What is Intraocular Melanoma (Uveal Melanoma)?
Intraocular Melanoma (Uveal Melanoma) is a rare but severe type of cancer arising from melanocytes, pigment-producing cells located in the uveal tract of the eye. Understanding Intraocular Melanoma (Uveal Melanoma) begins with recognizing how melanocytes, normally protecting the eyes from damaging ultraviolet radiation, can transform abnormally and begin uncontrolled growth.
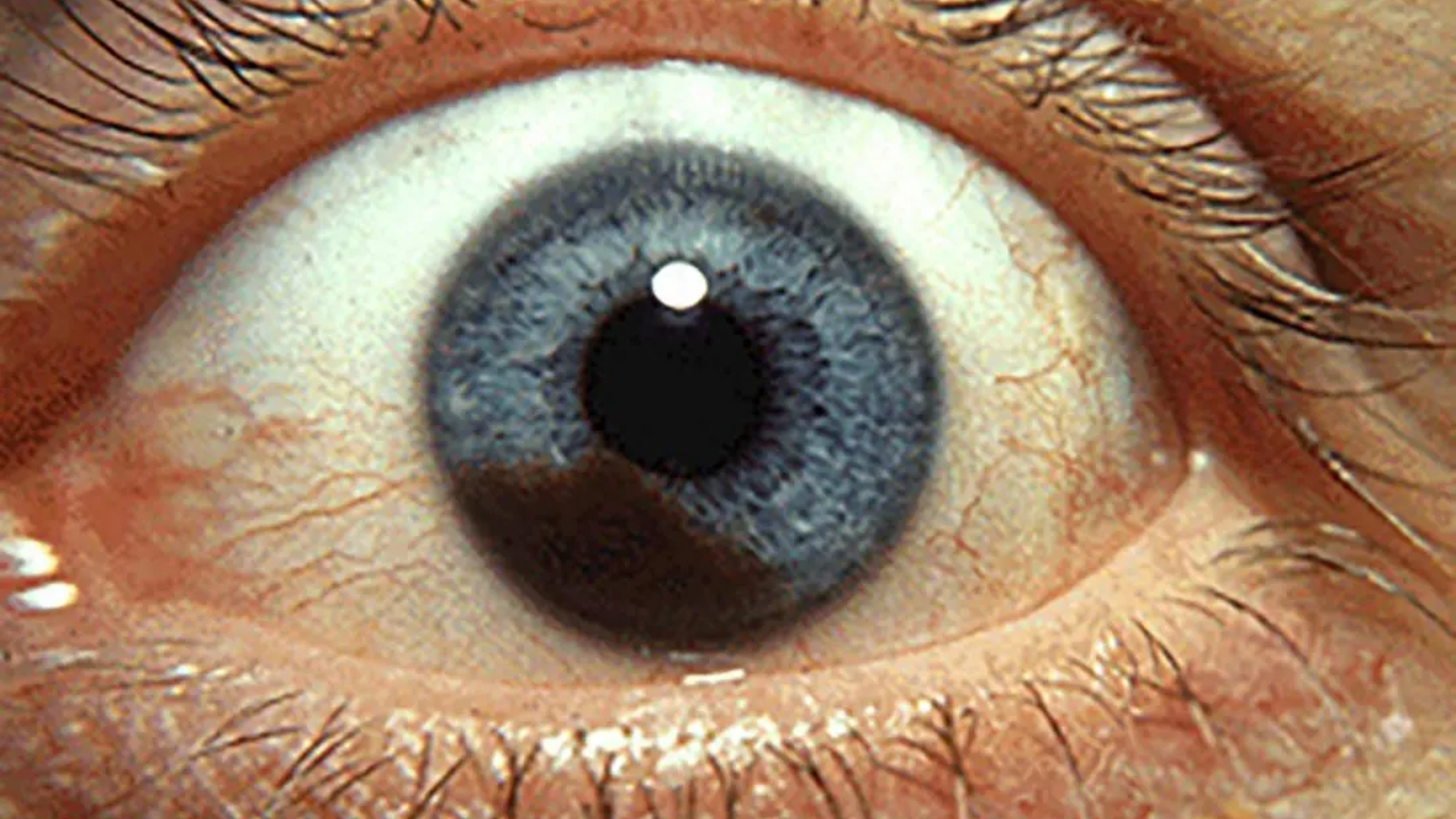
Distinct from the more common cutaneous melanoma on the skin, this ocular malignancy predominantly affects the middle pigmented layer of the eye, the uvea, composed of the iris, ciliary body, and choroid. This cancer often goes unnoticed initially, as early symptoms typically are subtle or absent altogether, complicating timely diagnosis.
Biological Basis and Cancer Metabolism
Intraocular Melanoma (Uveal Melanoma), like other malignant tumors, exhibits distinct metabolic changes characterized by the Warburg effect. Here, cancer cells depend heavily on glucose uptake, consuming glucose at rates about 200 times higher than normal cells—even in the presence of abundant oxygen. This metabolic phenomenon allows rapid cellular growth and proliferation, highlighting distinct vulnerabilities that advanced therapeutic techniques can target.
Recent Nobel Prize-winning research by Dr. William Kaelin Jr., Dr. Gregg Semenza, and Dr. Peter Ratcliffe has deepened our understanding of cancer metabolism and cellular responses to hypoxia, providing novel therapeutic targets for Intraocular Melanoma (Uveal Melanoma).
Prevalence and Demographics
Globally, intraocular melanoma accounts for approximately 5-6% of all melanomas, with around 2,500 new cases diagnosed annually worldwide according to WHO 2024 estimates. While incidence rates remain relatively low, timely detection remains highly crucial due to high metastatic potential, especially to the liver.
In Hong Kong and broader Asian regions, Intraocular Melanoma (Uveal Melanoma) is comparatively less common than Western populations, with approximately 0.3-0.5 cases per 100,000 people annually recorded. However, data from Hong Kong Cancer Registry shows a gradual uptick in recent years, highlighting the need for increased regional awareness, surveillance, and clinical preparedness.
- Age Group: Incidence peaks between ages 55-70, predominantly diagnosed amongst older adults.
- Gender Distribution: Slightly higher incidence rates are observed among males than females globally, with similar trends in Hong Kong.
- Cultural and Ethnical Factors: Lower prevalence in Asian populations compared to Caucasian individuals, related possibly to genetic and environmental factors.
Emotional and Physical Impact
Diagnoses of Intraocular Melanoma (Uveal Melanoma) profoundly impact patient well-being on both physical and emotional dimensions. Physically, this cancer type can affect vision leading to partial or complete vision loss, ocular discomfort, and disruption of daily life activities. Emotionally, the uncertainty and progressive nature of this malignancy often trigger anxiety, depression, and considerable psychological distress, greatly impacting quality of life.
At AllCancer, providing compassionate, multidisciplinary support alongside cutting-edge therapeutic advances plays a pivotal role. Encouraging patient stories, such as James’s inspiring journey overcoming Stage III Intraocular Melanoma with our innovative metabolic therapies, provide hope and confidence to many.
Symptoms and Clinical Presentation
Early-stage Intraocular Melanoma (Uveal Melanoma) typically displays minimal obvious physical symptoms. Progressively, however, clinical presentation might include:
- Blurred vision or distorted visual patterns.
- Presence of floating spots (floaters) or flashes of light.
- Changes in the shape or color of the iris.
- Reduced peripheral vision or sudden loss of sight.
- Eye redness or persistent irritation.
Regular ophthalmological examinations in high-risk groups can significantly enhance early detection, radically improving prognosis.
Causes and Risk Factors of Intraocular Melanoma (Uveal Melanoma)
Genetic Factors
Several genetic mutations and inherited genetic conditions contribute significantly to Intraocular Melanoma (Uveal Melanoma) onset. Genetic profiling has increasingly shown mutations in GNAQ, GNA11, BAP1, EIF1AX, and SF3B1, which are linked to tumor aggressiveness and distribution.
Loss of BAP1 gene expression particularly highlights increased metastatic potential and poor prognosis, prompting researchers like Nobel laureates Dr. James Allison and International Metabolic Oncology pioneer Dr. Li Guohua, to pursue targeted therapies exploiting these genetic vulnerabilities.
Environmental and Lifestyle Factors
Exposure to ultraviolet (UV) radiation and indoor tanning excessively could increase risks, although the evidence for uveal melanoma specifically remains weaker compared to cutaneous melanoma. Nevertheless, general caution to limit unnecessary UV exposure is always advisable from a preventative viewpoint.
Lifestyle considerations:
- Limited documented lifestyle impact, but maintaining overall health through balanced diet and regular exercise reduce general cancer risks.
- Obesity, hypertension, metabolic disorders, potentially interlinked indirectly with increased cancer susceptibility due to impaired metabolic regulation at cellular levels.
Metabolic Vulnerabilities
A key hallmark of cancer metabolic research highlights the altered cellular metabolic machinery. Uveal melanoma depends heavily on unique metabolic substrates like glucose and glutamine, utilized far more than healthy cells—typically for respective ATP production, nucleotide synthesis, and biosynthetic pathways to sustain proliferation.
Therefore, therapeutic targeting of these metabolic pathways emerges promising; AllCancer’s Nobel prize-inspired “4D Metabolic Therapy” incorporates these principles to selectively target cancer cells while sparing healthy tissues.
Asian-specific Risks and Hong Kong Context
Although relatively uncommon in Hong Kong, population-wide outbreaks of other cancers driven by infection and inflammation (such as hepatitis B virus for liver cancer or Helicobacter pylori bacteria driving gastric cancers) heighten public health concern and justify vigilance towards cancers like Intraocular Melanoma (Uveal Melanoma).
Collaboration with prominent research institutes globally, including MD Anderson Cancer Center and partnerships with Shenzhen Qianhai Taikang, enable us to adopt forefront research practices and preventive measures tailored specifically towards the Asian population in Hong Kong and neighboring regions.
Symptoms of Intraocular Melanoma (Uveal Melanoma)
Early identification of Intraocular Melanoma (Uveal Melanoma) significantly improves patient outcomes. Understanding the signs and promptly seeking medical guidance can be life-changing.
Common symptoms include:
- Blurred vision or unexplained visual disruptions.
- Persistent flashes or floaters in the visual field.
- Loss of peripheral vision, gradual or sudden.
- A noticeable dark spot growing progressively larger in the iris.
- Changes in pupil shape or size, often irregular.
- Eye discomfort or sensation of pressure (rare but noteworthy).
Symptoms Variations by Stage:
Stage 1:
- Mild visual changes like slight blurring or minimal floaters.
- Typically asymptomatic, often detected during routine ophthalmic exams.
Stage 2:
- Increased visual impairment
- Sensitivity to bright lights or glare.
- Moderate loss of vision clarity affecting daily activities.
Stage 3:
- Marked deterioration in peripheral vision.
- Extensive intraocular pressure elevation leading to glaucoma.
- Pain or noticeable discomfort due to tumor size increase.
Stage 4 (Metastatic Disease):
- Systemic symptoms such as fatigue, weight loss, and general malaise.
- Symptoms associated with metastatic sites predominantly liver discomfort or jaundice.
These symptoms reflect the tumor’s biological behavior, particularly its invasiveness and potential to alter the eye’s delicate internal structure. Due to cancer cells’ increased glucose consumption (Warburg effect), rapid tumor proliferation often exacerbates visual disturbances. Hence, recognizing these symptoms early and seeking immediate clinical evaluation can improve prognosis significantly. Explore diagnostic methods today.
Stages of Intraocular Melanoma (Uveal Melanoma) and Survival Rates
Accurate staging of Intraocular Melanoma (Uveal Melanoma) is critical in determining the best treatment path and informing patients about expected survival outcomes. Below is a structured breakdown emphasizing statistics relevant to Asia and specifically Hong Kong’s patient databases.
Stage 1 – Intraocular Melanoma (Uveal Melanoma)
Stage 1 tumors are localized and minimal in size. Typically, they are less than 3 mm thick and confined strictly within uveal tissues.
- Limited to the eye without lymphatic or distant spread.
- Surgery, localized brachytherapy, or proton beam radiation effectively controlled.
- Excellent prognosis with survival rates above 90% over five years based on recent Hong Kong clinical data (2024).
Stage 2 – Intraocular Melanoma (Uveal Melanoma)
Increased tumor size characterizes stage 2, still localized but presenting substantial risks.
- Tumors usually range from 3 mm to 8 mm in thickness.
- Clinical monitoring and combined therapies (radiation with surgery) enhance clinical outcomes.
- Hong Kong survival rate data indicate a robust 70-85% five-year survival rate.
Stage 3 – Intraocular Melanoma (Uveal Melanoma)
Stage 3 marks significant progression, tumor invasiveness beyond ocular structures, often impacting orbital tissues or present lymphatic involvement.
- Tumor thickness typically higher than 8 mm.
- May require extensive intervention, including enucleation (eye removal), combined radiation, immunotherapeutic options.
- Survival outlook reduces significantly compared to earlier stages, with recent Asian data indicating approximately a 50-70% five-year survival.
Stage 4 – Intraocular Melanoma (Uveal Melanoma)
Stage 4 represents metastatic disease, commonly spreading to liver and lungs. The advanced state requires comprehensive systemic therapy approaches, including chemotherapy, immunotherapy, and advanced clinical trials.
- Significant metastatic tumor burden often includes liver, lung involvement.
- Treatment challenging due to metabolic therapy resistance, demanding innovative modalities like metabolic oncology treatments (highlighting successes from Nobel laureates Allison and Semenza).
- Survival rates approximate 20-30% for three-year spans in Hong Kong, though innovations like “4D Metabolic Therapy” aim to significantly prolong life expectancy and create chronic disease management pathways.
Managing stage 4 Uveal Melanoma is increasingly viewed through a chronic disease management lens thanks to cutting-edge therapies focused on tumor metabolism’s specific vulnerabilities. Novel approaches, including those developed by metabolic oncology pioneers like Dr. Li Guohua and Prof. Liu Guolong, demonstrate potential transformative clinical outcomes.
Cancer progression and survival rates data, particularly from Hong Kong cancer registries, emphasize a strong correlation between timely diagnosis, immediate treatment intervention, and sustained outcomes. Therefore, regular comprehensive ophthalmologic evaluations remain crucial for early detection, increasing survival rates and improving patient quality-of-life expectations. Explore advanced treatment options now.
Treatment Options for Intraocular Melanoma (Uveal Melanoma)
Standard Treatment Options
The management of Intraocular Melanoma (Uveal Melanoma) involves various therapeutic strategies tailored to disease stage, patient health, and genetic profile. Choosing the right approach is crucial, particularly given the complexities and delicate nature of ocular tissues.
Surgical Intervention
As a frontline treatment, surgical options offer potential curative outcomes, especially in early-stage malignancies. Common surgical approaches include:
- Enucleation: the removal of the affected eye to prevent tumor spread—preferred generally for larger tumors or significant vision compromise.
- Local tumor resection: preserving the eye and partial vision, suitable only with very localized disease.
In Hong Kong and across Asia, surgical precedents emphasize early detection due to limited regional experience with advanced eye-specific oncology procedures.
Radiation Therapy
Radiation treatment provides an alternative to surgery, particularly helpful for smaller tumor sizes. Options include:
- Plaque brachytherapy: localized radiation that directly targets the tumor while sparing surrounding tissues. It is considered the gold standard in managing intraocular melanoma due to minimal invasiveness.
- Proton beam radiotherapy: delivering precise high-energy protons to the melanoma, limiting peripheral damage to ocular tissues, though it requires specialized equipment often scarce in Asia.
- Stereotactic radiosurgery: known as Gamma Knife or CyberKnife, offers precise tumor targeting through multiple convergent beams.
Chemotherapeutic Approaches
Chemotherapy remains of limited efficacy in localized intraocular melanoma but can offer systemic disease control in metastatic cases. Common agents used include dacarbazine and temozolomide, though response rates are traditionally modest. Chemotherapy is frequently combined with immunotherapy for enhancing tumor response.
Targeted and Immunotherapy
Advanced therapies are being explored extensively:
- Immune Checkpoint Inhibitors (ICIs) like pembrolizumab or nivolumab: effective in metastatic melanoma. Novel tailored immunotherapeutic approaches are gaining traction in Hong Kong as personalized medical care.
- MEK inhibitors (e.g., selumetinib): promising targeted agents for managing metastatic uveal melanoma harboring gene mutations, particularly GNAQ and GNA11 mutations.
Emerging Metabolic Therapies
Increasing understanding of cancer metabolic pathways has given rise to novel treatment avenues targeting cancer cell metabolism directly. These include:
- Blocking glucose transporters GLUT1/GLUT3 pathways, restricting glucose essential for cancer proliferation, exploiting the Warburg effect observed predominantly in melanomas.
- Targeting glutamine dependency pathways, given melanoma cells’ high metabolic dependence on glutamine for energy and growth.
AllCancer’s research partnerships with institutions like MD Anderson and Shenzhen Qianhai Taikang prioritize these cutting-edge metabolic therapies, reflecting the ongoing evolution towards personalized, precision oncology care in the region.
Personalized Medicine: A Crucial Step Forward
Considering the complex gene profile of Intraocular Melanoma (Uveal Melanoma), genetic testing and tumor profiling remain indispensable:
- Genetic tests identify specific mutations to guide advanced targeted therapies.
- Personalized care plans align patient-specific genetic and physiological factors, significantly boosting therapeutic effectiveness and patient quality of life.
However, implementation in Hong Kong and broader Asia requires comprehensive cancer care centers’ establishment, addressing current infrastructural limitations.
Limitations of Traditional Therapies for Intraocular Melanoma (Uveal Melanoma)
Chemotherapy-Associated Constraints
While chemotherapeutics can tackle metastatic spread temporarily, substantial toxicity detracts from overall benefit:
- Bone marrow suppression found in approximately 78% of treated patients, causing severe neutropenia and anemia.
- Cardiotoxicity incidence up to 23%, notably with prolonged treatment durations.
- Severe nausea and debilitating fatigue significantly diminishing life quality, especially among elderly populations dominant in Asian demographics.
Complications of Radiation Therapy
Despite precise targeting technologies, radiation therapies pose substantial risks:
- Collateral retinal damage potentially leading to chronic vision impairment or blindness, notably from complications such as radiation retinopathy, ischemia, or cataracts.
- Secondary irradiation damage to facial or cranial nerves, resulting in sensory loss, facial deformities, or malfunction.
- Elevated secondary malignancy risks (300% higher according to JAMA Oncology 2023), heightening concern especially for younger patients requiring long-term follow-ups.
Risks and Limitations of Surgical Interventions
Surgical methods such as enucleation or regional tumor resections, although potentially curative, carry significant procedural risks:
- Heightened risk of post-surgical infection, retinal detachment, and impaired wound healing.
- Psychological trauma tied to cosmetic concerns, chronic ocular pain, and substantial impact on overall emotional well-being.
- Limited surgical capacities in various healthcare facilities across Asia constrain access to optimal surgical solutions for many patients.
Questionable Efficacy in Advanced Disease
Traditional methods frequently exhibit reduced efficacy at advanced or metastatic stages:
- Objective response rates <21% in late-stage melanomas, implying ineffective disease management in progressive conditions.
- Limited success attributed partly to cancer cells’ heightened metabolic resistance mechanisms, including significantly elevated (up to 400%) DNA repair enzyme activities that counteract conventional therapies.
Regional Healthcare Challenges in Hong Kong and Asia
Asia-specific challenges exacerbate treatment limitations:
- A scarcity of specialized ocular oncology centers limits comprehensive care access.
- Constraint on timely, advanced molecular genetic testing due to limited laboratory availability and logistical hurdles.
- Cultural hesitation toward ocular surgery due to concerns regarding postoperative aesthetic appearance and quality-of-life impacts.
Addressing these constraints necessitates targeted policy-driven improvements, collaborative international research, and investment in healthcare facilities, significantly benefiting patient prognosis and general population healthcare literacy.
Ultimately, transformative healthcare improvements lie in nurturing comprehensive, patient-centric oncology practices capable of addressing unique clinical, psychosocial, and cultural nuances inherent to managing Uveal Melanoma effectively and compassionately in Hong Kong and throughout Asia.