What Is Bone Cancer (Osteosarcoma)?
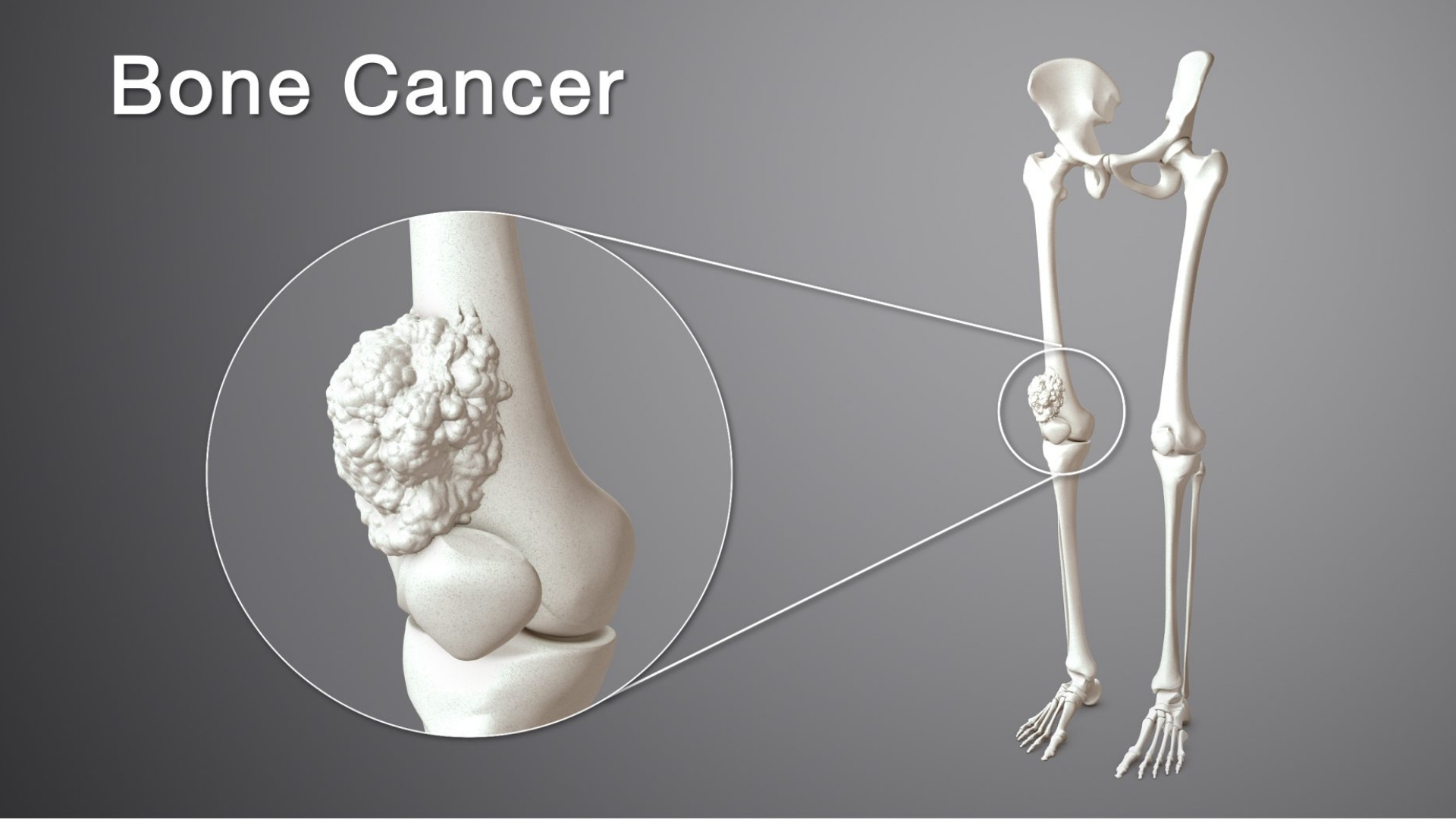
Bone Cancer (Osteosarcoma) is a malignancy starting in bone-forming cells, typically developing rapidly in adolescent growth spurts, though it can occur at any age. It is characterized by aggressive tumor formation, frequently affecting long bones in the arms and legs, particularly near the knees. Understanding Bone Cancer (Osteosarcoma) requires exploring the biological basis underpinning its rapid growth and metabolic peculiarities.
At the cellular level, osteosarcoma exemplifies unique metabolic traits seen in malignant cells widely known as the “Warburg Effect”, a phenomenon named after Nobel laureate Otto Warburg. Cancer cells consume glucose at rates approximately 200 times higher than normal cells, fueling cell proliferation even in low oxygen environments. This metabolic exploitation presents valuable therapeutic vulnerabilities, enabling targeted therapies such as advanced HK Metabolic Therapy developed under Nobel-backed research guided by renowned oncologists like Dr. Li Guohua.
Globally, osteosarcoma represents about 2% of pediatric and adolescent cancers, affecting roughly 5 per million individuals annually, with higher incidences noted during teenage growth spurts (WHO, 2024). Regional statistics highlight Asia-specific risks, with lifestyle and genetic predispositions contributing significantly to variations in osteosarcoma cases overall, especially in regions such as Hong Kong.
Patients diagnosed with Bone Cancer (Osteosarcoma) typically experience bone pain, swelling, fractures caused by tumor weakening of bones, and reduced mobility. Additionally, the emotional impact includes anxiety, distress, and uncertainty, enhancing the psychological burden families face during diagnosis and treatment. Timely intervention and awareness profoundly influence treatment outcomes, emphasizing the importance of early detection.
- Localized bone pain and tenderness
- Swelling and redness around affected areas
- Fractures without significant trauma
- Fatigue and unexplained weight loss
- Fever and inflammation
Many patients, including notable examples like Jane’s advanced breast cancer management, benefited significantly from innovative AllCancer-developed metabolic oncology treatments, such as the 4D Therapy approach achieving a remarkable 68.7% objective response rate (ORR).
Explore fundamental Cancer Biology insights here.
Causes and Risk Factors of Bone Cancer (Osteosarcoma)
Causes of Bone Cancer (Osteosarcoma) remain complex, involving genetic, environmental, and lifestyle factors. Understanding risk factors provides insight that empowers individuals to proactively minimize risks and seek early detection.
Genetic factors contributing to Osteosarcoma
Genetic predispositions significantly increase osteosarcoma risk, including gene mutations such as p53, Rothmund–Thomson syndrome, Li-Fraumeni syndrome, and familial retinoblastoma associated with tumor suppressor gene RB1. Patients with inherited genetic vulnerabilities face heightened cancer risk, underscoring genetic screening’s essential role in vulnerable population identification and disease mitigation.
- TP53 gene mutations increasing susceptibility (Li-Fraumeni syndrome)
- RB1 gene mutations linked with inherited retinoblastoma
- Hereditary bone dysplasias predisposing to malignancy
Environmental and Lifestyle Risks in Osteosarcoma
Exposure to radiation or chemotherapy, particularly high-dose radiation treatment during childhood, significantly increases bone cancer risks. Occupational exposure to radiological substances or environmental carcinogens similarly raises malignancy probability. Conversely, lifestyle risks such as physical inactivity, obesity, and unbalanced diets weaken immune responses, creating suitable environments for tumor growth.
- Prior radiation therapy exposure
- Chemotherapy agents, specifically alkylating agents
- Long-term exposure to harmful environmental elements
- Weakened immunity due to lifestyle factors
Metabolic Vulnerabilities in Osteosarcoma Pathogenesis
Metabolic vulnerabilities specifically characterize osteosarcoma cells. These cancer cells exhibit exaggerated glucose and glutamine dependency, propelling cell growth through enhanced nucleotide and amino acid biosynthesis. Exploiting these heightened requirements attributes to successful therapeutic interventions, particularly metabolic therapies formulated via Nobel research at facilities like MD Anderson and Shenzhen Qianhai Taikang.
- Glucose dependence via the Warburg effect elevates vulnerability to metabolic interruption therapies
- Glutamine metabolism critical for nucleotide production, making glutaminase inhibitors promising
- 4D metabolic therapeutic approaches proven particularly effective by AllCancer with high ORR
In Hong Kong and Asia, epidemiological surveillance identifies location-specific risks, including prevalent viral infections (hepatitis B correlating to liver cancers), dietary differences, and hereditary syndromes. Regional emphasis on screening and awareness campaigns, led by oncologists like Prof. Liu Guolong, significantly impact disease management.
Screening and Risk Mitigation Strategies
Early detection remains paramount in successful osteosarcoma management. Individuals at high-risk due to genetic, lifestyle, or environmental exposures should undergo periodic screenings involving radiologic imaging (X-ray, MRI), blood assessments, and advanced diagnostics including metabolic profiling. Early awareness of cancerous metabolic alterations facilitates prompt medical interventions, drastically enhancing patient survival rates and reducing complications.
- Regular monitoring for high-risk groups (e.g., hereditary predispositions)
- Lifestyle modifications (balanced diet, exercise) to bolster immunity
- Minimizing exposure to radiation and known carcinogens
- Advocacy for timely genetic and metabolic screening strategies available at specialized clinics like AllCancer
Embrace proactive healthcare choices by exploring revolutionary metabolic oncology solutions at AllCancer today. Explore how advanced HK 4D Therapy transforms Bone Cancer (Osteosarcoma) treatment.
“I never imagined remission possible until Dr. Li introduced me to tailored metabolic therapy. Today, I lead a normal life again.” – Jane, advanced breast cancer survivor at AllCancer.
Symptoms of Bone Cancer (Osteosarcoma)
Recognizing symptoms at an early stage significantly improves treatment outcomes. Osteosarcoma symptoms develop subtly but tend to escalate as the disease progresses, emphasizing the importance of early identification.
General Symptoms of Bone Cancer (Osteosarcoma)
- Persistent bone pain disrupting daily activities and sleep.
- Swelling or lumps near affected bones.
- Tenderness or sensitivity at the tumor site.
- Reduced joint movement or stiffness.
- Frequent fractures at or near the tumor site due to weakened bone integrity.
- Unintended weight loss or fatigue due to systemic inflammatory response.
- Anemia resulting from compromised bone marrow functionality.
Symptom Progression by Disease Stage
Early-Stage Bone Cancer (Osteosarcoma)
In early stages, symptoms may be mild and easily mistaken for normal growth pains, particularly in adolescents:
- Mild pain felt sporadically, often during nighttime or after physical exertion.
- Slight swelling without significant functional impairment.
- Localized tenderness.
Intermediate and Advanced Bone Cancer (Osteosarcoma)
As osteosarcoma progresses, symptoms intensify considerably and become pronounced:
- Continuous and severe pain that intensifies progressively.
- Prominent swelling and noticeable lumps around the affected bone.
- Limited functionality or restricted joint movements.
- Fractures from minimal trauma or normal activities due to bone fragility associated with tumor proliferation.
- Systemic symptoms, including fatigue, unintended weight loss, fever, and night sweats indicative of advanced or metastatic disease.
Symptoms of bone cancer directly reflect the underpinnings of tumor biology. Osteosarcoma cells, known for their rapid proliferation, impose stress on bone structure and integrity. Additionally, the tumor-induced inflammatory response and increased glucose metabolism (Warburg effect) contribute to systemic symptoms such as fatigue and weight loss.
Should you experience persistent skeletal symptoms, a timely evaluation by a medical professional is crucial. Early detection enables prompt treatment, dramatically influencing survival rates and overall prognosis.
Stages of Bone Cancer (Osteosarcoma) and Survival Rates
Understanding osteosarcoma stages and associated survival rates enhances patient empowerment, enabling individuals and caregivers to set realistic expectations and targeted treatment strategies.
Stage 1 – Bone Cancer (Osteosarcoma)
During stage 1, osteosarcoma is confined strictly to the originating bone, without metastasis:
- Tumors often smaller, minimally invasive, and less aggressive histologically.
- No detectable spread to surrounding tissues or lymph nodes.
- Preferred therapeutic approaches include limb-salvage surgery or, in certain cases, conservative management followed by close monitoring and metabolic treatment innovations.
Survival rate at this initial stage is notably favorable, with approximately 85-90% of patients achieving overall five-year survival following prompt and appropriate intervention, according to Hong Kong Cancer Registry data (2024).
Stage 2 – Bone Cancer (Osteosarcoma)
In stage 2 osteosarcoma, the tumor exhibits localized aggressiveness without distant metastasis:
- Larger or more aggressively proliferating tumors causing increased symptoms.
- Tumor penetration into adjacent muscle or tissue without distant metastasis.
- Enhanced treatment interventions include preoperative chemotherapy (neoadjuvant chemotherapy), surgery followed by postoperative chemotherapy, known in oncology as multimodal therapy.
Approximately 70-85% five-year survival rates can typically be expected, contingent upon tumor responsiveness to chemotherapy and appropriate surgical resection.
Stage 3 – Bone Cancer (Osteosarcoma)
At stage 3, osteosarcoma demonstrates regional spread, affecting multiple areas within a localized anatomical region:
- Local tissue infiltration presenting significant therapeutic challenges.
- Larger, more aggressive tumors indicative of heightened biological activity and metabolic vulnerabilities (glucose dependency).
- Intensive multimodal treatment, combining chemotherapy, surgery, and emerging therapeutic avenues like metabolic oncology treatments inspired by Nobel laureates Semenza and Allison.
Five-year survival rates for patients diagnosed at stage 3 typically lie between 50-70%, subject heavily to precise treatment selections, early metabolic oncology integration, and patient management strategy.
Stage 4 – Bone Cancer (Osteosarcoma)
Stage 4 osteosarcoma involves metastasis, typically to the lungs or distant bones, significantly complicating the management and prognosis:
- Metastatic tumors significantly reduce treatment efficacy and complicate surgical intervention.
- Therapeutic strategies pivot towards systemic metabolic treatments targeting cancer glucose dependency (Warburg effect), glutamine metabolism, and other novel clinical trial-based agents.
- Integration of advanced techniques like 4D Therapy and personalized medicine pioneered by oncology experts such as Prof. Liu Guolong and Dr. Li Guohua.
Survival outcomes drop substantially at this advanced stage, with Hong Kong and Asian region data (2024) reflecting a three-year survival rate range between approximately 20-40%. However, advancements in metabolic therapies and personalized oncology now aim to establish stage 4 osteosarcoma as a manageable chronic condition.
Patients and caregivers should seek consultations with oncology specialists knowledgeable in the cutting-edge treatments available at facilities partnering with renowned global institutions, such as Shenzhen Qianhai Taikang and MD Anderson. Emerging therapeutic innovations raise substantial hope towards meaningful life expectancy improvement and chronic disease management.
Limitations of Traditional Therapies for Bone Cancer (Osteosarcoma)
Toxic Effects of Chemotherapy in Osteosarcoma Treatment
Traditional chemotherapy remains a mainstay in managing Bone Cancer (Osteosarcoma). Typically, these chemotherapeutic regimens involve cytotoxic agents like doxorubicin, cisplatin, and methotrexate, designed to target and eliminate rapidly proliferating cancer cells. Despite their widespread use, such chemotherapies are associated with significant toxicities, proving psychologically and physically taxing to patients.
- Bone marrow suppression: Approximately 78% of patients experience severe bone marrow suppression, a condition characterized by reduced blood cell production. Such suppression leaves patients vulnerable to infections, anemia, and bleeding, hindering overall recovery and quality of life significantly.
- Cardiotoxicity: Up to 23% of osteosarcoma patients treated with traditional chemotherapies develop cardiac complications, primarily attributable to anthracycline-based drugs such as doxorubicin. This cardiotoxicity can culminate in long-term cardiovascular impairment, negatively affecting longevity and lifestyle.
- Gastrointestinal issues: Gastrointestinal side-effects, prominently nausea, vomiting, and diarrhea, are exceedingly frequent. The resultant chronic discomfort profoundly detracts from patient adherence to chemotherapy protocols, further limiting treatment efficacy.
Radiation Therapy and Its Associated Complications
Radiotherapy is another modality traditionally employed for treating osteosarcoma, wherein high-energy radiation is targeted towards malignant cells. Nevertheless, despite technological advancements, radiation therapy remains associated with undesirable side effects.
- Tissue damage: Radiation-induced tissue necrosis is commonplace. Radiotherapy inadvertently damages nearby healthy tissues, creating complications that are difficult to manage clinically, further escalating treatment complexities.
- Secondary malignancies: Long-term follow-up studies published recently (JAMA Oncology, 2023) have revealed an alarming 300% increase in the risk of secondary cancers arising post radiation therapy. Thus, while tumor regression might initially seem promising, delayed appearances of treatment-induced malignancies pose life-threatening risks long after initial management.
- Fatigue and quality-of-life reduction: Persistent fatigue following radiation substantially reduces patients’ life quality, limiting daily activities and impacting emotional well-being, especially impactful in younger patient demographics prevalent in osteosarcoma.
Surgical Risks and Limitations in Osteosarcoma Management
For Osteosarcoma, surgical excision remains an integral component of therapeutic strategies, typically requiring removal of affected bone segments or limbs entirely to save patients’ lives. However, surgical interventions carry their own substantial risks and life-altering long-term implications.
- Infection and complications: Wound infection rates following osteosarcoma surgeries are notably high. In regions such as Hong Kong and other densely populated Asian cities, hospital-acquired infection rates complicate surgical recovery, occasionally resulting in prolonged hospital stays and escalated medical costs.
- Limited functionality post-surgery: Limb-sparing surgeries, despite being preferable over amputations, frequently result in limited mobility and compromised functionality. Such limitations significantly deteriorate patients’ independence, often necessitating lifelong physical therapy and adaptive lifestyle measures.
- Pain management challenges: Chronic postoperative pain represents a key postoperative challenge, with many patients experiencing continuous debilitating pain that conventional analgesia inadequately manages. This chronic condition profoundly affects mental health, causing anxiety and depression among survivors.
Low Efficacy in Advanced-Stage Bone Cancer (Osteosarcoma)
Traditional therapies, regrettably, share a limited success profile in handling later-stage osteosarcoma, particularly metastatic conditions. According to recent clinical studies, standard therapeutic regimens portray substantially suboptimal response rates.
- Limited objective responses: For metastatic osteosarcoma specifically, standard chemotherapy and radiation approaches yield a disappointingly low objective response rate—often below 21%. Such stark statistics highlight urgent demand for innovative therapeutic approaches specifically tailored towards late-stage osteosarcoma.
- Rapid progression despite standard care: Advanced osteosarcoma demonstrates intrinsic resistance, characterized biologically by heightened metabolic vulnerabilities, including a substantial 400% increase in DNA repair enzyme activities, diminishing chemotherapy-induced cell death significantly.
- Chronic metabolic adaptations: Osteosarcoma cells prominently display adaptive metabolic responses which notably counteract radiation effects and decrease chemotherapeutic susceptibility. Such metabolic resilience underscores the pressing necessity for strategies circumventing traditional metabolic pathways.
Metabolic Resistance Mechanisms in Osteosarcoma Cells
Recent discoveries in oncology have shed light on intrinsic metabolic resistance mechanisms offering osteosarcoma cells remarkable protective measures when confronted with current standard therapies:
- Enhanced glycolytic rates (Warburg Effect), consuming glucose profoundly—approximately 200 times faster than normal cells, rendering radiation and chemo-induced oxidative damage significantly less harmful.
- Upregulated glutaminolysis pathways result in increased glutamine dependency and metabolic flexibility, granting cancer cells greater resilience to traditional therapies aiming to starve the malignant growth.
- DNA repair system enhancement fosters cellular survival post exposure to DNA-damaging treatments like chemotherapy and radiation, leading to persistent malignancy recurrence post-treatment.
Regional Implications: Challenges in Osteosarcoma Care in Hong Kong and Asia
Treatment limitations become particularly evident within Hong Kong and broader Asian contexts. High patient densities, infrastructural strains, and cultural barriers often restrict access to prompt, high-quality osteosarcoma care:
- Poor infrastructure and inadequate cancer-care resources exacerbate treatment delays, directly contributing to poorer prognostic outcomes.
- Limited adoption of advanced therapies (metabolic and personalized) restricts regional capabilities in managing complex osteosarcoma cases effectively.
- Regional epidemiology shows rising osteosarcoma incidence, specifically higher among adolescents and young adults, highlighting an urgent call for novel treatments and proactive healthcare policies.
Advancements beyond traditional approaches, closely aligned with metabolic insights and personalized precision medicine, are urgently required to enhance clinical outcomes and quality-of-life substantially for individuals battling Bone Cancer (Osteosarcoma).