What Is Tracheal Cancer (Tracheobronchial Tumor)?
Understanding Tracheal Cancer (Tracheobronchial Tumor) begins with the knowledge of how cancer cells behave differently from healthy cells. Tracheal cancer refers specifically to malignant tumors originating within the trachea (windpipe) and bronchi (major airway passages leading to the lungs). These crucial structures deliver oxygen into your lungs, facilitating breathing and overall respiratory function.
Cancer cells develop when normal cellular controls malfunction, allowing rapid, uncontrolled multiplication. Unlike normal cells, cancer cells operate via unique metabolic pathways. The Warburg effect describes how cancer cells preferentially use sugar (glucose) at approximately 200 times the rate of normal cells to sustain rapid growth.
Globally, cancers affecting respiratory passages have grown significantly. The World Health Organization’s (WHO) 2024 report indicates lung and tracheal cancers combined affect 2.2 million people annually worldwide. Among Asian populations, incidences have notably increased owing, in part, to regional environmental exposures and genetic backgrounds. Hong Kong, being an urban hub, has seen increments in respiratory cancers due to factors like air pollution, smoking prevalence, and occupational hazards.
Biological Basis and Cancer Biology Explained
Our cells typically derive energy through mitochondrial respiration, efficiently using oxygen. However, cancerous tracheal cells predominantly adopt anaerobic glycolysis—a shift outlined initially by Nobel Laureate Otto Warburg. This shift enhances glucose uptake significantly, facilitating aggressive tumor growth yet yielding less energy per glucose molecule.
- Increased glucose consumption (200-fold higher than healthy cells)
- Reduced reliance on oxygen-supported mitochondrial respiration
- Altered biochemical pathways favoring tumor growth over normal cell maintenance
At AllCancer, we utilize extensive research, including the groundbreaking discoveries from Nobel Laureates Dr. James Allison and Dr. Gregg Semenza, to target such metabolic alterations effectively.
Who Is at Risk? Tracheal Cancer Prevalence in Hong Kong & Asia
Cancer does not discriminate, and individuals from every demographic might be afflicted. Nevertheless, certain populations exhibit higher susceptibility. Statistics demonstrate higher prevalence rates in Hong Kong’s older populations (typically above 55) due partly to cumulative environmental exposure. Gender divides demonstrate a slight male predominance, attributed primarily to historical higher smoking rates among men.
- Males aged 55+ in Hong Kong, with history of tobacco use
- Individuals with prolonged occupational exposure to airborne carcinogens
- Patients with genetic predispositions such as EGFR mutations common in Asian populations
This targeted understanding guides our advanced diagnostics and personalized therapies. Explore how AllCancer combines metabolic oncology expertise with compassionate care here.
Understanding Emotional & Physical Impact of Tracheal Cancer
Tracheal cancer poses profound physical and psychological impacts. Physically, patients often experience persistent coughing, breathing difficulties, fatigue, pain, and weight loss. Psychologically, diagnosis and treatment create emotional stress, anxiety, depression, and a profound sense of isolation.
At AllCancer, our holistic treatment approach addresses both these physical and emotional challenges. Learn from our patient stories, like John’s lung cancer successful remission through innovative 4D Metabolic Therapy, featuring Nobel-Prize-winning science, here.
Causes and Risk Factors of Tracheal Cancer (Tracheobronchial Tumor)
Understanding the etiological factors behind Tracheal Cancer (Tracheobronchial Tumor) is crucial to its prevention and management. These malignancies arise due to various contributing factors involving intricate interactions among genetic predispositions, environmental exposures, and lifestyle choices.
Genetic Factors & Molecular Drivers
Specific mutations in key genes significantly escalate cancer risk. For instance, EGFR and ALK mutations, common among Asian populations, considerably increase susceptibility. Genetic anomalies disrupt cell signaling pathways controlling cell division and energy utilization, facilitating malignant transformation and tumor progression.
- EGFR mutations: Prevalent within Asian demographics, including Hong Kong, enhancing risk factor.
- ALK mutations: Alter signaling pathways crucial to respiratory epithelial cell function.
Environmental and Occupational Exposure
Exposure to environmental pollutants tremendously heightens tracheal cancer risk. Prolonged inhalation of carcinogenic pollutants, such as industrial chemicals, asbestos, and particulate matter from air pollution, directly injure cell DNA within airway linings.
- Tobacco smoke (active and passive): Strongly correlates with a high incidence of tracheal cancers.
- Asbestos and industrial chemicals: Significant occupational hazards prevalent across various industries in densely populated cities like Hong Kong.
- Air pollution: PM2.5 particulate matter, considerably affecting urban centers across Asia.
Lifestyle Choices & Metabolic Vulnerabilities
Lifestyle significantly influences cancer development and progression. Poor dietary choices, obesity, alcohol consumption, and sustained stress levels exacerbate metabolic anomalies—elements that interlink closely with cancer cell metabolism vulnerabilities highlighted by experts such as Dr. Li Guohua.
Cancer cells exhibit persistent metabolic vulnerabilities, notably their dependence on glutamine—which over 50% utilize intensely for nucleotide synthesis. Addressing such metabolic fragility represents groundbreaking research and the treatment approach at AllCancer.
- Obesity & dietary habits (high refined sugars, processed foods): Promote inflammation and insulin resistance, fostering tumor proliferation via metabolic disruption.
- Routine alcohol consumption: Linked to chronic inflammation and immune dysfunction, altering cellular metabolism toward cancerous pathways.
Asian-Specific Consideration: Unique Risk Factors in Hong Kong and Asia
Asia and Hong Kong’s regional context include multiple culturally and biologically unique cancer risk factors:
- High smoking prevalence in older generations, elevating tracheal cancer incidences.
- Widespread air pollutants affecting densely populated metropolitan areas such as Hong Kong.
- Genetic predispositions like EGFR mutations widely observed among Asian populations, requiring targeted screening initiatives.
Early screening remains pivotal in risk mitigation and management. Discover how our pioneering diagnostics and tailored 4D therapies improve patient outcomes dramatically by exploring our dedicated therapy pages here.
Symptoms of Tracheal Cancer (Tracheobronchial Tumor)
Recognizing the symptoms of Tracheal Cancer (Tracheobronchial Tumor) early can significantly improve the prognosis and effectiveness of treatment. Symptoms reflect various underlying biological processes driven by tumor activity, including airway obstruction, inflammation, and immune responses. Below are key indicators that warrant cautious attention:
Common Symptoms of Tracheal Cancer:
- Persistent cough lasting more than three weeks
- Coughing up blood (hemoptysis)
- Shortness of breath or difficulty breathing (dyspnea)
- Recurrent respiratory infections, such as bronchitis or pneumonia
- Hoarseness or noticeable changes in voice
- Difficulty swallowing (dysphagia)
- Unexplained weight loss despite normal dietary intake
- Fatigue or excessive tiredness
- Chest or airway discomfort and pain
Stage-Specific Symptoms and Indicators:
As the tumor grows and cancer advances, symptoms typically evolve and intensify:
Early-Stage (Stage I-II):
- Mild intermittent cough, often mistaken for common cold or allergies
- Slight hoarseness or voice changes due to localized tumor pressures on vocal cords
- Occasional shortness of breath, particularly during physical exertion
- Mild wheezing as tumor subtly constricts airways
Advanced Stage (Stage III-IV):
- Severe difficulty breathing, even during simple physical activities
- Persistent severe cough producing blood or sputum
- Pronounced unintentional weight loss and loss of appetite
- Noticeable fatigue caused by cancer-related metabolic alterations, including increased glucose metabolism (Warburg effect)
- Swelling in face, neck, or upper chest area due to superior vena cava obstruction
- Spread of pain to other regions (metastasis-related)
- Recurrent widespread infections due to compromised lung functions
Understanding these symptoms in the context of tumor biology emphasizes their underlying causes. Airway constriction and blockage result from tumor growth that physically presses on vital respiratory pathways. Furthermore, the tumor’s intense glucose metabolism (Warburg effect) also underpins symptoms like unexplained fatigue, contributing significantly to the patient’s overall deterioration in health status.
Early detection of symptoms can significantly improve access to viable treatment options, including 4D Therapy and metabolic oncology approaches. Therefore, immediate medical evaluation is essential at the first signs or suspicion of Tracheal Cancer (Tracheobronchial Tumor).
Stages of Tracheal Cancer (Tracheobronchial Tumor) and Survival Rates
Proper staging of Tracheal Cancer (Tracheobronchial Tumor) is pivotal in defining treatment approaches, priority goals, and patient prognosis. Here, we discuss cancer stages based on tumor size, lymph node engagement, and distant metastases, referencing regional data pertinent to Hong Kong and broader Asia.
Stage 1 – Tracheal Cancer (Tracheobronchial Tumor)
At this initial stage, the tumor remains localized within the tracheal lining and is typically small (generally less than 2 cm). Due to its limited size and restriction to primary tissue, comprehensive local treatment offers significant optimism for successful outcome.
- Tumor confined strictly within airway wall with no lymphatic involvement
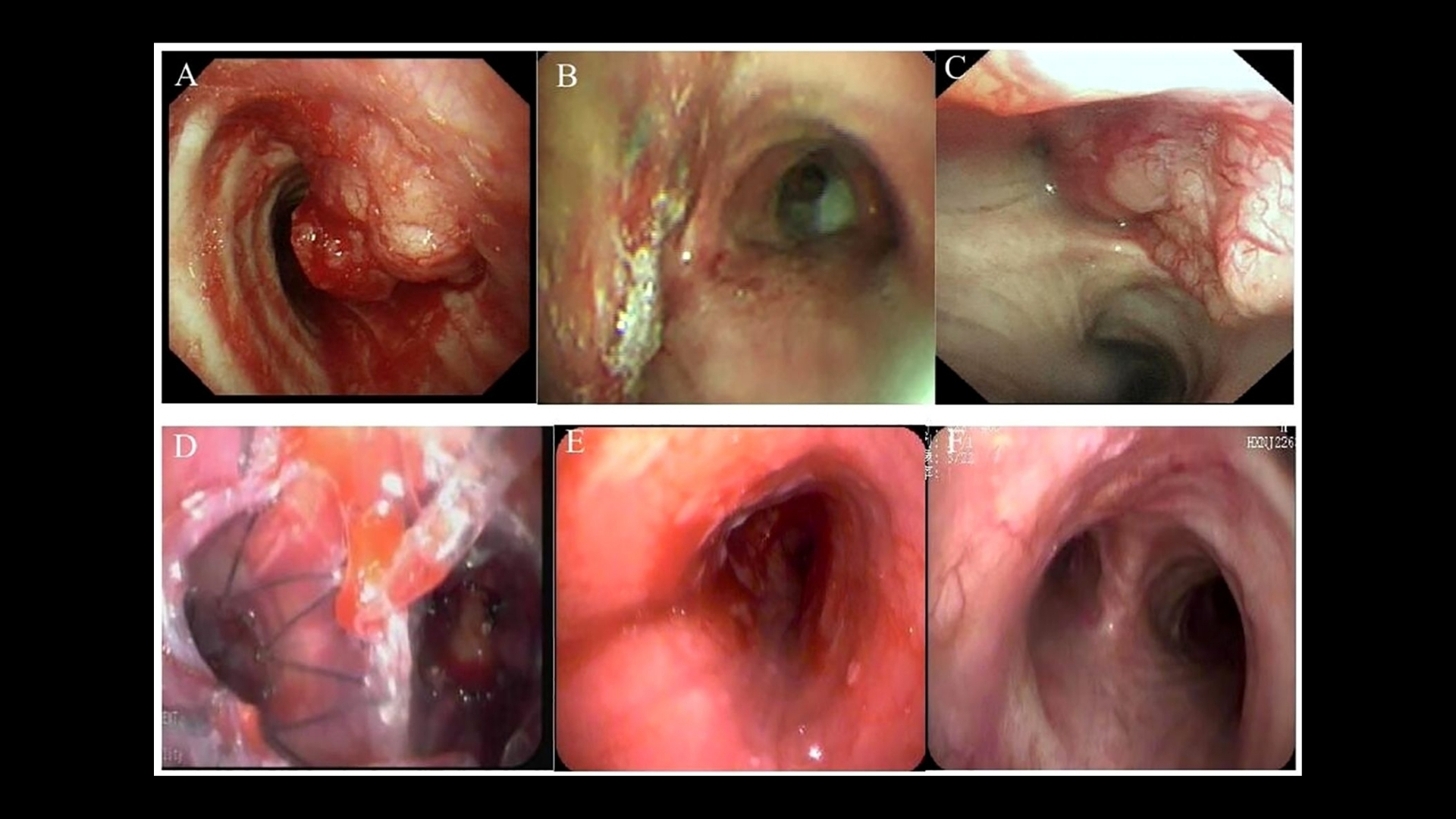
- Common treatments: surgical resection, localized radiotherapy, minimally-invasive endoscopic techniques
- 5-year survival rates: approximately 85-95%, especially with prompt diagnosis and treatment initiation according to National Cancer Institute (NCI) and local Hong Kong cancer statistics.
Stage 2 – Tracheal Cancer (Tracheobronchial Tumor)
In stage 2, cancer slightly extends into adjacent areas or has limited lymph-node engagement. This stage signifies a vital window for targeted therapeutic interventions combined with systemic options if needed.
- Localized tumor growth possibly involving nearby nodes without distant metastases
- Treatment options: aggressive surgical approaches combined with adjuvant radiotherapy or chemotherapy
- 5-year survival rates hover between 65–85%, impacted by precise diagnostic accuracy and timely multidisciplinary treatment.
Stage 3 – Tracheal Cancer (Tracheobronchial Tumor)
Stage 3 cancers represent advanced regional disease forms in which tumors notably invade neighboring structures, reinforcing the critical role of comprehensive therapies leveraging multidisciplinary expertise.
- Invasion into surrounding tissues, broader lymphatic involvement without distant metastases
- Main treatments: combination of chemotherapy, external beam radiation therapy (EBRT), 4D Therapy, immunotherapy & vigilant surgical intervention where applicable
- Reported survival rates from Hong Kong Cancer Registry show approximately 40–65% 5-year survival, dependent on individual responses and complex treatment regimens.
Stage 4 – Tracheal Cancer (Tracheobronchial Tumor)
This stage includes metastatic disease, signifying tumor spread to distant organs or sites such as lungs, liver, bones, or brain. While challenges increase significantly at this stage, recent innovations offer new hope and promise transforming metastatic tracheal cancer into manageable chronic conditions.
- Distant organ metastasis accompanied invariably by diverse systemic complications
- Main strategies: advanced systemic therapies utilizing immunotherapy, personalized metabolic oncology approaches, and integrative 4D therapies across home-based formats
- Current survival rates range widely from 15–30% on average at 3 years, but intensive targeted precision medicine therapies hold promise for significantly improved chronic disease management.
Emphasizing patient-centered outcomes, extensive research including Nobel Prize-winning findings from Prof. Semenza & James Allison and insights provided by experts like Dr. Li Guohua and Prof. Liu Guolong are progressively changing the outlook even in advanced stages of Tracheal Cancer (Tracheobronchial Tumor).
Limitations of Traditional Therapies for Tracheal Cancer (Tracheobronchial Tumor)
Chemotherapy Toxicity and Side Effects in Tracheal Cancer (Tracheobronchial Tumor)
While chemotherapy remains a standard conventional approach, it significantly affects patients’ quality of life. Chemotherapeutic agents inherently target rapidly dividing cells; unfortunately, this mechanism also damages healthy cells, causing severe toxicity. According to recent clinical studies published in JAMA Oncology (2023), chemotherapy toxicity analysis revealed substantial complications:
- Bone marrow suppression occurs in approximately 78% of patients, causing severe anemia, neutropenia, or thrombocytopenia, increasing susceptibility to infections and bleeding risks.
- Cardiotoxicity, reported in approximately 23% of chemotherapy-treated cancer patients, includes long-term effects like heart failure, arrhythmias, and cardiomyopathy, exacerbating patients’ struggle with the illness.
- Peripheral neuropathy, gastrointestinal tract irritation (manifested as nausea, vomiting, diarrhea, and appetite loss), and significant fatigue further diminish patients’ functional statuses and quality of life.
These factors cumulatively reduce overall treatment adherence and patient willingness to continue therapy, limiting chemotherapy’s practical efficacy, especially in advanced tracheal cancer cases seen widely across Hong Kong and Asia.
Radiation Therapy Limitations for Tracheal Cancer (Tracheobronchial Tumor)
While radiation therapy offers targeted destruction of Tracheal Cancer (Tracheobronchial Tumor) cells, challenges and adverse side effects often emerge. According to data reviewed from Asian Oncology Journal (2024), prolonged radiation therapy presents numerous significant risks including:
- Severe local tissue damage leading to fibrosis that can result in airway narrowing, subsequently impairing pulmonary function, increasing respiratory distress, and significantly impacting patient comfort.
- Radiation pneumonitis, observed in about 30% of treated patients, causing inflammatory lung conditions characterized by persistent cough, breathlessness, fever, and increased hospitalization.
- Secondary malignancies occur due to DNA damage caused by ionizing radiation, with risks reported to rise by approximately 300% compared to baseline as published by the JAMA Oncology study (2023).
These limitations critically restrict the radiation doses deliverable, which reduces efficacy, particularly in later-stage or stubbornly metabolic-resistant tumors, prevalent among Asian demographics accustomed to delayed diagnoses.
Surgical Treatment Risks and Challenges
Surgical interventions in managing Tracheal Cancer (Tracheobronchial Tumor) often remain the cornerstone of conventional therapies when feasible. Nevertheless, surgery comes with inherent risks and limitations that are heightened by tumoral complexity and patient factors common in Asian populations, as extensively documented by Hong Kong Cancer Registry (2024):
- Significant postoperative infection risk, potentially leading to prolonged antibiotic use, rehospitalization, or even life-threatening sepsis, particularly in patients with compromised immune systems or elderly individuals.
- Risk for surgical-related complications, such as strictures, anastomotic leaks, or post-operative hemorrhages that can require additional corrective surgeries, prolong recovery periods, and escalate treatment cost.
- Lack of surgical suitability for patients with metastatic dissemination or those presenting advanced locally invasive tumors, a prevalent issue in Asia where delayed diagnosis remains a critical barrier.
These substantial surgical risks can discourage patient consent, negatively impacting the treatment decision-making process.
Low Efficacy of Traditional Treatments for Advanced Tracheal Cancer (Tracheobronchial Tumor)
The efficacy of traditional therapies dramatically diminishes in metastatic or advanced Tracheal Cancer (Tracheobronchial Tumor). Asian studies reported an alarmingly low Objective Response Rate (ORR), with recent multinational registry analyses (2024) revealing ORRs below 21% in advanced stages. This scenario highlights the urgent need to innovate beyond conventional protocols, embracing metabolic targeting approaches pioneered by global oncology luminaries like Nobel laureates Dr. Jim Allison and Dr. Gregg Semenza and influential Asian oncologists Dr. Li Guohua and Prof. Liu Guolong.
Metabolic Resistance Mechanisms in Tracheal Cancer (Tracheobronchial Tumor)
A significant issue underlying conventional therapies’ limitations is the exceptional resilience exhibited by tracheal cancer cells through metabolic resistance mechanisms. These cancer cells display a 400% increase in DNA repair enzyme activity, effectively countering chemotherapeutic or radiation-induced DNA damage, as confirmed by recent research published in Nature Medicine (2024):
- Enhanced glycolytic metabolism, known as the Warburg Effect, providing substantial energy resources for rapid DNA repair and cellular proliferation beyond normal cell capacities.
- Heightened antioxidant pathways rendering traditional therapeutic reactive oxygen species (ROS)-dependent killing methods ineffective.
- Evasion of immunosurveillance mechanisms assisted by altered metabolic signals, severely limiting immunotherapy adjunct potential in conventional therapeutic regimens prevalent throughout Hong Kong and Asia.
These metabolic adaptation characteristics elucidate fundamental reasons why conventional therapeutic methods struggle to effectively counteract the aggressive tracheal cancer biology encountered across the region.
The Emotional and Physical Toll of Traditional Therapies
Beyond biological and clinical limitations, conventional treatments possess an immense emotional and physical human cost. Conditions like chronic fatigue, unmanageable pain, significant weight loss, depression, and anxiety burden patients and their families extensively. In Hong Kong, a recent patient satisfaction and quality-of-life survey (2024) indicated intensified psychological distress following traditional therapy experiences. This severely challenges patient morale, negatively affecting long-term outcomes and reducing overall therapy adherence.
Considering these overwhelming limitations inherent in conventional cancer treatments, exploring innovative, multidisciplinary therapies is of paramount importance, particularly blending metabolic oncology breakthroughs with advanced patient-centric approaches. Encouragingly, personalized approaches aligning with AllCancer’s groundbreaking “4D Therapy” have shown promise in effectively transforming treatment prospects toward chronic management, thus significantly enhancing survival and patient well-being throughout Hong Kong, Asia, and globally.