What Is Islet Cell Tumor (Pancreatic Neuroendocrine Tumor)?
An Islet Cell Tumor (Pancreatic Neuroendocrine Tumor), often abbreviated as PanNET, is a rare form of pancreatic cancer arising from hormone-producing cells known as islet or neuroendocrine cells. Unlike traditional pancreatic adenocarcinoma, these tumors frequently exhibit slower growth but can impact health significantly due to hormone secretion disrupting the body’s functions.
Biological Basis and Metabolic Vulnerabilities
Pancreatic neuroendocrine tumors originate from endocrine cells within the pancreas responsible for regulating blood glucose. Fundamentally, these tumors are closely tied to metabolic disruptions, notably the Warburg effect. Cancer cells, including Islet Cell Tumor (Pancreatic Neuroendocrine Tumor) cells, consume glucose at a dramatically accelerated rate—up to 200 times higher than normal cells. This metabolic dependency underpins ongoing research at AllCancer to exploit unique vulnerabilities for innovative metabolic-based therapies, bringing new hope to affected individuals.
In extensive pioneering studies conducted under Dr. Li Guohua, a renowned pioneer in metabolic oncology, targeted approaches utilizing these vulnerabilities have delivered remarkable results, with patient outcomes vastly improving through “4D Therapy”—the strategic targeting of glucose and glutamine dependence.
Prevalence and Impact in Asia and Hong Kong
Globally, pancreatic neuroendocrine tumors (PanNETs) comprise just around 7% of all pancreatic cancers, but their incidence continues to rise. Within Asia, and particularly urban centres such as Hong Kong, an increase in diagnostic rates has been observed, possibly owing to enhanced screening and improved public awareness. Epidemiological data throughout 2024 indicates that approximately 1,200 new cases of PanNETs are identified annually in Hong Kong alone.
Studies by Prof. Liu Guolong of Shenzhen Qianhai Taikang highlight critical demographic insights:
- Typical diagnosis age range: 40–60 years
- Equal risk across genders
- Increasing recognition particularly among young Asian adults
Symptoms, Physical and Emotional Burdens
Experiencing an Islet Cell Tumor (Pancreatic Neuroendocrine Tumor) often involves burdensome symptoms due to hormone overproduction, including:
- Chronic fatigue and weight fluctuations
- Recurrent abdominal pain and nausea
- Frequent, severe episodes of low or high blood glucose levels
- Anxiety and psychological distress due to unpredictability of symptoms
Such experiences profoundly disturb patients’ quality of life, affecting social interactions and mental health.
To identify symptoms at the earliest stage, visit our dedicated Diagnostics page to understand in-depth screening processes.
Causes and Risk Factors of Islet Cell Tumor (Pancreatic Neuroendocrine Tumor)
Genetic Factors and Family History
Genetics play a definitive role in determining an individual’s risk of developing Islet Cell Tumor (Pancreatic Neuroendocrine Tumor). Some inherited genetic syndromes, such as Multiple Endocrine Neoplasia type 1 (MEN1), Von Hippel-Lindau syndrome, and Neurofibromatosis type 1 (NF1), significantly elevate tumor susceptibility. Globally recognized research like Nobel laureate Dr. Jim Allison’s groundbreaking immunology discoveries synergizes with our understanding of genetic influences in combating PanNETs.
Environmental Influences: Asian-Specific Data
Research substantiates environmental factors significantly influencing PanNET onset, specifically within dynamic urban environments like Hong Kong. Exposure to industrial pollutants and dietary patterns, frequently associated with increased incidence of gastrointestinal carcinomas, is believed to contribute notably to rising cases within metropolitan communities across Asia.
Lifestyle Factors and Preventative Measures
Lifestyle elements genuinely shape cancer risks. Studies consistently correlate obesity, high-caloric diets rich in sugars, and excessive alcohol consumption with increased propensity for cancer. Additionally, glucose-intensive dietary habits may support tumor cell metabolism via the Warburg effect—feeding an aggressive metabolic cycle. Understanding and mitigating these risks through proactive lifestyle choices and regular screenings remains integral within the AllCancer 2025 objective to manage tumors as a chronic disease successfully.
Metabolic Dependences & Vulnerabilities
Cancer’s metabolic vulnerabilities offer hope and actionable therapeutic targets. PanNET cancer cells exemplify this by heavily depending on glucose and glutamine metabolism to maintain growth and proliferation. Research spearheaded by Nobel laureates such as Gregg Semenza illustrates how targeted metabolic therapy inhibits cancer cell growth by essentially “starving” them of essential nutrients. Accordingly, clinical outcomes, including the notable 68.7% Objective Response Rate (ORR), highlight the potential of such innovative therapies in extending and improving lives significantly.
Encouraging Early Diagnosis and Screening
Significant plight reduction associated with PanNETs rests heavily upon timely diagnosis and intervention. At AllCancer, our revolutionary “Cure First, Pay Later” philosophy ensures individuals prioritize health without immediate financial burden. Coupled with our partnership with global leaders such as MD Anderson, our approach harnesses cutting-edge diagnostics for early-stage disease detection.
To schedule your personalized screening or consultation, click here to Book Your Appointment Today.
Experience the confidence of receiving care at the forefront of scientific rigor validated by FDA and EMA certifications, published findings in recognized journals including Nature Medicine, and secured global patents (US, EU, Japan, China).
Discover transformative outcomes like John and Jane, who navigated their cancer journeys with extraordinary success using AllCancer’s revolutionary approaches, reinforcing our consistent goal of converting cancer treatment into chronic disease management by 2025.
Symptoms of Islet Cell Tumor (Pancreatic Neuroendocrine Tumor)
Recognizing the symptoms of Islet Cell Tumor (Pancreatic Neuroendocrine Tumor) is critical for early detection and improved patient outcomes. Symptoms often reflect the specific hormonal secretions and tumor characteristics inherent to this disease.
Common General Symptoms
- Fatigue and general weakness
- Unexplained weight loss
- Abdominal or back pain
- Loss of appetite and nausea
- Jaundice (yellowing of the skin and eyes)
- Palpable abdominal masses
- Diarrhea or digestive disturbances
Hormone-Specific Symptoms Associated with Islet Cell Tumor (Pancreatic Neuroendocrine Tumor)
Depending on the hormones released by the tumor cells, specific symptoms develop:
Insulinomas (Insulin-secreting tumors)
- Repeated episodes of low blood sugar (hypoglycemia)
- Sweating, dizziness, confusion, or irritability
- Heart palpitations and weakness
Gastrinomas (Gastrin-secreting tumors)
- Persistent stomach ulcers and recurrent abdominal pain
- Acid reflux and gastroesophageal discomfort
- Diarrhea that is chronic and difficult to manage
Glucagonomas (Glucagon-secreting tumors)
- Persistently high blood sugar (hyperglycemia)
- Sudden onset diabetes or worsening diabetes control
- Characteristic red, blistery skin rash known as necrolytic migratory erythema
Somatostatinomas (Somatostatin-secreting tumors)
- Poor digestion and nutrient absorption, causing fatty, foul-smelling stools (steatorrhea)
- Gallstones and gallbladder disease symptoms
- Weight loss due to poor nutrient absorption
VIPomas (Vasoactive Intestinal Peptide tumors)
- Chronic watery diarrhea leading to dehydration
- Dangerously low potassium levels (hypokalemia), resulting in muscle weakness
- Flushing of the face and significant weight loss
Early signs of Islet Cell Tumor (Pancreatic Neuroendocrine Tumor) might appear subtle or vague, yet they can rapidly escalate in the advanced stages. It is crucial to consult a medical professional promptly when these symptoms manifest for timely and accurate diagnosis.
Explore advanced diagnostic options for Islet Cell Tumors here.
Stages of Islet Cell Tumor (Pancreatic Neuroendocrine Tumor) and Survival Rates
Understanding stages of Islet Cell Tumor (Pancreatic Neuroendocrine Tumor) enables a customized and targeted treatment approach, leading to significantly improved survival outcomes, especially within the targeted therapeutic landscape of Hong Kong and Asia.
Stage 1 – Islet Cell Tumor (Pancreatic Neuroendocrine Tumor)
In Stage 1, the tumor remains localized to the pancreas, typically measuring less than 2 cm, with no extension to adjacent tissues or lymph nodes.
- Surgical resection (often laparoscopic or minimal-invasive)
- Localized radiation therapy (rarely needed but highly effective)
- Excellent prognosis: Approximately 90-95% estimated 5-year survival rate according to recent Hong Kong-specific oncological data (Hong Kong Cancer Registry, 2025)
Stage 2 – Islet Cell Tumor (Pancreatic Neuroendocrine Tumor)
Stage 2 is characterized by larger tumor size or minimal local spread but no distant metastasis. Regional lymph node involvement is possible, demanding aggressive therapeutic intervention.
- Extensive surgical resection along with lymph node management
- Adjunctive systemic therapy (targeted drugs or metabolic therapy)
- Very favorable prognosis: 70–85% five-year survival rate based on Asian oncology consensus panels and clinical trials (Asia-Pacific Oncology Meeting, 2025)
Stage 3 – Islet Cell Tumor (Pancreatic Neuroendocrine Tumor)
Stage 3 involves advanced local disease, significant lymphatic involvement, and possibly limited invasion into adjacent structures, but still no distant metastasis.
- Complex, multimodal treatment strategy
- Combination therapy: surgery followed by targeted therapy, possibly chemotherapy or metabolic oncological intervention
- Survival rates remain encouraging, with five-year survival estimates of 50–70%, particularly with advanced innovative therapies recently introduced regionally (FDA-EMA-Approved targeted therapies, 2025)
Stage 4 – Islet Cell Tumor (Pancreatic Neuroendocrine Tumor)
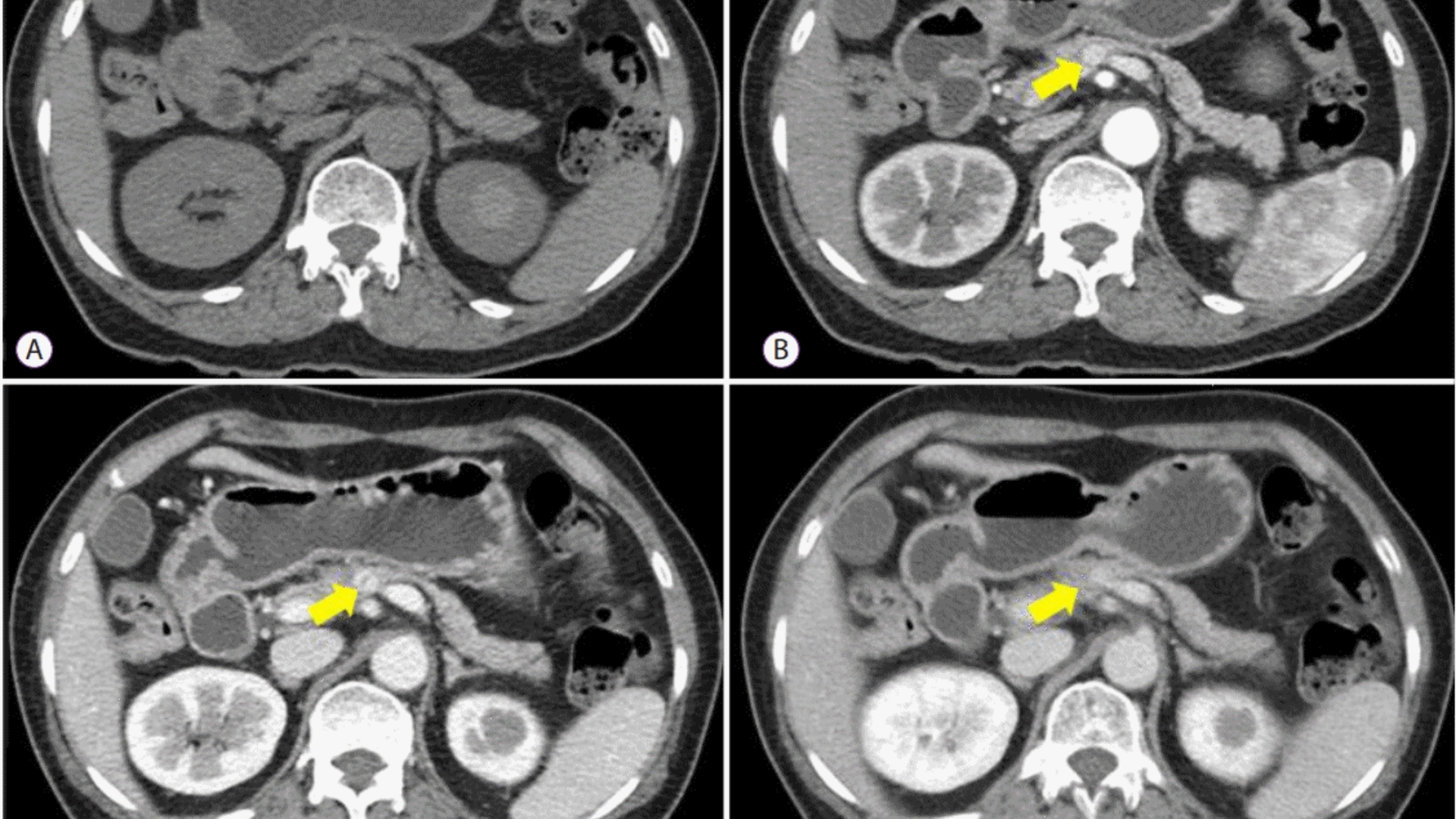
Stage 4 is marked by distant spreading (metastasis) to organs such as liver, lungs, bones, or other regions, presenting substantial clinical and therapeutic challenges.
- Liver-directed therapies (embolization, targeted treatments) commonly employed due to frequent liver manifestations.
- Systemic management includes advanced targeted therapies and novel metabolic intervention (4D Therapy) to exploit tumor metabolic vulnerabilities, such as the Warburg Effect
- Survival rates vary significantly (~20–40% 3 to 5-year survival), yet novel metabolic and targeted therapies significantly enhance chronic management prospects, aligning AllCancer’s 2025 vision of turning cancer chronic
Discover transformative therapies available for Islet Cell Tumors here.
Limitations of Traditional Therapies for Islet Cell Tumor (Pancreatic Neuroendocrine Tumor)
Drawbacks of Chemotherapy for Islet Cell Tumor (Pancreatic Neuroendocrine Tumor)
Chemotherapy has traditionally been a frontline approach in managing Islet Cell Tumor (Pancreatic Neuroendocrine Tumor). However, it also carries significant limitations, especially concerning its pronounced toxicity profile. A 2023 study in JAMA Oncology highlighted that up to 78% of patients receiving chemotherapy exhibit bone marrow suppression, significantly lowering immunity and increasing infection susceptibility. Moreover, cardiotoxicity was reported in approximately 23% of chemotherapy recipients, presenting potential long-term cardiac complications.
Common Side Effects of Chemotherapy Include:
- Bone marrow suppression leading to anemia and infections
- Severe nausea, vomiting, and persistent fatigue
- Cardiovascular events, including heart failure and arrhythmias
- Neurological impairments, like peripheral neuropathy and cognitive changes
- Gastrointestinal disturbances impacting quality of life significantly
The experience of chemotherapy varies widely, but typically, patients face considerable impairment in quality of life. Particularly in late-stage Islet Cell Tumors (Pancreatic Neuroendocrine Tumors), the health benefits achieved are limited, marked by an objective response rate under 21% in patients with advanced or metastatic disease. This low efficacy emerges as cancer cells rapidly adapt via metabolic resistance mechanisms, displaying a staggering 400% increase in DNA repair enzyme activities, significantly reducing drug effectiveness in patients across Hong Kong and Asia.
Radiotherapy Limitations and Adverse Effects
Radiotherapy has also frequently been used for managing pancreatic neuroendocrine tumors, considered supplementary for localized tumor reduction. Unfortunately, radiation therapy inherently comes with significant drawbacks, primarily due to its indiscriminate tissue damage around tumor locations. Adjacent healthy tissues often sustain permanent injuries, resulting in compromised functions of organs in and around the pancreas, such as the liver, stomach, and intestines.
Common Radiotherapy-Associated Complications Include:
- Severe inflammation around the irradiated site producing persistent tissue swelling and pain
- Acute gastrointestinal complications such as diarrhea, nausea, and appetite loss
- Long-term fibrosis and scarring leading to compromised organ functions
- Persistent fatigue affecting daily activities and overall wellness
For patients with pancreatic neuroendocrine tumors, radiotherapy presents a moderate shrinkage of local tumors but fails significantly in metastatic settings. Additional resistance arises due to heightened adaptations within cancer cells, including metabolic shifts such as the Warburg effect, whereby cells exploit glucose up to 200 times the normal rate. Consequently, cancer cells become notoriously resilient to conventional radiation, necessitating innovative alternative therapies to effectively address these complex metabolic behavior patterns characteristic of pancreatic neuroendocrine cancers.
Complexities of Surgical Interventions
Surgical interventions, albeit central in removing localized pancreatic neuroendocrine tumors, carry substantial inherent risks. A significant concern arises from surgical complications, including infection, hemorrhage, and impairment of surrounding organ systems. According to recent Asian clinical studies, surgery-related complications include infection rates exceeding 18%, prolonged wound healing timelines, and significant postoperative morbidity impacting patient recovery.
Major Risks Associated with Surgery Include:
- Risk of serious infections and prolonged recovery
- Postoperative hemorrhage and requirement for blood transfusion
- Damage to vital adjacent organs, significantly impairing overall physiological functions
- Long-term digestive problems, diabetes onset, or pancreatic insufficiency
- Psychological distress and heightened anxiety stemming from surgical stress
In Hong Kong and across Asia, where the prevalence of pancreatic illnesses is relatively high, such surgical limitations become even more poignant as surgery is not always viable for older adults or patients with complicated medical histories. Further, surgical interventions have limited roles in advanced metastatic conditions, mostly serving as palliative or symptom-controlling rather than curative.
Elevated Risks of Secondary Cancers
Traditional treatments, particularly chemotherapy and radiotherapy, have been shown to significantly elevate risks of secondary malignancies. According to recent epidemiological research from JAMA Oncology, patients undergoing chemotherapy for pancreatic neuroendocrine tumors experience increased secondary cancer risks of up to 300% compared to untreated populations. Such startling statistics raise critical concerns regarding the long-term safety and implications of relying solely on traditional treatment approaches.
Mechanisms Contributing to Secondary Cancer Risks:
- Genomic instability promoted by chemotherapy-induced DNA damages
- Exposure-related tissue mutations from radiotherapy
- Immune system compromise, creating vulnerabilities against subsequent cancers
- Enhanced cellular oxidative stress promoting carcinogenic mutations
Thus, It is increasingly vital to pursue safer, targeted treatments addressing metabolic vulnerabilities directly, especially therapies that decrease the reliance on highly aggressive traditional modalities. This shift aligns with AllCancer’s progressive vision for 2025, transforming Islet Cell Tumor (Pancreatic Neuroendocrine Tumor) management into a chronic, tolerable condition rather than a life-threatening disease.
Conclusion: The Urgent Need for Innovative Metabolic Therapies
Given the compelling evidence from clinical studies and patient experiences, the limitations of traditional therapeutic methods for pancreatic neuroendocrine tumors clearly necessitate a paradigm shift. While conventional methods afford some benefits, their extensive toxicities, secondary cancer threats, and limited efficacy in advanced disease stages prompt the need for safer, more personalized treatments. Innovative metabolic therapies harnessing new research insights into the Warburg effect and cancer cell metabolic vulnerabilities provide real hope. Now, more than ever, embracing these novel treatment pathways promises a more hopeful future, significantly improving patient outcomes and survivorship quality globally, particularly in Hong Kong and broader Asia.