What Causes Cancer: A 2025 Evidence-Based Guide
Overview
Cancer begins when the tightly regulated instructions inside our cells are rewritten by mutations. These changes can switch on pathways for rapid growth, disable the “stop” signals that keep cell numbers in balance, or cripple the DNA-repair machinery that normally fixes typos in our genetic code[1]. While some mutations are inherited, the overwhelming majority arise after birth and are driven by modifiable lifestyle factors, infections, and environmental exposures.
Primary User Intent & How This Guide Fulfills It
Most people who type “what causes cancer” into Google are looking for a trustworthy, plain-language explanation of why the disease starts, plus actionable steps to reduce risk. This article directly answers that need by:
- Explaining the biology of mutations and tumor formation.
- Listing evidence-based causes in everyday terms.
- Providing 2025 prevention recommendations.
- Linking to authoritative health portals for deeper reading.
1. Gene Mutations—The Root Cause
Key takeaway: Mutations are necessary but not sufficient; additional “hits” are needed for full-blown cancer.
- Oncogenes – mutations here act like a stuck accelerator pedal, telling cells to divide non-stop.
- Tumor-suppressor genes – when these brakes fail, cells ignore stop signals.
- DNA repair genes – when spell-checkers are disabled, further mutations accumulate rapidly[1].
2. Inherited vs. Acquired Mutations
| Type | Share of All Cancers | Examples | Implication |
|---|---|---|---|
| Inherited (germline) | ≈5–10 % | BRCA1/2, Lynch syndrome | Earlier screening needed |
| Acquired (somatic) | ≈90–95 % | TP53 from smoking, UV-induced BRAF | Often preventable |
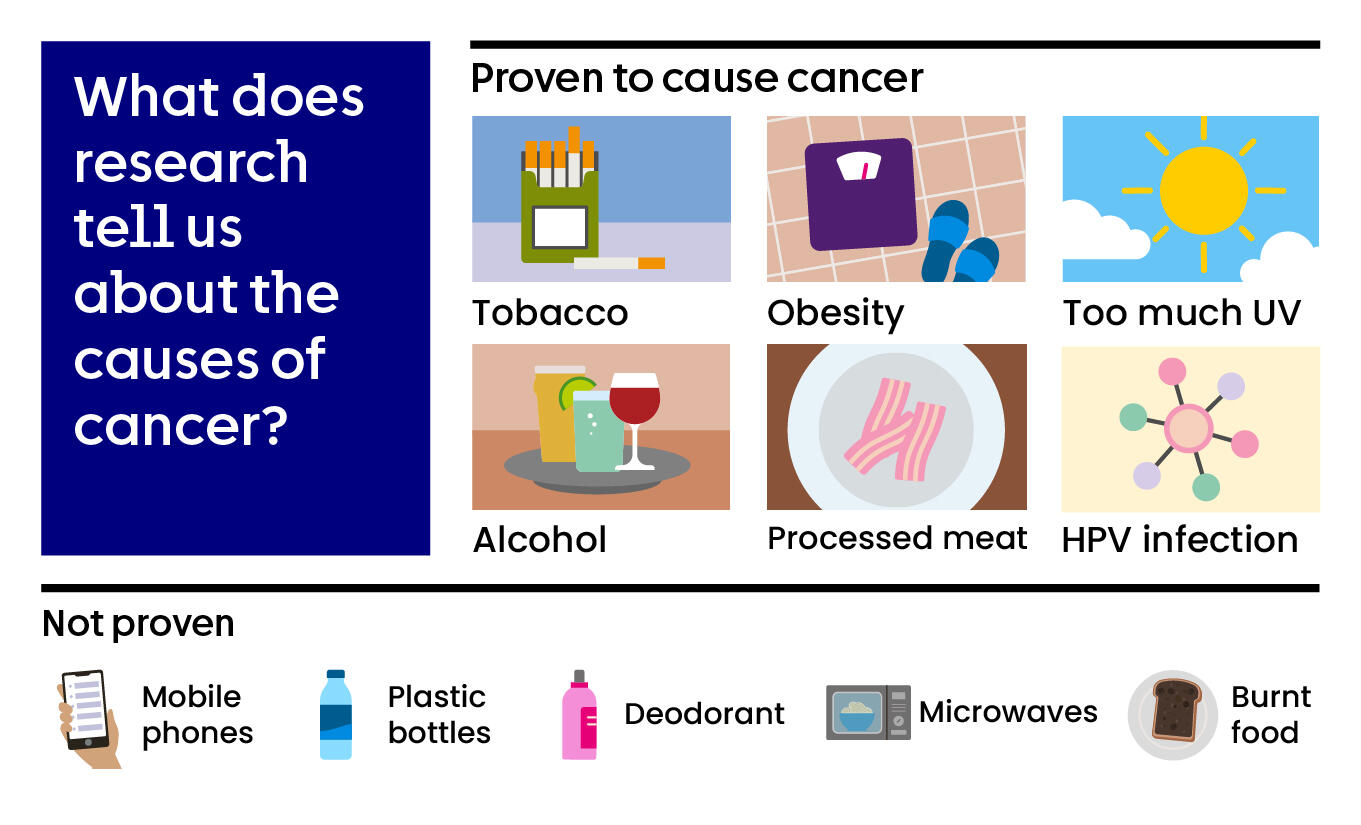
3. Lifestyle & Environmental Causes (2025 Update)
3.1 Tobacco and Alcohol
Smoking remains the single largest preventable cause, responsible for ≈22 % of global cancer deaths in 2024 projections. Alcohol adds a synergistic risk, especially for head-and-neck and esophageal cancers.
3.2 Diet, Obesity & Physical Inactivity
- Processed meat is classified as Group 1 carcinogen.
- Obesity increases endometrial cancer risk 5-fold and post-menopausal breast cancer risk 1.5-fold.
- Regular moderate exercise can cut colon-cancer risk by 24 %.
3.3 Infectious Agents
| Pathogen | Cancers | Prevention |
|---|---|---|
| HPV | Cervical, oropharyngeal | Vaccination & screening |
| Hepatitis B/C | Liver cancer | Vaccination, antivirals |
| Helicobacter pylori | Stomach cancer | Test & treat |
3.4 Environmental & Occupational Exposures
Historical studies—from Yamagiwa’s 1915 coal-tar experiments in rabbits[2] to modern cohorts—confirm that:
- Asbestos → mesothelioma, lung cancer.
- UV radiation → melanoma.
- Aflatoxin-contaminated food (common in hot, humid climates) interacts with hepatitis B to multiply liver-cancer risk 59-fold[2].
4. Emerging & Less-Known Causes
- Chronic inflammation – e.g., reflux esophagitis → Barrett’s → esophageal adenocarcinoma.
- Microbiome dysbiosis – altered gut flora may promote colorectal neoplasia (2025 meta-analysis).
- Air pollution (PM2.5) – now linked to increased lung and bladder cancer incidence.
5. Can We Prevent Most Cancers?
Yes—around 40–50 % of cancers are preventable. The World Cancer Research Fund’s 2025 blueprint centers on “Life’s Simple 7”:
- Don’t smoke or vape.
- Limit alcohol to ≤1 drink/day (women) or ≤2 drinks/day (men).
- Maintain a healthy body weight (BMI 20–25).
- Eat a plant-forward diet (≥400 g fruits & vegetables daily).
- Be physically active (≥150 min moderate or 75 min vigorous per week).
- Protect skin from UV exposure.
- Stay up to date on vaccinations and cancer screenings.
6. What to Do if You’re at High Risk
- Genetic counseling if you have a strong family history.
- Enhanced screening protocols (e.g., annual breast MRI for BRCA carriers).
- Chemoprevention (aspirin for Lynch syndrome; tamoxifen for high-risk breast tissue).
7. Key Takeaways
- Cancer is a multi-step process driven by DNA damage and clonal evolution.
- Only a small fraction is inevitable; most cases trace back to identifiable—and avoidable—causes.
- Every individual can lower risk through evidence-based lifestyle choices and timely medical interventions.
References
- Mayo Clinic – Cancer – Symptoms and causes – https://www.mayoclinic.org/diseases-conditions/cancer/symptoms-causes/syc-20370588
- NIH PMC – Historical review of the causes of cancer – https://pmc.ncbi.nlm.nih.gov/articles/PMC4734938/