What Is Vulvar Cancer (Vulvar Carcinoma)?
Vulvar Cancer (Vulvar Carcinoma) is an uncommon but significant form of cancer that originates in the external female genital organs, primarily the vulva. These malignant cells grow uncontrollably, often developing lesions or growths in the vulvar area. Although commonly identified in postmenopausal women, cases are increasingly appearing in younger populations, highlighting the importance of awareness and early diagnosis.
Biologically, Vulvar Cancer (Vulvar Carcinoma) arises when healthy vulvar cells mutate, developing characteristics conducive to uncontrolled proliferation. One hallmark of vulvar cancer biology—shared with many cancers—is metabolic reprogramming, specifically demonstrated through the Warburg effect. Cancer cells in Vulvar Cancer (Vulvar Carcinoma) show an abnormal increase in glucose metabolism, consuming glucose at rates up to 200 times greater than normal cells. This metabolic vulnerability allows for innovative therapeutic approaches focusing on disrupting their energy supply.
Globally, Vulvar Cancer (Vulvar Carcinoma) represents approximately 4-5% of gynecologic malignancies, with WHO studies from 2024 highlighting close to 45,000 new diagnoses annually worldwide. In Hong Kong and broader Asia-Pacific regions, awareness remains limited yet crucial—the incidence rate has gradually increased due to shifting lifestyle and risk factors such as HPV infection and demographic aging.
Patients diagnosed with this cancer often experience both physical and emotional burden:
- Chronic pain in vulvar regions
- Painful urination
- Bleeding or discharge not related to menstruation
- Formation of ulcers or lumps impacting daily activities
- Intense feelings of anxiety, embarrassment, and distress due to intimate nature
Given these challenges, at AllCancer, we provide compassion-driven education, supporting patients to gain clarity and confidence in managing their condition. For a deeper scientific understanding, consider exploring our comprehensive cancer biology resources here.
Causes and Risk Factors of Vulvar Cancer (Vulvar Carcinoma)
Understanding the contributory factors for Vulvar Cancer (Vulvar Carcinoma) is the first step towards prevention and health optimization. Several intertwined genetic, environmental, metabolic, and lifestyle elements significantly heighten the risk for developing Vulvar Cancer (Vulvar Carcinoma).
Genetic Risk Factors
Genetic alterations have a considerable role in cancer pathogenesis. Specific genetic patterns influencing Vulvar Cancer (Vulvar Carcinoma) development include vulnerability-like disruptions in tumor suppressor genes, such as TP53, and mutations affecting pathways relating to cellular proliferation and differentiation. While traditionally less studied than BRCA mutations in breast and ovarian cancers, genetic risk assessments and family histories can reveal essential insights for early screening.
Environmental and Infectious Risk Factors
Infection with high-risk Human Papillomavirus (HPV)—notably HPV-16 and HPV-18—remains a significant factor behind Vulvar Cancer (Vulvar Carcinoma). Studies indicate that patients with prior HPV infections are several-fold more likely to develop vulvar neoplastic conditions. Environmental variables also include chronic vulvar inflammation or conditions like lichen sclerosus, enhancing malignant transformation risk.
Lifestyle and Metabolic Risk Factors
Lifestyle choices have marked consequences in Vulvar Cancer (Vulvar Carcinoma) development:
- Smoking dramatically elevates vulvar carcinoma diagnosis probabilities due to immune suppression and inflamed tissues.
- Obesity and dietary habits influence hormonal balances and chronic inflammation, potentially catalyzing cellular changes towards malignancy.
- Poor diet and sedentary lifestyle significantly affect metabolic health, increasing glucose availability—leveraged by vulvar cancer cells through metabolic phenomena such as the Warburg effect.
Furthermore, the metabolic dependency of Vulvar Cancer (Vulvar Carcinoma) on glucose and other nutrients creates essential therapeutic targets. Nearly 50% of cancer types, including vulvar malignancies, depend decisively on glutamine metabolismes besides glucose for nucleotide synthesis and rapid growth, reflecting exciting therapeutic possibilities.
Asian and Hong Kong-specific Risks
Regional epidemiological studies highlight specific vulnerabilities in Hong Kong and wider Asian populations:
- Increasing prevalence of HPV infections and inadequate vaccination rates.
- Aging populations with rising incidence rates, especially among women aged 60 and above.
- A widespread stigma around discussing gynecological health, leading to delayed diagnoses.
Empowering regional populations through culturally-sensitive awareness campaigns and vigorous educational initiatives can significantly reduce vulvar carcinoma incidences. Engage proactively in community screening programs and regular gynecological check-ups.
Book a consultation today and utilize AllCancer’s cutting-edge diagnostic facility to assess your personalized risk precisely.
Symptoms of Vulvar Cancer (Vulvar Carcinoma)
Recognizing the early signs and symptoms of Vulvar Cancer (Vulvar Carcinoma) can play a crucial role in timely diagnosis and management. Although these symptoms might be subtle initially, being informed can significantly improve outcomes.
Common Symptoms in Early Stages:
- Persistent itching or irritation in the vulvar area.
- Abnormal bleeding unrelated to menstruation or menopause.
- A lump or bump on the vulva.
- Vulvar skin color changes, including redness or paleness.
- Pain or tenderness localized to the vulva.
- Burning sensation during urination.
Symptoms Related to Advanced Stages (Stage 3 and 4):
- Severe fatigue and weakness due to systemic impact.
- Swollen lymph nodes may appear in the groin region, reflecting regional metastasis.
- Significant vulvar ulcers or open sores that won’t heal even after continued treatments.
- Painful sexual intercourse (dyspareunia) indicating increased tumor burden.
- Pain radiating to adjacent pelvic or groin areas, suggesting invasive growth and nerve involvement.
- Chronic lower back or abdominal pain, reflecting deeper tissue infiltration.
- Unplanned substantial weight loss, typical in advanced malignancy stages.
- Leg swelling (lymphedema), as the tumor obstructs normal lymph fluid drainage.
These symptoms often directly represent underlying tumor biology. For instance, persistent itching signals chronic inflammation induced by malignant cells, while abnormal bleeding is associated with tumor infiltration disrupting regular blood vessels. Redness or ulcers on the vulvar skin can indicate uncontrolled proliferation and impaired tissue repair mechanisms, typical attributes of carcinoma progression.
It is imperative that anyone experiencing these symptoms promptly seeks professional medical evaluation. Early detection significantly improves prognosis and outcomes, allowing focused treatments such as surgery, chemotherapy, and innovative metabolic therapies, including our Nobel-backed 4D therapy which strategically targets cancer cells dependent on heightened glucose metabolism, commonly referred to as the Warburg effect.
To understand diagnostics further, please visit our detailed Diagnostics for Vulvar Cancer (Vulvar Carcinoma) page.
Stages of Vulvar Cancer (Vulvar Carcinoma) and Survival Rates
Knowing the stage of Vulvar Cancer (Vulvar Carcinoma) is fundamental to formulating an effective treatment approach. Stages are internationally classified based on size, regional involvement, and distant metastasis. The following directly reflects population-specific data and treatment outcomes relevant to Hong Kong and surrounding Asian regions.
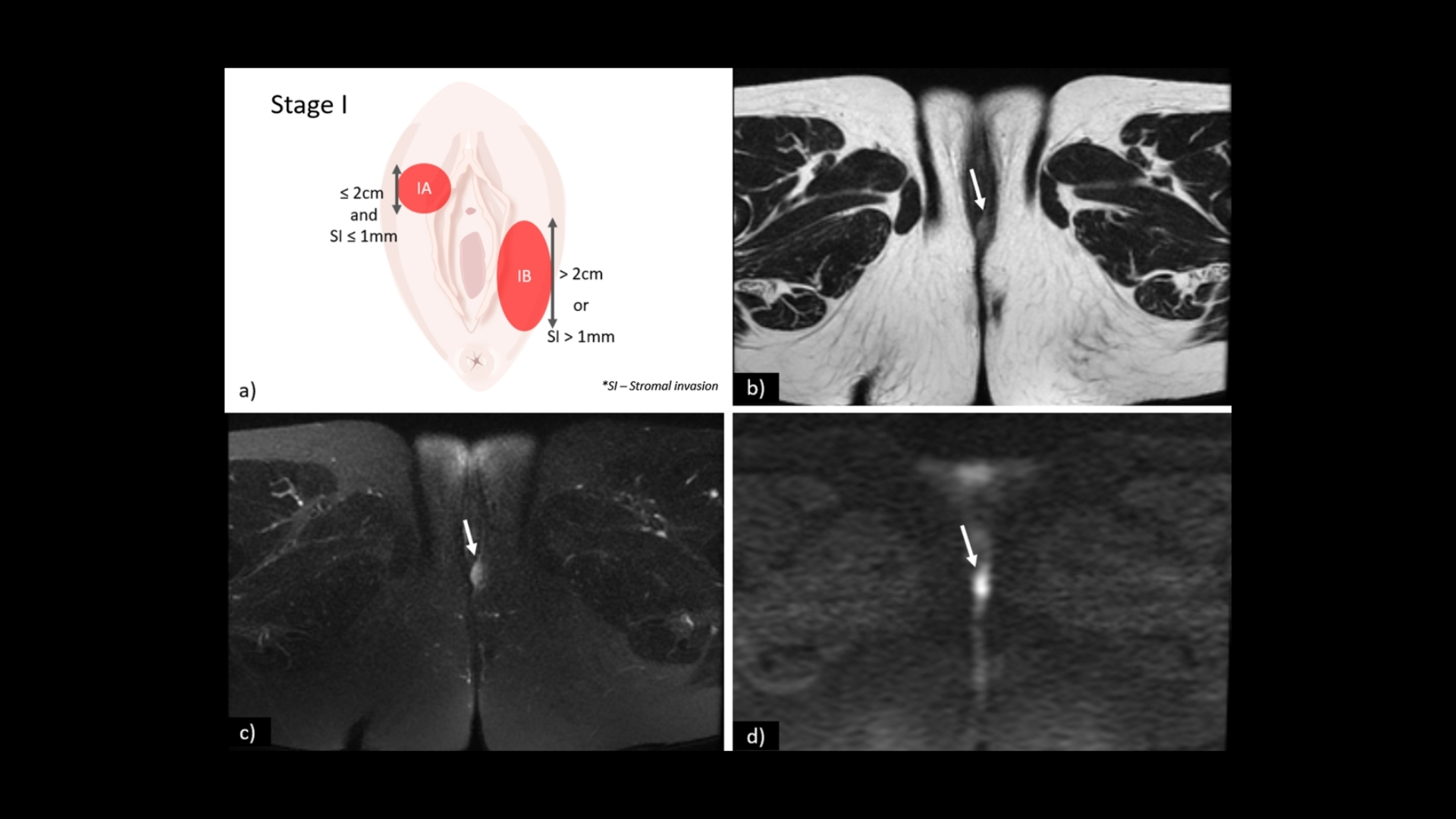
Stage 1 – Vulvar Cancer (Vulvar Carcinoma)
At Stage 1, the tumor is localized exclusively within the vulva, usually measuring below 2 centimeters in diameter.
- Tumor limited to the vulval skin or underlying tissue.
- No lymph node involvement or distant spreading observed.
- Treatment Options: Surgical excision, radiation, and a comprehensive approach integrating metabolic oncology.
- Outcome: More than 90% survival rate within five years, emphasizing the significance of early detection.
Stage 2 – Vulvar Cancer (Vulvar Carcinoma)
The tumor size typically expands and might affect nearby structures like the urethral or vaginal orifices but doesn’t yet involve lymph nodes or distant organs.
- Tumor invasive, but still localized to vulval region.
- Slight functional impairment may be present due to growing tumor.
- Treatment escalates to more aggressive surgical techniques, potentially combined radiation therapies, and adjuvant chemotherapy.
- Outcome: Survival rate stays robust, offering a 5-year survival of 70-85% with appropriate interventions.
Stage 3 – Vulvar Cancer (Vulvar Carcinoma)
In Stage 3, tumors have spread to nearby lymph nodes and regional structures within the pelvis or lower abdomen, reflecting a significant progression of disease.
- Local lymphatic invasion evident, impacting groin lymph nodes.
- Visible tumor enlargement or ulcerations with extensive skin migration.
- Treatment involves aggressive multimodality approaches involving surgical excision, radiation, chemotherapy, and introduction of advanced targeted metabolic therapies.
- Outcome: Survival probabilities moderate, implying meticulous management can achieve 5-year survival rates ranging from 50-70% based on regional treatment experience and technologies.
Stage 4 – Vulvar Cancer (Vulvar Carcinoma)
Stage 4 indicates distant metastasis to vital organs further from the original site, sometimes including lungs or liver involvement, posing significant management challenges.
- Distant metastases visible in organs like lungs, liver, bones, or brain.
- Extensive tumor spread markedly impairing quality of life due to severe functional consequences.
- Therapy shifts focus towards systemic-targeted approaches, integrating surgery with advanced chemotherapy regimens, and exploring novel therapeutic paradigms like metabolic targeting and immune modulation.
- Clinical innovations like 4D metabolic therapies, supported by groundbreaking Nobel laureate research, are increasingly relevant, transforming Vulvar Cancer management into a chronic disease scenario.
- Outcome: historically, a 20-30% survival rate over three years can be anticipated. Although still serious, advanced interdisciplinary management has gradually improved prognosis.
For comprehensive insights into treatment options available at each stage, do visit our specialized Treatment options for Vulvar Cancer (Vulvar Carcinoma) page.
Limitations of Traditional Therapies for Vulvar Cancer (Vulvar Carcinoma)
Chemotherapy and Its Associated Toxicities in Vulvar Cancer (Vulvar Carcinoma)
Chemotherapy, a cornerstone in traditional cancer management, aims to eliminate rapidly dividing vulvar cancer (vulvar carcinoma) cells by interfering with their division and growth processes. However, the systemic nature of chemotherapy means it also exerts a broad and often indiscriminate impact on healthy cells, leading to significant toxicities.
- Bone Marrow Suppression (78% risk): Chemotherapy for vulvar cancer dramatically affects hematopoietic stem cells within the bone marrow, greatly increasing susceptibility to infections, bleeding, and anemia due to reduced white cells, platelets, and erythrocytes.
- Cardiac Toxicity (23% risk): Many chemotherapeutic agents, particularly anthracyclines like doxorubicin routinely used in treatments across Asia, can significantly damage cardiac tissue leading to compromised heart function, arrythmias, and heart failure—burdening patients already dealing with cancer diagnosis.
- Fatigue and Nausea: Persistent chemotherapy-induced fatigue severely impacts quality of life, physical stamina, mental health, and social interactions. Furthermore, uncontrollable nausea and vomiting episodes often exacerbate nutritional deficiency in affected individuals.
- Secondary Cancer Risks (up by 300%, JAMA Oncology 2023): Alarmingly, chemotherapy increases long-term risk of developing secondary malignancies, creating a challenging healthcare scenario particularly pertinent in densely populated regions like Hong Kong.
Limitations Associated with Radiation Therapy for Vulvar Cancer (Vulvar Carcinoma)
Radiation therapy, often combined with chemotherapy for enhanced efficacy, similarly comes with severe limitations attributable mainly to radiation’s non-specific damage to surrounding healthy tissues.
- Tissue Damage and Scarring: Radiation therapy can lead to significant local tissue destruction due to inflammation-induced fibrosis, resulting in chronic pain, restrictive scarring, difficulties in urination, defecation, and negatively impacting sexual health and self-image.
- Dermatological Side Effects: Vulvar carcinoma patients treated with radiation frequently experience acute dermatitis and chronic skin atrophy, leading to diminished life quality and persistent discomfort.
- Increased Infection Risks: Radiotherapy compromises lymphatic drainage and normal skin barrier defenses, significantly elevating the risk of local and systemic infections. This issue is particularly problematic for elder populations frequently affected by vulvar carcinoma, common in Asian demographics with aging populations.
Surgical Challenges in Vulvar Cancer (Vulvar Carcinoma)
Surgical interventions represent another standard treatment approach for early stages of vulvar carcinoma. Nevertheless, surgical strategies present substantial drawbacks, particularly regarding extensive tissues removal and significant postoperative morbidities.
- High Infection Risks Post-Surgery: Extensive surgeries, especially vulvectomy and lymph node dissections, raise postoperative infection risks significantly. Such surgical interventions further require extensive antibiotic treatments and prolonged hospitalizations.
- Long-Term Functional Impairments: Surgical removal of vulvar tissues radically affects daily functions such as mobility, urinary and bowel functions, sexual activity, and considerably diminishes overall patient quality-of-life.
- Pain and Wound Healing Problems: Lingering chronic pain from nerve damage, common post-surgical complication, accounts for significant emotional and psychological distress among patients. Wound dehiscence and delayed healing cause prolonged recovery accessed commonly in Asian metropolitan healthcare centers, such as hospitals in densely populated Hong Kong.
Low Efficacy in Advanced-Stage Vulvar Cancer (Vulvar Carcinoma)
Traditional therapies demonstrate dramatically reduced effectiveness once the cancer metastasizes, substantially lowering potential for successful patient outcomes. Specifically, the objective response rate (ORR) drops starkly to less than 21% for advanced-stage vulvar cancers, significantly limiting therapeutic hopes for affected individuals and clinicians alike.
Studies conducted in Hong Kong highlighted further dismal prognosis statistics with remote areas experiencing even lower survival outcomes. Patients receiving conventional treatments report severely diminished health-related quality-of-life measures, considerable psychological distress, and limited therapeutic benefit, accentuating the critical demand for innovative treatment approaches.
Metabolic Resistance in Vulvar Cancer Cells
A growing concern within oncology practices pertains to cancer cell metabolism and resistance mechanisms that hinder effective treatment implementation. Cancer cells, including vulvar carcinoma cells, exhibit metabolic flexibility, significantly impeding traditional therapies’ effectiveness in eradicating malignancies completely.
- Enhanced Glucose Uptake and Warburg Effect: Vulvar cancer cells exhibit markedly increased glucose consumption (200-fold compared to normal cells), presenting limitations in conventional treatments which typically do not target metabolic vulnerabilities effectively.
- Increase in DNA Repair Enzyme Activity (400% increase): Vulvar carcinoma cells demonstrate alarming boosts in DNA repair enzymes following traditional chemotherapy or radiation exposure. This metabolic adaptation enables survival tactics, reducing sensitivity towards standard therapies, and elevating recurrence risks notably.
- Glutamine Dependency: Many vulvar carcinoma cells demonstrate a dependency on glutamine metabolism alongside the classic Warburg effect pathway. Traditional therapies do not target this dependency, thus providing opportunities for resistant cancer cells survival.
Regional Context and Challenges in Hong Kong and Asia
Asian regions such as Hong Kong particularly experience challenges exacerbating conventional treatments’ limitations. Limited healthcare resources, public healthcare system burden, aging population dynamics, and cultural factors prolong patient hesitations around accessing early care and complicating ongoing treatment management.
- Healthcare Resource Limitations: With increasing pressures on healthcare systems, facilities in Hong Kong report delays in diagnosis, lower patient follow-up compliance rates, and increased waiting periods for treatments, leading to poorer prognoses overall.
- Cultural and Societal Stigmas: Vulvar carcinoma presents particular sensitivities within Asian societies, leading to delayed diagnoses and advanced presentation stages. Such delay significantly impacts treatment effectiveness and curative prospects, heightening emotional and physical burdens patients experience.
Therefore, highlighting these critical limitations underscores an urgent global and regional healthcare imperative: the continued search and integration for improved therapies ideally addressing both biological vulnerability and patient quality-of-life—the precise promise held by innovative therapeutic breakthroughs.