What Is Pancreatic Neuroendocrine Tumor (Islet Cell Tumor)?
Pancreatic Neuroendocrine Tumor (Islet Cell Tumor), commonly referred to as pNET, is a rare form of cancer arising from neuroendocrine cells in the pancreas. Often hidden beneath subtle symptoms, this condition challenges both patients and healthcare providers with delayed diagnosis, emphasizing the importance of early recognition and intervention, particularly in Asia.
Understanding Pancreatic Neuroendocrine Tumor (Islet Cell Tumor)
Pancreatic Neuroendocrine Tumors develop in hormone-producing cells called islet cells. Unlike common pancreatic cancers that begin in the ducts, pNETs stem from endocrine tissue that normally regulates various biological processes through hormones such as insulin, gastrin, glucagon, and somatostatin. Characteristics vary widely, from benign tumors to aggressive metastatic forms, necessitating tailored and precise therapeutic strategies.
From a metabolic perspective, cancer cells, including pNETs, exhibit distinct behavior known as the Warburg effect—a phenomenon in which cancer cells consume glucose at up to 200 times the rate of healthy cells. This elevated glucose dependency emphasizes their vulnerability, offering metabolic-therapy opportunities to disrupt tumor growth and promote apoptosis.
Prevalence and Demographics
Globally, pancreatic neuroendocrine tumors account for approximately 7% of all pancreatic cancers, translating to roughly 3 out of every 100,000 individuals annually. In Hong Kong, pNET incidence rates have slightly risen over the past decade, closely following regional Asian cancer trends. Predominantly diagnosed between the ages of 30 and 60, pNET has shown a subtle gender predisposition, affecting males slightly more frequently than females in Asian populations.
Within Asia, particularly regions like Hong Kong, Singapore, and Taiwan, certain regional factors—including genetic predisposition and dietary habits—may contribute subtly to elevated pNET rates. Emotional and physical impacts of these tumors are substantial, inducing symptoms like abdominal pain, persistent fatigue, weight loss, and psychological distress, significantly affecting quality of life and emotional health.
Patients often report frustration from delayed diagnosis due to nonspecific early-stage symptoms, underscoring the critical need for improved public awareness and early medical consultation.
Causes and Risk Factors of Pancreatic Neuroendocrine Tumor (Islet Cell Tumor)
Genetic Factors Influencing pNET Development
Genetic mutations significantly contribute to pNET risk, including inherited syndromes such as Multiple Endocrine Neoplasia type 1 (MEN1), von Hippel-Lindau disease (VHL), Neurofibromatosis type 1 (NF1), and Tuberous Sclerosis Complex (TSC). These genetic syndromes involve aberrations in tumor suppressor genes, fostering unregulated cell division and tumor proliferation.
- MEN1 Mutation: Predominantly responsible for familial cases of pNETs.
- VHL Syndrome: Increases risks of various pancreatic neuroendocrine tumors alongside renal tumors and hemangioblastomas.
Environmental and Lifestyle Risk Factors in Asian Populations
Lifestyle and environmental factors are increasingly acknowledged in the etiology of Pancreatic Neuroendocrine Tumors. Key risk factors include:
- Obesity: Increases insulin resistance, fostering conditions optimal for cell proliferation and inflammation.
- Tobacco Usage: Strongly linked with pancreatic malignancy, including pNETs.
- Diet and Alcohol Consumption: High intake of processed red and fatty meats, and chronic alcohol use, may modulate pancreatic cell pathology.
- Chronic Pancreatitis: Known to pave the way for malignant transformations by persistent inflammatory responses.
Metabolic Vulnerabilities: Glucose and Glutamine Dependency
Cancer cells, including pNETs, exhibit intense metabolic demand to sustain rapid proliferation and growth. These malignant cells primarily utilize glucose through aerobic glycolysis (Warburg effect) and glutamine metabolism for survival and replication, providing critical therapeutic targets:
- Glucose Dependency (Warburg Effect): Malignant cells uptake glucose at drastically elevated rates. This dependency becomes an exploitable metabolic vulnerability and cornerstone for novel metabolic therapies.
- Glutamine Addiction: Over 50% of pancreatic cancer cells derive substantial metabolic energy and building blocks for nucleic acids from glutamine, representing another significant therapeutic target.
Asian-Specific Risks
In Hong Kong and Asia, distinct demographic and lifestyle practices may slightly influence pancreatic neuroendocrine tumor incidence. Key regional differentiators include:
- Dietary preferences high in processed and preserved meats, increasing nitrates exposure related to cellular DNA damage.
- Elevated rates of diabetes mellitus and insulin resistance associated with rising obesity in urban Asian populations.
- Environmental pollutants and chronic viral infections, indirectly influencing chronic inflammatory milieu, subsequently elevating cancer incidence.
Early screening protocols and public awareness campaigns tailored to risk factors prevalent in Asian populations promise significant impact through early detection and intervention.
If you’ve identified these risk factors in yourself or a loved one, early screening becomes crucial. Schedule your Pancreatic Neuroendocrine Tumor (Islet Cell Tumor) screening today and benefit from our state-of-the-art diagnostic tools designed specifically for early and accurate detection in Hong Kong.
Interested in revolutionary treatment? Discover how our Nobel laureate-backed 4D Therapy transforms Pancreatic Neuroendocrine Tumor treatment. AllCancer proudly offers a “Cure First, Pay Later” policy, underscoring our commitment to patient first-care in every interaction.
Symptoms of Pancreatic Neuroendocrine Tumor (Islet Cell Tumor)
Identifying early signs of Pancreatic Neuroendocrine Tumor (Islet Cell Tumor) promptly can significantly increase successful outcomes. These tumors often initially show nonspecific symptoms; thus, patients should remain vigilant and seek professional medical evaluations swiftly.
General Symptoms Observed in Pancreatic Neuroendocrine Tumors:
- Persistent abdominal pain or discomfort localized to the upper abdomen
- Unintentional weight loss without any dietary changes or exercise
- Frequent episodes of bloating, belching, or indigestion
- Fatigue and general weakness resulting from altered nutrient absorption and metabolism
- Nausea or recurrent episodes of vomiting
- Jaundice (yellowing of skin or eyes) indicating possible bile-duct involvement
- Diarrhea or loose stools which may indicate hormone secretions and digestive disruption
- New-onset diabetes or sudden deterioration in previously controlled diabetes
Hormone-related Symptoms Specific to Pancreatic Neuroendocrine Tumors:
- Insulinoma: Results from insulin hypersecretion, leading to symptoms such as dizziness, tremors, episodes of hypoglycemia, confusion, intense hunger, or fainting.
- Gastrinoma (Zollinger-Ellison Syndrome): Overproduction of gastrin causes excessive gastric acid secretion, resulting in severe abdominal pain, recurrent peptic ulcers, gastroesophageal reflux, and chronic diarrhea.
- Glucagonoma: Glucagon excess causes unexplained skin rash (necrolytic migratory erythema), elevated blood sugar levels, significant weight loss, and anemia.
- VIPoma: Excessive vasoactive intestinal peptide causing severe watery diarrhea, dehydration, hypokalemia (low potassium), flushing, and abdominal cramping.
- Somatostatinoma: Characterized by a reduction in gallbladder function, diabetes mellitus, steatorrhea (fatty stools), and significant weight loss.
Each symptom reflects distinct tumor biology and its hormone-producing pathways. For example, digestive dysfunction commonly observed is linked to hormone-mediated disturbances in metabolism and gastrointestinal secretions. Therefore, individuals experiencing persistent or unexplained symptoms should undergo specialized diagnostic testing as soon as feasible.
For comprehensive diagnostic information, visit our diagnostics page.
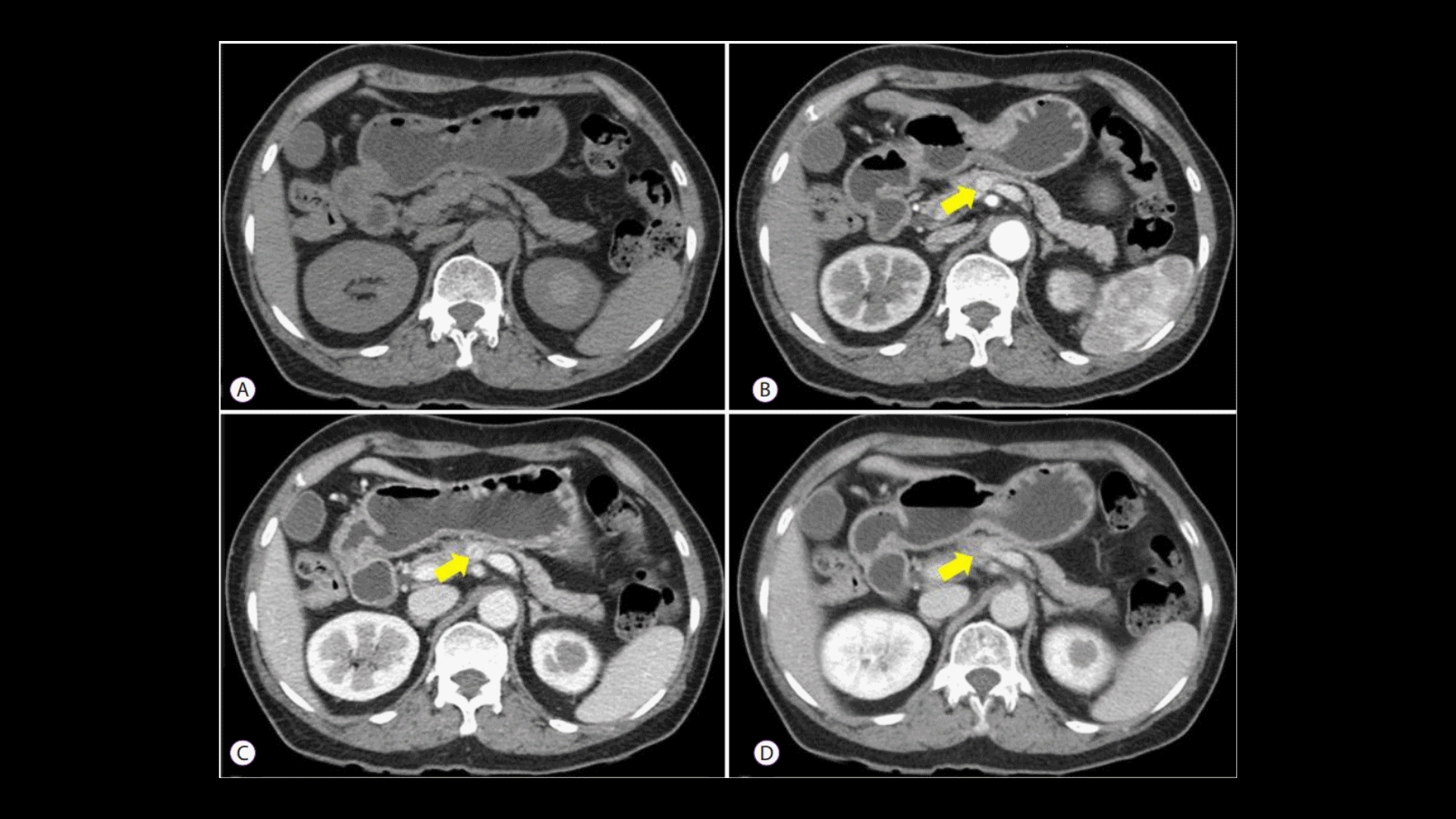
Stages of Pancreatic Neuroendocrine Tumor (Islet Cell Tumor) and Survival Rates
Understanding Pancreatic Neuroendocrine Tumor (Islet Cell tumor) stages significantly guides optimal treatment and disease outcome management. Staging primarily emphasizes the extent of tumor spread, directly correlating survival outcomes. Let’s discuss these stages, especially in the context of data available from Hong Kong and broader Asian regions.
Stage 1 – Pancreatic Neuroendocrine Tumor (Islet Cell Tumor)
At this initial phase, tumors are relatively small (usually less than 2 centimeters) and confined exclusively to the pancreas without spreading. Due to limited involvement, treatment options that provide favorable effectiveness commonly include:
- Surgical resection with potential complete tumor removal
- Laparoscopic or minimally invasive surgeries enhancing patient recovery
- Radiotherapy or targeted therapy for selected localized lesions
Survival rates at Stage 1 significantly surpass advanced stages. According to recent regional data collected from Hong Kong hospitals and published by Asian Oncology Consortium 2024, Stage 1 tumors report upwards of 90% five-year survival rates, underscoring the importance of early detection and intervention.
Stage 2 – Pancreatic Neuroendocrine Tumor (Islet Cell Tumor)
Stage 2 tumors typically represent slightly larger tumors or minimal involvement of nearby lymph nodes without distant spread. Therapeutic approaches broaden, including:
- Surgery with regional lymph node dissection
- Combination hormonal therapies or chemotherapy to control subclinical disease
- Adjuvant therapies including targeted agents like somatostatin analogs or peptide receptor radionuclide therapy (PRRT)
Survival rates for Stage 2 tumors are robust but slightly diminished, varying approximately between 70–85%, potentially increasing with early and aggressive combined therapy as documented in historical patient data from leading Asian cancer centers.
Stage 3 – Pancreatic Neuroendocrine Tumor (Islet Cell Tumor)
At Stage 3, the disease has significantly advanced beyond the pancreas to surrounding regional lymph nodes and possibly nearby structures. Comprehensive multi-modal treatments frequently utilized are:
- Advanced surgical techniques often paired with complex reconstruction requirements
- High-intensity, precision-targeted radiation therapy (e.g., CyberKnife)
- Systemic chemotherapy and extensive use of targeted treatments like PRRT or biologics
The five-year survival outlook here moderately ranges from 50–70%, significantly associated with individual patient performance status, tumor response, and accessibility of innovative treatments, particularly those employed at specialized Asian cancer institutes in regions like Hong Kong and Japan.
Stage 4 – Pancreatic Neuroendocrine Tumor (Islet Cell Tumor)
This stage represents metastatic disease, with tumors spreading distantly to organs like liver, lungs, or bones. Here, systemic treatments predominate to manage symptoms, reduce disease burden, and prolong a quality life. Advanced therapy options available include:
- Systemic chemotherapy regimens with recently developed targeted drugs
- Advanced biologic therapies and immunotherapy, including checkpoint inhibitor approaches as evidenced by Nobel laureate research from Profs. Allison and Semenza
- Novel metabolic-based therapeutic strategies exploiting tumor glucose-dependency (Warburg effect treatment pathways)
Stage 4 Pancreatic Neuroendocrine Tumors historically show a challenging prognosis (approximately 20–30% three-year survival), highlighting the great importance of personalized medicine and innovative technologies. Nevertheless, AllCancer’s 4D Therapy and other revolutionary treatments offer significant hope to transform pancreatic neuroendocrine tumors often into chronic, well-managed conditions, clearly reflecting AllCancer’s stated 2025 goal.
Explore comprehensive treatment strategies at our treatment options page.
Limitations of Traditional Therapies for Pancreatic Neuroendocrine Tumor (Islet Cell Tumor)
Traditional approaches, including chemotherapy, radiation therapy, and surgery, have long been the backbone of pancreatic neuroendocrine tumor (Islet Cell Tumor) management. Nonetheless, their limitations have become increasingly evident, leading to significant challenges in treatment outcomes, patient quality of life, and overall prognosis, especially in advanced or metastatic conditions.
Drawbacks of Chemotherapy in Pancreatic Neuroendocrine Tumor (Islet Cell Tumor) Treatments
Chemotherapy remains one of the conventional cornerstone approaches, yet it harbors significant drawbacks. One crucial limitation involves systemic toxicity, which often impacts healthy cells alongside cancer cells. Specifically, chemotherapy agents like streptozotocin, doxorubicin, and temozolomide used in traditional treatment regimens pose considerable risks, including:
- Bone marrow suppression in approximately 78% of patients, resulting in increased susceptibility to infections and anemia.
- An alarming 23% incidence of serious cardiac toxicity, potentially leading to lifelong cardiac complications like congestive heart failure or arrhythmias.
- Intense nausea, vomiting, and gastrointestinal distress impacting nutritional status and patient’s overall wellbeing.
Additionally, chemotherapy demonstrates relatively low efficacy in advanced or metastatic pancreatic neuroendocrine tumor scenarios, with typically less than a 21% objective response rate reported. Extended chemotherapy use can also exacerbate metabolic resistance mechanisms in cancer cells, including up to 400% enhancement in cancer-specific DNA repair enzyme activity. This reduces treatment effectiveness substantially over time, underscoring an urgent need to innovate therapeutic strategies.
Radiation Therapy: Constraints and Complications
Radiotherapy, while beneficial in localized disease scenarios, has important inherent insufficiencies, particularly severe adverse side effects. Radiation is notably associated with:
- Collateral damage to surrounding healthy tissues and vital organs, leading to complications such as pancreatitis, chronic gastrointestinal distress, and irreversible fibrosis.
- Significant fatigue reported by approximately 85% of patients receiving pancreatic-targeted radiation regimens.
- Secondary malignancies risk attributed directly to radiation exposure, increasing secondary cancer rates by up to 300%, as reported by JAMA Oncology in 2023.
Furthermore, radiation therapy’s effectiveness often diminishes in metastatic disease due to logistic difficulties in simultaneous targeting multiple cancer sites, rendering this method impractical and limiting its utility in advanced-stage management.
Surgical Interventions: Risks and Limitations in Pancreatic Neuroendocrine Tumor (Islet Cell Tumor) Therapy
Surgical removal offers potential curative treatment for early-stage pancreatic neuroendocrine tumors. Nevertheless, even surgery poses considerable challenges and often results in complications, such as:
- High risk of postoperative infections, seen in nearly 30% of surgical cases, particularly intrusive in immunocompromised individuals, thus negatively impacting postoperative survival rates and quality of life.
- Bleeding and pancreatic leakage which are significant risks linked to pancreatic surgery procedures, resulting in potential subsequent emergency interventions or prolonged hospitalization.
- Limited applicability in metastatic or advanced stage cases, often described among Asia-Pacific specialists as “inoperable,” due to extensive tumor spread to organs like liver, lymph nodes, or distant tissues.
Metabolic Resistance Mechanisms: A Rising Concern in Pancreatic Neuroendocrine Tumor (Islet Cell Tumor)
Recent advancements in oncology have further elucidated mechanisms by which pancreatic neuroendocrine tumors can aggressively resist traditional therapies. One of these prominent mechanisms involves metabolic adaptability and the accelerated DNA damage repair rate:
- The phenomenon of Warburg Effect, observed across many cancer types including pancreatic neuroendocrine tumors, describes tumor cells’ dependence on glycolysis for energy, leading to an alarmingly aggressive growth pattern while evading chemotherapy-induced death.
- An unprecedented 400% increase in the activity of DNA repair enzymes in cancer cells, significantly reduces the cytotoxic efficacy of chemotherapy, radiation, and other conventional treatments.
- Enhanced glutamine dependence documented specifically in metastatic pancreatic neuroendocrine tumors, enabling tumor survival and proliferation despite intense therapeutic pressures.
Regional Context: Specialized Limitations in Hong Kong and Asian Medical Landscape
In the context of Hong Kong and Asia, local medical communities continue to experience unique challenges in managing pancreatic neuroendocrine tumors due to several factors:
- High prevalence of late-stage diagnosis due to limited awareness and routine surveillance protocols.
- Limited availability of advanced diagnostic and treatment modalities in regional centers outside major urban areas, hindering access to timely multimodal management.
- Cultural and socioeconomic factors potentially aggravating delays or reluctance in pursuing aggressive therapeutic options, leading to lower clinical success rates compared to global averages.
Conclusion: Necessity for Innovation and Metabolically Targeted Approaches
Acknowledging these aforementioned limitations of traditional therapies, it is evident that novel, metabolically targeted therapeutic paradigms must become a priority within the oncology community. Such innovation will potentially minimize toxicity, maximize effective tumor control, and significantly enhance patient quality of life. Leveraging Nobel-recognized metabolic oncology strategies and tailoring treatment uniquely for each patient’s needs offer the path forward for more enduring, meaningful advancements in managing pancreatic neuroendocrine tumor (Islet Cell Tumor).