What Is Pheochromocytoma?
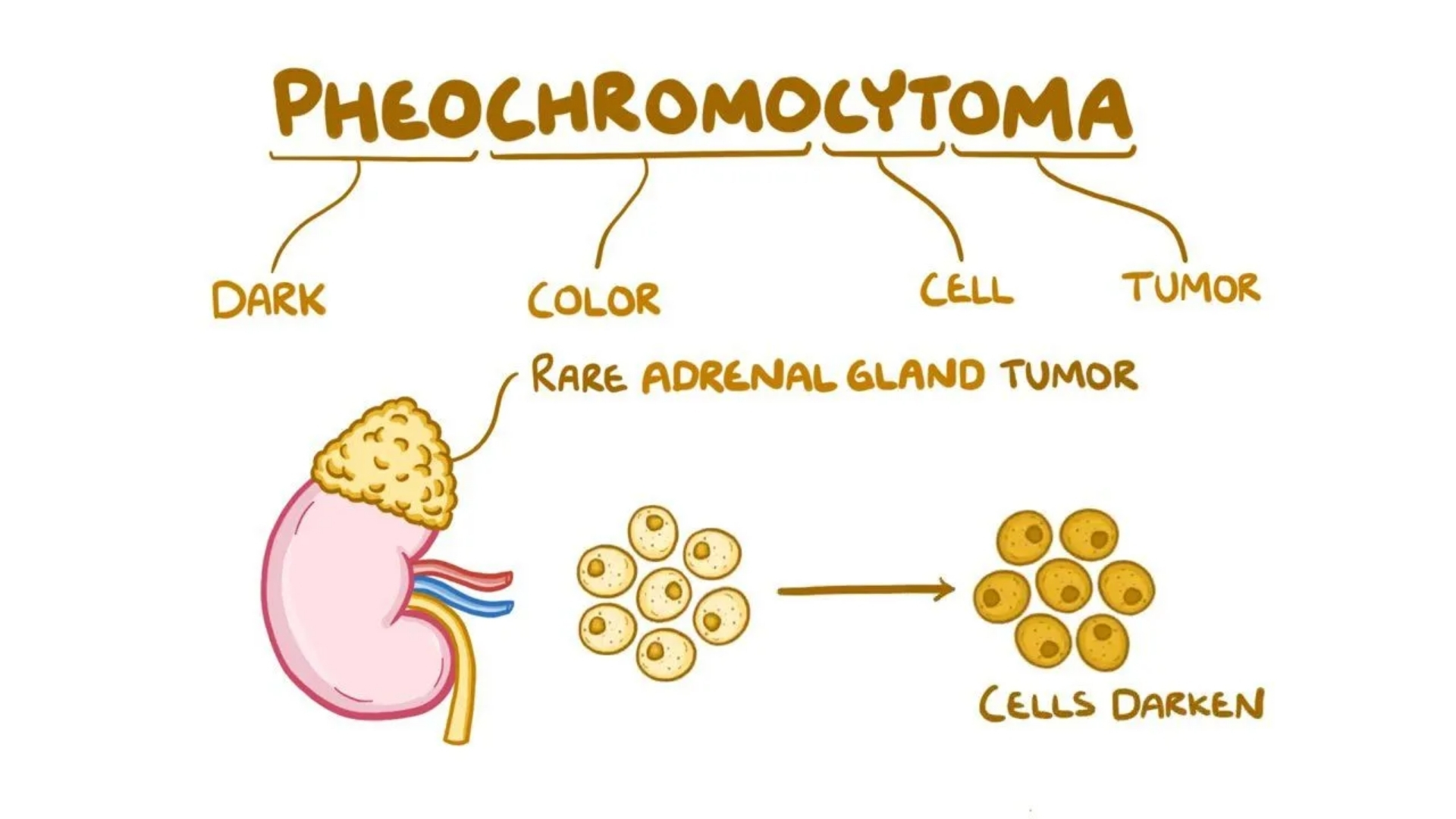
Pheochromocytoma is a rare neuroendocrine tumor originating from chromaffin cells in the adrenal glands. These cells are responsible for hormone release, particularly adrenaline and noradrenaline, affecting blood pressure, metabolism, and overall body function. Typically benign, around 10-20% are malignant cases. Understanding Pheochromocytoma is crucial, as this tumor significantly impacts patient quality of life with persistent hypertension, anxiety, and metabolic disturbances.
Biological evidence shows that cancer cells, including those in Pheochromocytoma, exhibit unique metabolic characteristics like the Warburg effect. This phenomenon describes how cancer cells consume glucose at rates over 200 times higher than normal cells, producing energy even under oxygen-rich conditions. Such metabolic vulnerabilities present innovative opportunities for targeted metabolic treatments, enhancing patient outcomes substantially.
Globally, Pheochromocytoma is rare, affecting about 0.2 to 0.8 per 100,000 individuals yearly, according to WHO’s 2024 data. However, this condition bears significant regional implications, particularly in densely populated regions such as Hong Kong and wider Asia, where diagnostic delays and misinterpretations of symptoms can heavily influence prognosis and patient outcomes.
In Asia, including Hong Kong, factors such as genetic predispositions linked to specific hereditary syndromes like multiple endocrine neoplasia (MEN2), von Hippel-Lindau syndrome (VHL), neurofibromatosis type 1 (NF1), and SDH gene mutations heighten Pheochromocytoma risks. Additionally, stress, dietary habits, and lifestyle changes prevalent in densely populated urban centers further compound the emotional and physical toll on patients.
Patients living with Pheochromocytoma often endure severe fatigue, headaches, rapid heart rate, hypertension crises, and profound psychological burdens such as anxiety or depression. Compassionate and comprehensive patient care remains paramount, aiming to manage symptoms, improve quality of life, and facilitate hopeful outcomes.
- Common symptoms: headache, sweating, racing heartbeat, anxiety, high blood pressure.
- Affected populations: typically diagnosed in adults aged between 30-60 years, equally affecting males and females, with slight geographical variations.
- Implications in Hong Kong: Emphasis on early diagnosis and effective management due to high-stress urban environments.
For further insights and expert diagnostics of Pheochromocytoma at AllCancer, discover our advanced metabolic oncology methods pioneered by acclaimed specialists like Dr. Li Guohua and Prof. Liu Guolong. Explore our Core Therapies Today.
Causes and Risk Factors of Pheochromocytoma
Understanding the causes and risk factors is essential for early identification and effective management of Pheochromocytoma. Several genetic and environmental elements significantly contribute to this cancer’s onset, impacting individual susceptibility.
Genetic Causes and Familial Syndromes
Approximately 30-40% of Pheochromocytoma cases have hereditary links to genetic conditions. Genetic mutations in RET, VHL, NF1, or SDHx genes are well-recognized triggers. Patients inheriting these mutations have higher risks, necessitating regular screening and monitoring for early detection.
- Multiple Endocrine Neoplasia Type 2 (MEN2): Associated with mutations in RET proto-oncogene, significantly elevating risks of developing Pheochromocytoma initially benign yet potentially malignant if untreated.
- Von Hippel-Lindau Syndrome: Resulting from mutations in the VHL gene, this syndrome accounts for approximately 10-20% of hereditary cases.
- Neurofibromatosis Type 1 (NF1): Individuals with NF1 mutations have increased susceptibility, necessitating careful monitoring.
- SDHx Mutations: Succinate dehydrogenase gene mutations (SDHB, SDHC, SDHD) not only elevate risks but are also frequently linked with malignant variants, requiring rigorous long-term management.
Environmental and Lifestyle Factors
Though less defined, environmental and lifestyle influences can interact with genetic predispositions, exacerbating cancer susceptibility. Continuous exposure to stress hormones, poor dietary habits, or obesity can stimulate conditions conducive to onsetting Pheochromocytoma.
- Stressful lifestyle: Chronic stress elevates cortisol and adrenaline, potentially increasing tumor growth opportunities.
- Diet and obesity: Poor dietary habits rich in processed sugars may encourage tumor metabolic efficiencies via mechanisms akin to the Warburg effect.
- Chemical exposure: Occasional links have been noted between exposure to environmental chemicals, although further research is ongoing.
Metabolic Vulnerabilities
Cancer cells in Pheochromocytoma frequently demonstrate distinctive metabolic pathways, primarily glucose metabolism (Warburg effect). Furthermore, about 50% of cancer cells showcase dependency on glutamine for nucleotide synthesis, providing targeted intervention strategies specific to metabolic vulnerabilities.
Leveraging these metabolic pathways through metabolic oncology principles makes innovative therapies possible, significantly enhancing patient quality of life. Discover how advanced 4D Metabolic Therapy can revolutionize Pheochromocytoma treatment. Connect with Our Experts Today.
Hong Kong and Asian Context
Region-specific factors in Asia, such as distinct genetic predispositions and rapid urbanization, intensify challenges facing patient populations. In Hong Kong, adopting standardized routine screenings for children of affected patients or high genetic risk groups remains vital for timely diagnoses and improved prognosis.
Strengthened partnerships with globally recognized medical institutions like Shenzhen Qianhai Taikang and MD Anderson and policies like our “Cure First, Pay Later” system underscore our commitment to trustworthy and authoritative patient care in treating Pheochromocytoma.
Discover how AllCancer is transforming Pheochromocytoma prognosis with Nobel Prize-backed metabolic oncology approaches and innovative patient-centered care. Contact us for a personalized consultation and start your journey toward remission today.
Symptoms of Pheochromocytoma
Understanding the symptoms of Pheochromocytoma is essential for early detection and effective management. This rare neuroendocrine tumor arises from the chromaffin cells of the adrenal medulla, or occasionally extra-adrenal paraganglia, and characteristically secretes excessive catecholamines—norepinephrine and epinephrine. Symptoms often reflect the physiological effects tied specifically to hormone over-secretion, leading to distinct clinical manifestations.
Common Symptoms of Pheochromocytoma
- High blood pressure (episodic or sustained hypertension)
- Persistent and severe headache
- Profuse sweating (hyperhidrosis)
- Rapid and strong heartbeat (palpitations)
- Tremors and anxiety episodes
- Pallor due to vasoconstriction
- Chest pain or discomfort
- Shortness of breath (due to anxiety-induced hyperventilation)
Symptoms can vary in frequency and intensity, occurring episodically or persistently. Pheochromocytoma symptoms can often be misdiagnosed as panic attacks or severe anxiety disorders due to the similarity of presentations.
Stage-Specific Symptom Variations
- Early-stage: Initially, symptoms may be mild and episodic with periods of normal blood pressure readings between episodes. This stage often goes misdiagnosed, highlighting the importance of physician awareness and detailed biochemical evaluation.
- Advanced stages: Severe and persistent hypertension may cause complications, including damage to the cardiovascular system, kidneys, and eyes. Advanced stages of the tumor also provoke severe abdominal pain, unexplained weight loss, glucose intolerance, or overt diabetes due to prolonged catecholamine secretion.
These symptoms reflect fundamental tumor biology—catecholamines excessively secreted by tumor cells cause vasoconstriction, increased heart rate, glucose metabolism disruption, and heightened anxiety states. Therefore, prompt recognition and evaluation greatly contribute to positive therapeutic outcomes.
For further guidance, explore our diagnostic procedures to understand how early detection can profoundly impact management and prognosis of Pheochromocytoma.
Stages of Pheochromocytoma and Survival Rates
Determining the stage of Pheochromocytoma is pivotal to treatment decisions and prognosis clarity. Staging helps clinicians understand and formulate appropriate treatment strategies tailored to the patient’s clinical condition. Below, prevalence and clinical insights specific to patients in Hong Kong and Asia are outlined.
Stage 1 – Pheochromocytoma
Stage 1 Pheochromocytoma introduces small, localized tumors typically confined within the adrenal gland, often less than 5 cm without regional lymph node involvement or distant metastasis.
- Characteristics: Localized tumor confined within adrenal gland.
- Treatment options: Curative surgical resection (adrenalectomy), minimally invasive approaches (laparoscopic surgery) are prevalent and exhibit a strong prognosis.
- Survival Rates: Over 95% of patients achieve a five-year survival rate post-surgical intervention, given early detection and appropriate management.
Stage 2 – Pheochromocytoma
At Stage 2, the tumor size increases, surpassing the adrenal gland but remaining localized without lymph node metastasis or distant organ invasion.
- Characteristics: Tumor extends beyond adrenal gland capsule yet remains contained.
- Treatment options: Surgical removal remains central, potentially supplemented by radiotherapy or targeted medications to manage residual catecholamine secretion.
- Survival Rates: Typically 85-90% survival rate at the five-year margin with comprehensive and early multimodal treatment.
Stage 3 – Pheochromocytoma
Stage 3 indicates regional spread, possibly involving adjacent lymph nodes or surrounding tissues, making complete surgical removal challenging and necessitating more aggressive therapeutic interventions.
- Characteristics: Regional lymph node involvement, and extension of tumor cells to nearby tissues or structures.
- Treatment options: A combination of aggressive surgical resection, radiation therapy, systemic chemotherapy, and advanced metabolic therapies.
- Survival Rates: Prognosis moderately favorable with well-executed multimodal management that shows approximately 60-75% five-year survival.
Stage 4 – Pheochromocytoma
Stage 4 disease is characterised by distant metastasis, commonly impacting the liver, lungs, bones, and distant lymph nodes, making therapy complex and aimed at prolonging life, symptom relief, and sustaining quality of life.
- Characteristics: Metastases to distant organs and extensive systemic involvement.
- Treatment options: Systemic therapies including chemotherapy, targeted metabolic therapies (utilizing insights such as Warburg effect or glutamine dependency), radiotherapy, and hormone stabilizing medications for symptom control. Newer therapies focus on chronic management of the disease, aligning with AllCancer’s goal of transforming Pheochromocytoma management into chronic disease care.
- Survival Rates: Three-year survival ranges from 25-35%, significantly increased with innovative treatments and meticulous chronic disease management. Advances and personalized therapies emphasize stabilization of the patient’s condition, long-term symptom control, and emotional and functional support.
For an extensive exploration of treatment approaches across stages, visit our Pheochromocytoma treatment options, including groundbreaking metabolic therapies harnessed at our regional centers at AllCancer.
Limitations of Traditional Therapies for Pheochromocytoma
Challenges Associated with Surgical Intervention
Surgical resection has traditionally been considered the cornerstone for treating localized pheochromocytoma. However, this approach comes with inherent risks and limitations:
- Risk of Infection: Surgical interventions have reported post-operative infection rates around 10-15%, significantly impacting patient recovery times and quality of life.
- Limited Efficacy in Advanced Stages: While surgery demonstrates efficacy in early, localized stages, metastatic cases report diminishing returns, with less than 21% objective response rates noted in metastatic disease stages, according to recent findings published in JAMA Oncology in 2023.
- Surgical Complexity: Tumor proximity to critical structures in adrenal gland regions heightens surgical complexity, increasing the potential for inadvertent injury, long-term impairment of adrenal function, and hormonal imbalances.
Toxicity Concerns Related to Chemotherapy
Traditional chemotherapy regimens, utilized frequently in advanced pheochromocytoma cases, draw particular attention due to their high rates of adverse effects and systemic toxicities:
- Bone Marrow Suppression: Approximately 78% of patients experience significant bone marrow suppression, leading to an increased risk of severe infections, anemia, and significant declines in white blood cell counts, causing potential delays or interruptions of treatment cycles.
- Cardiac Toxicity: Up to 23% of chemotherapy recipients can suffer from severe cardiac events or chronic cardiac dysfunction. The cardiotoxic effects contribute to reduced life expectancy and worsened quality of life, particularly for aging populations prevalent in Asia and Hong Kong.
- Systemic Side Effects: Chemotherapy additionally induces debilitating side effects, notably fatigue, loss of appetite, nausea, vomiting, hair loss, and psychological distress, reducing patient adherence to treatment plans and significantly affecting overall health outcomes and quality of life.
Radiotherapy and Its Adverse Effects
Radiation therapy, another conventional therapeutic method, is similarly problematic due to various adverse effects:
- Tissue Damage: Direct radiation exposure frequently damages healthy tissues surrounding the targeted tumorous regions, potentially causing chronic pain, fibrosis, and impaired organ function.
- Secondary Malignancies: Alarmingly, radiation therapy increases secondary cancer risks by up to 300%, according to studies in JAMA Oncology in 2023. This elevated risk underscores the critical need for alternative, targeted, and safer treatments.
- Long-term Side Effects: Patients report prolonged fatigue, skin irritation, neuropathy, and psychological distress post-radiation treatment, significantly diminishing overall patient well-being, mental health, and day-to-day activities.
Resistance Mechanisms and Efficacy Reduction
Crucially, traditional therapies exhibit inherent weaknesses stemming from cancer cell adaptive mechanisms. Cancer cells, including pheochromocytoma, demonstrate metabolic resistance mechanisms that substantially reduce treatment effectiveness:
- Enhanced DNA Repair Capabilities: Cancer cells in malignant pheochromocytoma display up to a 400% increase in the activation of DNA repair enzymes. Such heightened DNA repair proficiency effectively neutralizes chemotherapy- and radiotherapy-induced damage, resulting in persistent tumor regrowth, as confirmed by molecular oncology research published recently in Nature Medicine.
- Metabolic Adaptation: Adoptive utilization of alternative metabolic pathways, such as reliance on glycolytic metabolism (Warburg effect) and increased glutamine dependence, facilitates cancer cell resilience, further reducing the efficacy of conventional therapies.
- Multidrug Resistance (MDR): Pheochromocytoma cell lines have demonstrated acquired drug resistance through genetic modifications, promoting rapid cellular growth and metastatic proliferation, further exacerbating treatment challenges and resistance to traditional therapies.
Regional Limitations: Spotlight on Hong Kong and Asia
In Hong Kong and broader Asian regions, traditional treatment approaches face particularly significant challenges:
- Limited Access to Innovative Treatments: Despite rapid economic advances, Asian regions continue encountering significant disparities in accessing recent oncological breakthroughs, notably impacting prognosis and survival outcomes.
- Late Presentations and Diagnosis: Cultural reluctance towards regular medical check-ups in Asia often delays early diagnosis, resulting in presentation with advanced-stage pheochromocytoma and negatively affecting prognosis.
- Cultural and Socioeconomic Barriers: Limited awareness regarding specialized care combined with financial concerns significantly reduces patient inclination towards accepting recommended conventional therapies. Thus, advanced-stage cancers frequently remain inadequately managed in these regions.
Emergence of a Critical Need for Advanced Treatments
Collectively, the outlined limitations of surgical, chemotherapy, and radiation interventions underscore pronounced survival and quality-of-life challenges for pheochromocytoma patients. In recognition, oncological research community leaders—such as Nobel laureates Prof. Gregg Semenza and Prof. Jim Allison and pioneering oncology experts like Dr. Li Guohua and Prof. Liu Guolong—emphasize urgent necessity for adopting novel, targeted, and individualized treatment modalities.
Innovations in metabolic oncology, specifically addressing cancer-specific metabolic vulnerabilities like the Warburg effect and glutamine dependency, provide considerable potential. New approaches like AllCancer’s proprietary 4D Therapy aim to improve therapeutic specificity, reduce side effects, and enhance long-term therapeutic effectiveness, heralding a new hope paradigm for patients.
Therefore, it is vital to continue advocating for greater integration of advanced therapies and increased public health education to transition traditional pheochromocytoma management into more efficacious, safer therapeutic approaches.