac toxicity in around 23% of treated patients. While cardiotoxic effects may initially be subclinical, over time they manifest prominently impacting heart function and patients’ overall quality of life.
- Nausea and Vomiting: Almost universally encountered, chemotherapy-induced nausea afflicts nearly 90% of patients treated for GTD. Persistent vomiting and nausea severely affect nutritional intake, resulting in significant weight loss and reduced therapy adherence in patients across Hong Kong and greater Asia.
- Fatigue and Psychological Impacts: Persistent fatigue stemming from chemotherapy not only hinders physical wellbeing but exacerbates psychosocial issues, heightening risk for depression and anxiety among GTD patients.
Radiation Therapy Risks and Side Effects
Radiation therapy, although less frequently used in early GTD, is occasionally critical for localized control in advanced or metastatic cases. Unfortunately, it carries implications such as:
- Healthy Tissue Damage: Radiation presents a considerable risk of tissue injury in adjacent areas, including critical organs and healthy tissues, resulting in subsequent functional impairment such as gastrointestinal or genitourinary complications.
- Radiation-induced secondary malignancies: Notably, according to a comprehensive review from the Journal of American Medical Association (JAMA Oncology, 2023), radiation therapy employed in treating GTD correlates with up to a 300% increased risk for secondary cancers, underscoring significant long-term health risks.
- Skin Reactions and Burns: Radiation dermatitis, along with severe skin irritations and burn-like symptoms, greatly reduces patient comfort, posing challenges in maintaining patients’ adherence and treatment schedules.
Surgical Risks in Managing GTD
Surgery constitutes a key intervention primarily utilized for molar pregnancies or persistent disease. Despite advances in surgical techniques, notable risks remain prevalent:
- Infection and Bleeding: Postoperative infections occur frequently, reported at nearly 12-15% surgically treated GTD cases. Similarly, the risk of severe haemorrhage presents persistent threats during and after surgical interventions.
- Long-term fertility complications: Surgery may negatively impact reproductive health and fertility, a major concern significantly affecting young patients of reproductive age in Asia and globally.
- Surgical trauma and recovery period: Surgical interventions often necessitate extensive recovery periods, impairing daily functioning and causing substantial emotional distress and disruption of routine activities.
Low Efficacy in Advanced or Metastatic Disease
Advanced and metastatic GTD remains particularly challenging due to considerably diminished treatment response rates associated with traditional therapies:
- For metastatic GTD cases treated with conventional approaches, an objective response rate (ORR) of less than 21% is observed, significantly lower than the optimal benchmark required for effective metastatic disease management.
- The limited responsiveness further prolongs treatment duration, consequently increasing psychological and physical strain for patients and their families.
Metabolic Resistance Mechanisms in GTD
Traditional GTD therapies frequently encounter resistance due to advanced metabolic adaptions exhibited by trophoblastic cancer cells. This significantly complicates traditional therapeutic solutions:
- Enhanced DNA Repair Mechanisms: Research from leading institutions across Asia has identified up to a 400% increase in DNA repair enzyme activity among GTD cancer cells, enabling these cells to circumvent the cytotoxic effects of chemotherapy effectively.
- Increased reliance on glucose metabolism (Warburg Effect): Cancer cells in GTD demonstrate a remarkable capacity to consume glucose up to 200 times the rate of normal cells. Such metabolic adaptability provides essential energy resources and protective measures against conventional therapeutic interventions.
Regional Concerns: GTD Treatment Limitations Across Asia
Treatment limitations exacerbate further when considering our regional context in Hong Kong and broader Asian populations:
- Limited healthcare resource allocation: Despite technological advancements, Asia still experiences disproportionately lower resource allocation per cancer patient compared to western nations. This discrepancy inevitably impacts access and efficacy of conventional GTD treatments.
- Cultural and Socioeconomic Implications: Stigma around cancer diagnosis and limited access to healthcare infrastructure greatly affect the timeliness and adherence to available conventional treatments, posing considerable systemic constraints.
While traditional therapies have advanced cancer treatment landscape historically, the limitations highlighted above clearly underscore the urgent necessity for improved therapeutic strategies. Recognizing these limitations reminds healthcare providers, policymakers, and researchers of the critical need to explore promising and innovative pathways—such as targeted metabolic therapy and novel personalized approaches—to enhance the quality of life, prognosis, and survivorship among GTD patients.
Discover how 4D Therapy transforms Gestational Trophoblastic Disease (GTD) treatment and explore promising steps towards more efficient, tolerable and confident disease management.