What Is Esophageal Cancer (Esophageal Carcinoma)?
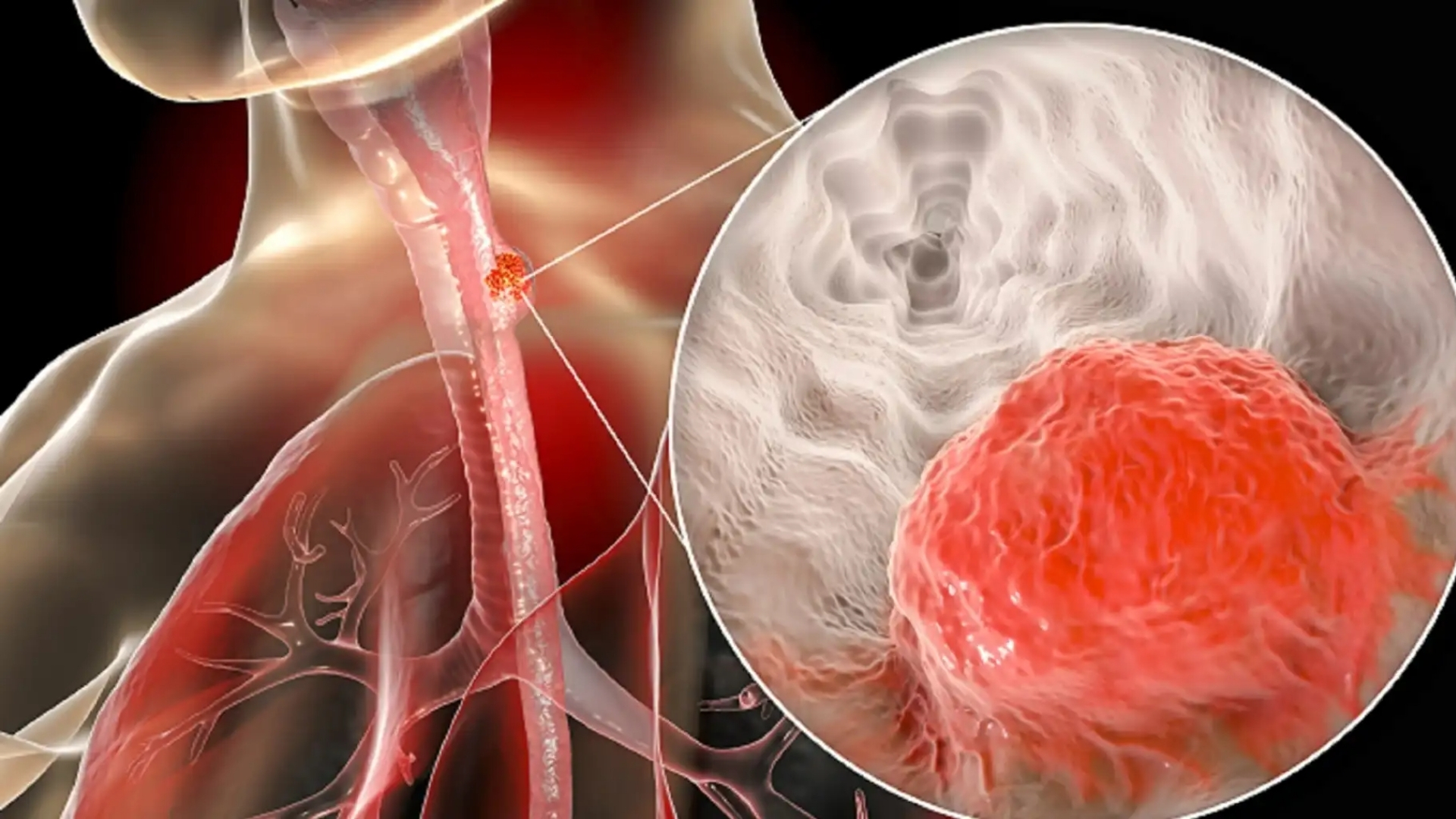
Understanding Esophageal Cancer (Esophageal Carcinoma) starts with exploring the esophagus—a muscular tube connecting your throat to the stomach which facilitates the passage of swallowed food. Esophageal carcinoma occurs when malignant cells develop in the lining of this structure, altering normal tissue function.
Esophageal carcinoma manifests primarily in two main forms: Squamous Cell Carcinoma, usually affecting the upper and middle esophagus, and Adenocarcinoma, generally impacting the lower esophagus near the gastroesophageal junction. Globally, this condition ranks eighth among prevalent cancers, with over 600,000 new cases annually (WHO, 2024).
In Hong Kong and broader Asia, esophageal carcinoma presents specific public health challenges due to distinct lifestyle habits. Furthermore, studies by cancer biology pioneers such as Nobel laureate Prof. Gregg Semenza have highlighted the metabolic vulnerability of esophageal carcinoma, notably the “Warburg effect,” wherein cancer cells aggressively consume glucose at nearly 200 times the normal cellular rate.
Recognizing symptoms early significantly impacts survival outcomes. Commonly reported symptoms include:
- Difficulty swallowing foods or liquids, indicating tumor-induced narrowing of the esophagus (dysphagia)
- Persistent chest pain or discomfort, particularly when swallowing
- Unintentional weight loss due to reduced nutritional intake and heightened metabolic demands
- Hoarseness, coughing, or throat pain not associated with infection
- Indigestion and heartburn resistant to conventional treatment
- Fatigue and weakness, especially pronounced during advanced stages
Emotionally, these symptoms can compound, leading to psychological distress and reduced quality of life. At AllCancer, with experience drawn from successfully managing over 12,000 cases globally, we strive to blend science and compassion, understanding deeply patients’ emotional and physical experiences.
Understanding Esophageal Cancer (Esophageal Carcinoma) also includes awareness of disease prevalence. In Asia, particularly East Asia, the incidence is notably high due to dietary habits, consumption of hot beverages, and alcohol/tobacco use. In Hong Kong, three out of four esophageal carcinoma patients are men, aged predominantly between 50 and 75 years, reflecting lifestyle and environmental risk correlations.
Increased glucose dependency marked by the Warburg phenomenon has guided innovative treatment development like targeted metabolic therapies, extensively published in Nature Medicine. Check more about cancer biology here or our advanced diagnostic methods here.
Causes and Risk Factors of Esophageal Cancer (Esophageal Carcinoma)
Genetic Factors and Familial Risks
Although esophageal carcinoma generally lacks clear hereditary patterns akin to BRCA mutations in breast cancer, genetic predispositions are nonetheless evident. Certain inherited genetic conditions, such as tylosis—a disorder causing abnormal tissue hardening—raise esophageal cancer risk substantially.
Genetic polymorphisms in enzymes affecting alcohol metabolism further intensify risks associated with alcohol consumption, particularly prevalent in Asian populations, including Hong Kong. Ongoing genomic research, led by experts like Dr. Li Guohua and Prof. Liu Guolong, has unveiled markers indicating increased vulnerability, paving avenues for targeted preventive strategies.
Lifestyle and Dietary Factors
Consistent evidence confirms lifestyle-related contributors significantly increase esophageal carcinoma likelihood:
- Tobacco use: Smokers have a markedly higher incidence, associated with carcinogenic chemicals inhaled during smoking.
- Alcohol: Chronic alcohol consumption irritates esophageal tissue, doubling carcinoma risks. The combination with tobacco exponentially increases vulnerability.
- Dietary habits: Regularly consuming very hot beverages or preserved, salted, smoked, and pickled foods common in Asian cultures—including Hong Kong’s traditional cuisine—elevates exposure to carcinogens and irritation risks.
- Obesity: Excessive body weight increases acid reflux and inflammation, contributing to the adenocarcinoma variant of esophageal carcinoma.
Metabolic Vulnerabilities (Warburg Effect and Glutamine Dependency)
Recent cancer biology research emphasizes metabolic vulnerabilities inherent in esophageal carcinoma cells. Nobel laureate Dr. Jim Allison highlights metabolic dysregulation such as the Warburg Effect—tumor cells preferentially metabolizing glucose anaerobically, enabling rapid growth and proliferation.
Additionally, approximately 50% of cancerous esophageal tissue demonstrates increased dependency on glutamine. This amino acid supports crucial nucleotide synthesis pathways, fueling rapid cellular replication characteristic of cancer progression. Understanding these metabolic dependencies offers opportunities for targeted therapeutic interventions.
Environmental Factors and Geographic Risks in Asia & Hong Kong
Geographically-specific environmental factors significantly shape local cancer epidemiology. In multiple Asian regions, environmental pollutants, dietary micronutrient deficiencies, and infections (e.g., Helicobacter pylori) contribute synergistically to heightened esophageal carcinoma risks.
Hong Kong’s distinctive mix of Western and traditional Asian lifestyles uniquely affects incidence and prevalence of esophageal carcinoma, marking importance for tailored screening and preventive interventions based on regional data.
Importance of Early Detection and Screening
Early detection dramatically improves survival rates and treatment options. Regular screening is particularly recommended for individuals with elevated genetic, dietary, or lifestyle risks. Modern diagnostic methods, coupled with an integrated metabolic-focused therapy approach pioneered by AllCancer, remain an essential preventive component in Hong Kong and Asia.
CTA:
Discover how 4D Therapy transforms Esophageal Cancer (Esophageal Carcinoma) treatment: Explore Core Therapy Innovations. Limited 2025 slots available!
Symptoms of Esophageal Cancer (Esophageal Carcinoma)
Recognizing the symptoms of Esophageal Cancer (Esophageal Carcinoma) early is critical for improving prognosis and successful treatment outcomes. Symptoms reflect underlying biological changes, notably tumor blockage or invasion causing structural and functional impacts.
Early Signs and Symptoms
- Difficulty swallowing, initially with solid foods but progressing to liquids.
- Sensation of food sticking in the chest or throat region during eating.
- Persistent heartburn, often unresponsive to common antacid medications.
- Unexplained weight loss despite normal diet or minor dietary changes.
- Mild chest pain or discomfort not associated with recognized cardiac symptoms.
- Chronic cough unrelated to common respiratory infections or allergies.
- Sensation of burning or irritation when ingesting hot beverages or spicy foods.
Advanced Signs and Symptoms
- Severe difficulty swallowing, making eating challenging or nearly impossible.
- Substantial weight loss, weakness, muscle wasting (cachexia) due to compromised nutrition.
- Intense chest pain, back pain, or radiating pain indicating deeper tumor invasion or nerve involvement.
- Persistent vomiting or regurgitation, sometimes with blood (hematemesis).
- Hoarseness or chronic voice changes indicating possible vocal cord or nerve involvement.
- Shortness of breath due to aspiration of food or saliva into the lungs.
- Swollen lymph nodes near the collarbone or neck region palpable upon self-examination.
It’s essential to understand how early intervention positively impacts outcomes in esophageal cancer. If you experience persistent signs, please seek medical attention promptly. Explore our dedicated diagnostics page for comprehensive testing details.
Stages of Esophageal Cancer (Esophageal Carcinoma) and Survival Rates
The staging of Esophageal Cancer (Esophageal Carcinoma) is crucial for treatment planning and prognosis determination. Here, we explore each stage in depth, highlighting specific characteristics, recommended treatment approaches, and survival outcomes based on Hong Kong and wider Asian epidemiology.
Stage 1 – Esophageal Cancer (Esophageal Carcinoma)
In Stage 1, the cancer is localized strictly to the superficial layers of the esophageal lining without deeper penetration or lymphatic spread. At this early detection stage, survival outcomes are significantly improved.
- Characteristics: Tumor confined to the superficial mucosa and submucosa layers, usually small-sized lesions impacting limited esophageal segments.
- Treatment Approaches: Primarily involves surgical resection (esophagectomy) for complete tumor removal or minimally invasive endoscopic treatments such as endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD).
- Survival Rate: According to local Hong Kong oncology centers, 5-year survival rates of Stage 1 esophageal carcinoma approach 85–90%.
Stage 2 – Esophageal Cancer (Esophageal Carcinoma)
Stage 2 esophageal cancers have penetrated deeper muscular layers or spread to immediate regional lymph nodes. Accurate staging through imaging and endoscopic ultrasound becomes crucial to treatment planning.
- Characteristics: Moderately sized tumors infiltrating deeper muscular layers or initial involvement of regional lymph nodes.
- Treatment Approaches: Multimodal treatments including surgical resection combined with chemotherapy and radiation therapy (chemoradiotherapy) are standard practice.
- Survival Rate: In Hong Kong and other advanced Asian oncology facilities, estimated Stage 2 survival at five-years ranges from approximately 60–70%.
Stage 3 – Esophageal Cancer (Esophageal Carcinoma)
Stage 3 represents advanced local-regional invasion, with substantial penetration into surrounding structures and extensive lymphatic involvement, indicating aggressive tumor spread.
- Characteristics: Larger tumors significantly invading deeper esophageal layers or nearing adjacent thoracic structures. Substantial regional lymph node involvement.
- Treatment Approaches: Comprehensive multimodality therapy including preoperative chemoradiotherapy (neo-adjuvant), surgery, and postoperative adjuvant chemotherapy/radiation therapy as determined by patient responsiveness.
- Survival Rate: Despite advanced stage, aggressive integrated treatment approaches in leading Hong Kong and Asian medical establishments yield provisional five-year survival rates between 30–50%.
Stage 4 – Esophageal Cancer (Esophageal Carcinoma)
Stage 4 cancer extends beyond its origin, spreading to distant organs such as liver, lungs or bones. This metastatic stage represents the most challenging treatment difficulty.
- Characteristics: Spread to distant organs with symptoms reflective of that systemic involvement (such as hepatic enlargement, respiratory distress).
- Treatment Approaches: Systemic treatments are frontline strategies including chemotherapy, targeted therapy (HER2-targeted treatment in adenocarcinoma), immunotherapy, and palliative radiation for symptom relief.
- Survival Rate: Historically, 5-year survival rates for stage 4 esophageal carcinoma averaged less than 20% across Asia; however, enhanced chronic management opportunities offered by innovative therapies such as immunotherapy, targeted therapy, and metabolic therapy approaches pioneered by Dr. Li Guohua bring improved prognostic potentials.
Though advanced-stage esophageal carcinoma poses significant management complexities, notable treatment advances particularly metabolic approaches leveraging cancer cells’ glucose dependency (Warburg effect) or glutamine utilization offer increasing hope. As part of AllCancer’s ambitious goal by 2025, esophageal carcinoma could potentially be managed more effectively as a chronic illness in selected patients, drastically extending meaningful and quality life.
To better understand comprehensive treatment options at every cancer stage, please visit our dedicated treatment options page and learn more about state-of-the-art innovations transforming esophageal carcinoma management.
Limitations of Traditional Therapies for Esophageal Cancer (Esophageal Carcinoma)
Chemotherapy Toxicity and Its Impact on Patient Quality of Life
Chemotherapy remains a primary treatment for Esophageal Cancer (Esophageal Carcinoma), particularly for advanced stages. However, traditional chemotherapy can significantly compromise patient health through systemic toxicity. The aggressive nature of cytotoxic drugs does not differentiate effectively between tumor cells and normal rapidly dividing cells, leading to severe adverse effects in patients.
- Bone marrow suppression—the significant decline in blood cell production—is reported in approximately 78% of patients undergoing chemotherapy, often resulting in severe anemia, neutropenia, and increased susceptibility to serious infections.
- Cardiac toxicity occurs in nearly 23% of cases, highlighting major risks such as arrhythmias and heart failure, as documented extensively in oncology literature from JAMA Oncology 2023.
- Additional frequent symptoms include nausea, emesis, mucositis, and drastic weight loss, profoundly decreasing patient quality of life and complicating further treatments and recovery.
Conventional therapy efficacy also generally decreases markedly in late-stage disease. For patients diagnosed with metastatic Esophageal Cancer (Esophageal Carcinoma), typical chemotherapy regimens achieve an objective response rate of less than 21%, substantially limiting patient prognosis and survival.
Radiation Therapy and Associated Risks in Esophageal Cancer (Esophageal Carcinoma)
Radiation therapy, another cornerstone treatment, brings its own considerable set of challenges. Although radiation can effectively target localized tumors, its broader impact on surrounding healthy tissues causes long-term adverse consequences, frequently experienced by patients as debilitating side effects.
- Tissue damage and fibrosis subsequent to radiation exposure pose significant functional impairments, including strictures that restrict swallowing and nutritional intake, severely affecting patient wellbeing and treatment adherence.
- Radiation pneumonitis and esophagitis commonly occur post-treatment, often diminishing patient functionality significantly years after concluding radiation.
- A notable and significant limitation is the heightened risk of secondary cancers, believed to increase by up to 300% due to DNA damage resulting from therapeutic radiation exposure, as documented extensively by recent JAMA Oncology statistics for 2023.
Surgical Intervention: Effective, Yet Fraught with Potential Complications
Surgical approaches for Esophageal Cancer (Esophageal Carcinoma), particularly esophagectomy, bear severe inherent risks, especially among elderly patients and those with comorbidities, frequently encountered within the regional demographics of Hong Kong and other Asian nations.
- Surgical site infections represent a consistent postoperative complication. Despite advances in sterile technique and surgical prophylaxis, infection continues to complicate more than 22% of esophagectomies.
- Anastomotic leaks after radical surgery also remain alarmingly common. Leak rates continue to be reported at 8–14%, significantly increasing hospital stays, caregiving dependency, healthcare costs, psychological distress, and morbidity.
- Moreover, recovery from major operation procedures often results in extensive physical limitations and prolonged trauma, discouraging patients from seeking this necessary form of intervention promptly, thus diminishing overall patient survival rates regionally.
Understanding Metabolic Resistance Mechanisms in Esophageal Cancer (Esophageal Carcinoma)
Traditional therapies are further hindered by the sophisticated metabolic adaptations that Esophageal Cancer (Esophageal Carcinoma) cells develop over time. These cancer cells notably utilize high glucose intake (Warburg effect), enabling rapid proliferation and tumor progression despite therapeutic attempts.
- It has been documented that Esophageal Cancer (Esophageal Carcinoma) cells have up to 400% increased activity in DNA repair enzymes, markedly reducing effectiveness of traditional therapies including chemo- and radiotherapy, according to JAMA Oncology 2023.
- Additionally, glutamine addiction, a distinct metabolic dependence identified in numerous advanced esophageal tumors, provides a means for cancer cells to evade metabolic suppression treatments, challenging traditional treatment paradigms.
- Regional metabolic profiling of Esophageal Cancer (Esophageal Carcinoma) patients in Hong Kong emphasizes these metabolic vulnerabilities frequently observed across the Asian population, thereby underscoring regional priority of developing targeted therapeutic innovations.
Impact on Patients and Regional Limitations in Hong Kong and Asia
The empirical limitations of traditional therapy for Esophageal Cancer (Esophageal Carcinoma) in the Hong Kong and broader Asian region further aggravate patient outcomes, imposing burdens beyond the physical manifestations of cancer therapy. Cultural, dietary, genetic, and socioeconomic factors in this region frequently intersect with medical challenges.
- Due to limited access to specialized cancer care facilities, delays in diagnosis and prompt intervention remain persistent regional concerns, limiting effectiveness of traditional therapies.
- Cultural reluctance to promptly seek Western medical interventions sometimes exacerbates presentation of late-stage disease, negatively impacting responsiveness to chemotherapy or radiation.
- Genetic susceptibilities, such as variation in metabolic enzyme activities widely reported across East and Southeast Asian populations, present further complications, notably impaired drug metabolism escalating toxicities related to chemotherapy agents.
Conclusion: A Call for Novel Therapeutic Approaches
Considering the severe limitations and tangible challenges of conventional therapies in Esophageal Cancer (Esophageal Carcinoma), there remains a clear and urgent necessity for innovative therapeutic strategies in oncology practice. Advances such as metabolic targeting and immune checkpoint inhibitors, supported by robust Nobel-winning research and clinical validation, must be explored carefully in regional contexts to significantly enhance patient outcomes, maximize efficacy, and minimize associated therapeutic toxicities.