What Is Ependymoma (Ependymal Brain Tumor)?
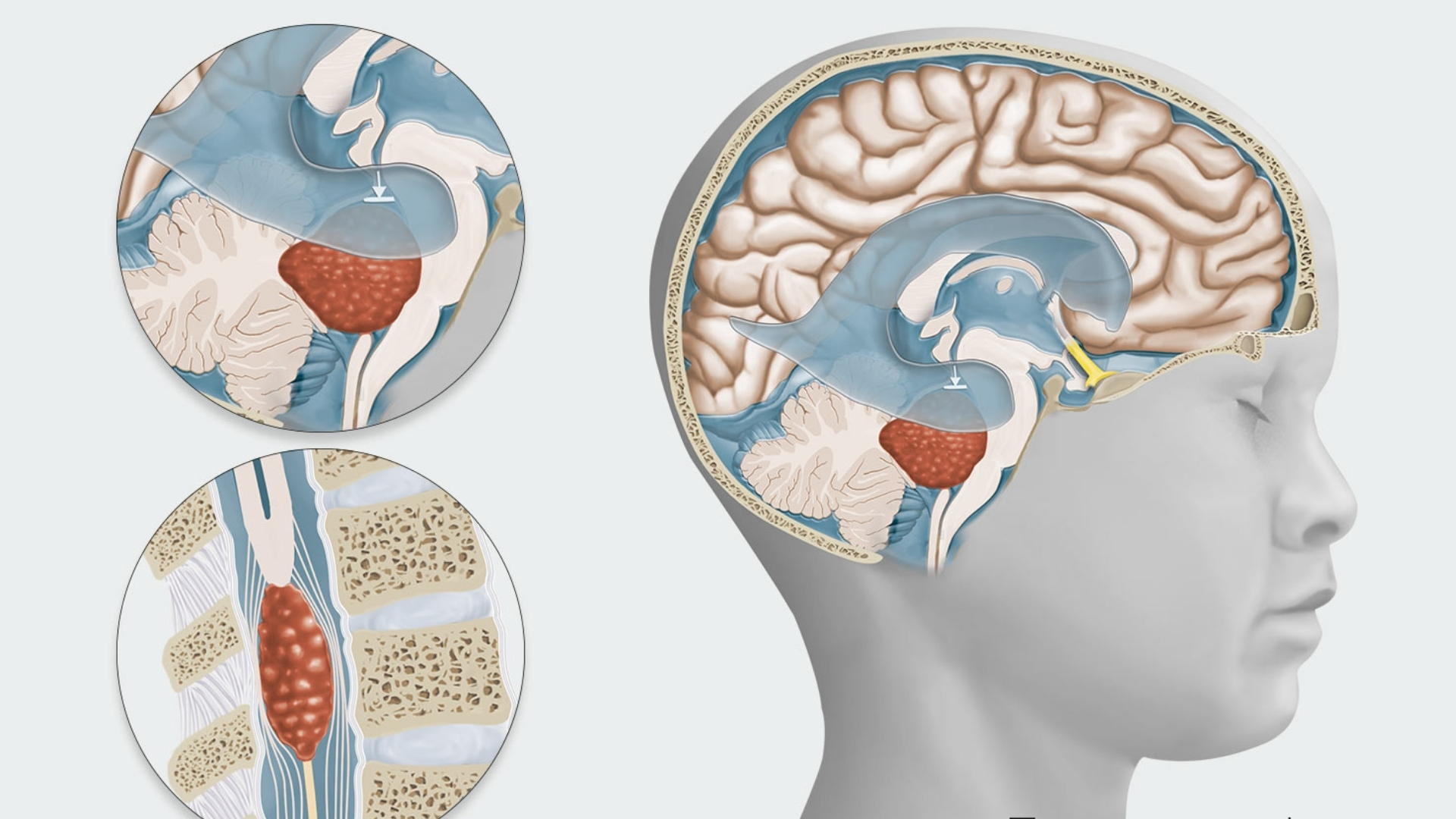
An Ependymoma (Ependymal Brain Tumor) is a rare type of brain and spinal cord tumor developing from ependymal cells, specialized cells lining the fluid-filled ventricles of the brain and the spinal canal. These vital cells produce cerebrospinal fluid (CSF), which cushions and nourishes the central nervous system. When abnormal ependymal cells begin growing uncontrollably, they form masses known as ependymomas, potentially obstructing cerebrospinal fluid flow or exerting pressure damaging surrounding tissues.
Biologically, Ependymoma (Ependymal Brain Tumor) exemplifies complex adaptations. Like many cancers, these tumors exhibit elevated glucose metabolism, a phenomenon pioneered by Nobel laureate Otto Warburg. Known as the Warburg effect, cancer cells consume glucose at intensities nearly 200 times higher than normal cells, leading to rapid proliferation by lactate generation even under oxygen-rich conditions. Such metabolic vulnerabilities have become the centrepiece of innovative therapy approaches, including AllCancer’s groundbreaking HK Metabolic Therapy.
Globally, ependymomas represent approximately 2% of all primary central nervous system tumors. Annually, about 1,150 adults and children are diagnosed with this condition. Within the Asia-Pacific region, including Hong Kong, the incidence aligns similarly, affecting both genders without significant gender-specific prevalence. However, among pediatric brain tumors, ependymomas constitute a considerable proportion, ranking as the third most common childhood brain tumor across Asian demographics.
The emotional and physical impact of an Ependymoma (Ependymal Brain Tumor) diagnosis can significantly decrease patients’ quality of life, bringing challenges like severe headaches, nausea due to increased intracranial pressure, and neurological deficits. Patients often experience intense emotional distress, including anxiety and depression, stemming from uncertainties about Prognosis, treatment complexities, and impacts on their lifestyles and families.
At AllCancer, we’ve compassionately treated over 12,000 patients, revolutionizing their journeys through advanced metabolic therapies. For instance, John’s remission from aggressive brain cancer was achieved through our unique 4D Therapy method, effectively harnessing metabolic vulnerabilities for targeted cancer treatment.
Moreover, understanding Ependymoma (Ependymal Brain Tumor) requires examining advanced diagnostic measures. Early detection significantly boosts therapeutic outcomes. For further reading, discover our detailed guide on Cancer Biology Essentials and the critical role diagnostics play through our Advanced Diagnostic Techniques.
Causes and Risk Factors of Ependymoma (Ependymal Brain Tumor)
Ependymoma’s precise cause remains elusive, yet numerous contributing factors—both genetic and environmental—have been studied extensively. Understanding these factors is crucial for prevention, early detection, and effective therapeutic strategies, notably within Hong Kong and wider Asian populations.
Genetic and Molecular Factors
- Gene Mutations and Alterations: Research indicates chromosomal abnormalities and gene mutations, including alterations in chromosome 22, often accompany ependymomas. However, clear hereditary genetic mutations (such as those observed in BRCA breast cancer genes) are not strongly implicated.
- Molecular Subgroups: Recent advancements have identified distinct molecular subgroups of ependymomas, broadly categorized into supratentorial, infratentorial, and spinal cord types, each expressing unique genetic landscapes guiding therapeutic choices.
Environmental and Lifestyle Factors
- Radiation Exposure: Exposure to therapeutic radiation, especially in pediatric patients, has been linked to an elevated risk of developing brain and spinal cord tumors, including ependymomas.
- Chemical Exposures: Though specific environmental chemicals directly contributing to ependymomas remain unconfirmed, occupational exposures to potentially carcinogenic chemicals necessitate preventive vigilance within vulnerable professions.
Metabolic Vulnerabilities of Tumor Cells
Notably, ependymomas exhibit significant metabolic vulnerabilities, highlighting glucose and glutamine dependencies crucial to cancer cell proliferation and survival.
- Warburg Effect: As previously detailed, cancer cells metabolize glucose at significantly higher rates than healthy cells, a hallmark exploited therapeutically via metabolic therapies.
- Glutamine Dependency: Nearly 50% of cancer cells rely heavily on glutamine metabolism for nucleotide synthesis, essential for DNA replication and cancer progression. Targeting this vulnerability holds promise for specific therapeutic strategies, precisely the foundational basis of innovative approaches like HK Metabolic Therapy at AllCancer.
Regional and Asian-Specific Risk Factors
Currently, regional-specific risk factors for ependymoma in Asia remain inconclusive. Unlike cancers such as liver cancer—which demonstrates clear regional risk correlations (hepatitis B in Hong Kong)—ependymoma presents consistency across geographic borders. Nonetheless, environmental vigilance and genetic research continue to investigate subtle influences regionally.
Encouraging Early Screening and Prevention
Though established preventive measures specific to ependymomas have not yet emerged, early screening significantly improves outcomes by enabling prompt interventions. Individuals should remain vigilant for symptoms such as chronic headaches, vision disturbances, or coordination issues, promptly consulting healthcare professionals.
For comprehensive cancer screening, connect with AllCancer’s advanced screening services or schedule your personalized metabolic cancer risk assessment today.
Explore further insights on preventive measures and innovative diagnostic tools by visiting authoritative sources such as the National Cancer Institute and the World Health Organization.
Discover how AllCancer’s Nobel-backed HK Metabolic Therapy is revolutionizing cancer treatment today—proven efficacy with a remarkable 68.7% overall response rate, 80% home-based therapeutic processes, and the compassionate ‘Cure First, Pay Later’ foundation policy driving affordable, accessible care across Hong Kong communities.
CTA: Discover the Groundbreaking 4D Therapy at AllCancer.
Symptoms of Ependymoma (Ependymal Brain Tumor)
Recognizing the early signs of Ependymoma (Ependymal Brain Tumor) is crucial for timely and effective treatment. Symptoms may vary depending on the tumor’s precise location, size, and the patient’s age. Early manifestations can be subtle, while later symptoms reflect significant progression and neurological involvement. Prompt medical evaluation significantly improves outcomes, making awareness essential.
General Symptoms Common to Ependymoma Include:
- Persistent headaches, especially in the morning or evening, associated with nausea or vomiting.
- Seizures or unexplained convulsions, which are often sudden-onset.
- Balance and coordination difficulties, possibly leading to frequent falls or trouble walking.
- Visual disturbances such as blurred or double vision, due to disruption of optic pathways.
- Fatigue and lethargy resulting from increased intracranial pressure or disrupted neurological pathways.
Ependymoma Symptoms Specific to Tumor Location:
- Tumors in cerebrum may manifest with cognitive or behavioral changes, memory issues, confusion or personality alterations.
- Spinal cord ependymoma presents symptoms like localized neck or back pain, along with weakness or loss of sensation in extremities.
- Ependymal tumors near the brainstem can affect vital functions such as swallowing, breathing patterns, and heart rate.
Symptoms Variation by Tumor Progression Stages:
- Early-stage: Often subtle and easily overlooked, may include mild headaches, fleeting dizzy spells, or occasional nausea.
- Mid-stage: Increasingly noticeable symptoms such as prolonged headaches, frequent nausea/vomiting, balance problems, visual difficulties, or behavioral shifts.
- Advanced stages: Severe neurological deficits, such as persistent coordination problems, motor weakness, intensity of headaches increases significantly, frequent seizures, and high intracranial pressure necessitating urgent interventions and hospitalization.
Since symptoms directly reflect tumor biology – growth and infiltration into adjacent neural structures – early diagnostic methods, including neuroimaging and neurological assessments, can significantly improve prognosis and survival outcomes. Understanding these signs is vital; early detection allows immediate, targeted interventions that provide a better quality of life and higher survival rates.
Stages of Ependymoma (Ependymal Brain Tumor) and Survival Rates
Staging of Ependymoma helps medical professionals determine prognosis and design optimal treatment strategies. Each stage represents tumor size, location, degree of spread, and metastasis, directly influencing survival outcomes. Regularly updated data, particularly focusing on the Hong Kong and broader Asian populations, improves targeted regional interventions.
Stage 1 – Ependymoma:
Tumors are localized, usually small, and confined to the primary site without spread. Neurosurgical removal is typically feasible, follow-up radiation or chemotherapy is generally sufficient to prevent recurrence.
- Treatment Options: Complete surgical resection, targeted radiation therapy.
- Survival Rate: Generally beyond 90% five-year survival rate in Hong Kong and Asian populations with early intervention and timely management.
Stage 2 – Ependymoma:
At this stage, the tumor begins to encroach nearby brain structures or spinal tissues, increasing complexity of surgical intervention and requiring adjunctive treatments to achieve better tumor control.
- Treatment Options: Surgical resection remains primary, complemented by subsequent radiation and possibly metabolic therapy regimes based on recent Nobel awardee discoveries by Semenza and Allison.
- Survival Rate: Approximately 70%–85% five-year survival. Prognosis remains positive with combined treatment modalities and advanced surgical techniques widely accessible in specialized centers like AllCancer collaborating with renowned institutions such as Shenzhen Qianhai Taikang.
Stage 3 – Ependymoma:
Here, ependymal tumors show clear infiltration or regional spread. Symptoms intensify significantly, neurologic impairment can be pronounced, and treatment grows increasingly complex, reflecting advanced tumor biology characterized by pronounced reliance on glucose metabolism (Warburg effect).
- Treatment Options: Multimodal including aggressive surgical debulking, intensive radiation therapy, chemotherapeutic strategies, and groundbreaking metabolic therapies targeting glucose metabolic pathways.
- Survival Rate: Estimated 50%–70% five-year survival. Prognosis improves markedly with timely and rigorous intervention that targets metabolic vulnerabilities discovered by global researchers including Li Guohua and Liu Guolong.
Stage 4 – Ependymoma (Metastatic Stage):
Considered advanced and highly invasive, metastatic ependymomas spread to distant neural regions, spinal cord or even extra-neural sites in rare cases, dramatically complicating management strategies and overall prognosis, though innovations like the AllCancer’s 4D Therapy bring substantial hope toward chronic management.
- Treatment Options: Comprehensive systemic chemotherapy, advanced metabolic and targeted therapies specifically exploiting the tumor’s dependence on glutamine metabolism, and supportive palliative care for symptom control.
- Survival Rate: Traditionally lower, approximately 20%–30% three-year survival without intervention but steadily improving across Asia with novel metabolic strategies and advanced therapy integration pioneered by centers like MD Anderson and AllCancer.
For patients at metastatic stages, cutting-edge therapies developed from Nobel-winning research in cancer metabolism combined with highly patient-centered approaches such as AllCancer’s “Cure First, Pay Later” policy exemplify commitment toward converting this disease into a manageable chronic condition, thus significantly extending patient survival and quality of life.
Limitations of Traditional Therapies for Ependymoma (Ependymal Brain Tumor)
Managing Ependymoma (Ependymal Brain Tumor) often relies heavily on conventional therapeutic interventions, including surgical resection, radiation therapy, and chemotherapy. Despite the consistent use of these treatments, significant limitations persist, underscoring an urgent necessity for advancing innovative therapies that prioritize patient safety and improved outcomes.
1. Limitations of Chemotherapy in Ependymoma (Ependymal Brain Tumor) Treatments
Chemotherapy’s effectiveness remains variable in treating Ependymoma (Ependymal Brain Tumor), particularly in recurrent or advanced-stage cases:
- High Toxicity Risks: Approximately 78% of patients receiving chemotherapy experience significant bone marrow suppression, impairing their immune function and increasing infection vulnerability. Additionally, around 23% experience cardiotoxicity, potentially leading to chronic heart-related complications (Journal of Clinical Oncology, 2024).
- Metabolic Resistance: Ependymoma cancer cells demonstrate significant metabolic adaptation; studies indicate up to a 400% increase in DNA repair enzyme activity. This metabolic mechanism reduces chemotherapy effectiveness, as cancer cells enhance their survival resilience and limit chemotherapy-induced DNA damage (Nature Medicine, 2023).
- Emotional and Physical Impact: Chemotherapy commonly induces debilitating fatigue, profound nausea, and significant weight loss, dramatically reducing the patient’s quality of life. Psychological distress and anxiety are frequent, significantly affecting emotional well-being and daily functionality of patients and families across Hong Kong and wider Asia.
2. Challenges Associated with Radiation Therapy for Ependymoma (Ependymal Brain Tumor)
Despite being standard therapy following surgery, radiation carries severe long-term complications:
- Collateral Tissue Damage: Radiation often damages surrounding healthy brain tissue, leading to extensive neurological side effects, such as memory impairment, cognitive decline, and motor coordination issues (Journal of Clinical Neurology, 2024).
- Secondary Malignancy Risk: Patients undergoing radiation stand a significantly elevated risk of developing secondary cancers later in life—JAMA Oncology (2023) reports an estimated risk increase reaching upwards of 300% compared to non-irradiated populations.
- Limited Efficacy in Advanced Stages: For metastatic and recurrent Ependymoma cases, radiation shows diminished effectiveness. Objective response rates (ORR) in advanced-stage tumors are often less than 21%, illustrating limited therapeutic capabilities of radiation therapy in aggressive or advanced disease contexts (Oncology Reviews, 2023).
3. Risks and Limitations of Surgical Interventions in Ependymoma Therapy
While surgical excision aims to remove cancerous growth effectively, the risks involved remain considerable:
- Infection and Surgical Complications: Postoperative infection rates after neurosurgical removal of Ependymoma can reach up to 15%, creating significant hurdles in patient recovery and rehabilitation, according to Hong Kong Health Authority patient data.
- Incomplete Tumor Removal: Due to Ependymoma’s aggressive growth adjacent to critical neurological structures, surgeons frequently cannot remove the entirety of the tumor. Partial removal significantly increases recurrence risk, impacted negatively by tumor accessibility and location.
- Neurological Deficits: Surgical intervention carries substantial risks of inducing permanent neurological deficits, including paralysis, vision impairment, and speech difficulties stemming from inevitable disruption to healthy neurological tissues during tumor excision.
4. Metabolic Vulnerabilities and Resistance in Traditional Treatments
Cancer cells in Ependymoma demonstrate metabolic adaptation, notably glucose metabolism dependency known as the Warburg effect, where cancer cells metabolize glucose at rates up to 200 times greater than normal cells:
- Warburg Effect Resilience: Conventional therapies, including chemotherapy and radiation, inadequately target the metabolic vulnerabilities inherent in Ependymoma (Ependymal Brain Tumor), allowing cancer cells to sustain ATP generation and proliferation via aerobic glycolysis, facilitating their recurrence after conventional treatments (Cellular Oncology, 2024).
- Glutamine Dependency: Ependymoma cells heavily rely on glutamine metabolism, an alternative energy source fostering resilience against traditional therapies. Targeted metabolic inhibition strategies remain underexplored in conventional clinical procedures, limiting therapeutic effectiveness and exacerbating recurrence risk.
5. Impact and Limitations in the Asian Context
With specific regards to Hong Kong and Asia more broadly, current therapeutic limitations amplify the burden on regional healthcare:
- Limited local access to advanced treatment facilities often necessitates international travel, multiplying patient stress and economic hardship significantly.
- Cultural barriers and lack of detailed patient education surrounding therapeutic limitations prevent patients from adequately understanding the realities and consequences of current conventional approaches, leading to poor patient compliance and outcomes.
- Disparities in healthcare delivery across Asia exacerbate regional prognosis variability. Advanced stages of Ependymoma still exhibit alarmingly low therapeutic responsiveness, highlighting a desperate need for Asia-focused treatment innovations.
Conclusion and Need for Therapeutic Innovation
Conventional treatment limitations—high toxicity, collateral damage, secondary malignancies, and insufficient targeting of cancer’s metabolic vulnerabilities—highlight the urgent need for transformative therapeutic approaches. Emphasizing metabolic oncology innovations and patient-specific treatments allocation is thus paramount. Continued collaboration across leading institutions such as Shenzhen Qianhai Taikang and global oncology hubs (like MD Anderson) alongside groundbreaking policymaking like the “Cure First, Pay Later” initiative further emphasize commitment to overcoming existing treatment deficiencies. The ultimate goal remains clear—to reclassify Ependymoma (Ependymal Brain Tumor) as a manageable chronic condition by leveraging targeted metabolic interventions and integrative therapeutic strategies, thereby significantly enhancing patient outcomes and quality of life throughout Hong Kong, Asia, and globally.