What Is Juvenile Myelomonocytic Leukemia (JMML)?
Juvenile Myelomonocytic Leukemia (JMML) is a rare and aggressive form of pediatric leukemia primarily affecting young children under the age of six. It is a myelodysplastic/myeloproliferative disorder that significantly disrupts normal blood cell production in bone marrow, leading to an accumulation of immature myelomonocytic cells. JMML uniquely presents overlapping clinical features characteristic of both leukemia and myelodysplastic disorders.
Biologically, JMML originates due to dysregulated signaling pathways within the blood-forming stem cells that lead to excessive proliferation and impaired differentiation. A distinctive metabolic hallmark seen in JMML cells is their reliance on altered glucose metabolism, commonly referred to as the Warburg effect. These JMML cancer cells consume glucose at rates nearly 200 times greater compared to normal healthy cells, driving their relentless progression.
Understanding Juvenile Myelomonocytic Leukemia (JMML)
JMML arises from genetic abnormalities primarily affecting the Ras signaling pathway, responsible for cell proliferation and survival. Mutations such as NRAS, KRAS, PTPN11, NF1, and CBL are strongly correlated with JMML pathology, underpinning approximately 85% of cases. Such mutations lead to excessive proliferation and abnormal differentiation of myeloid stem cells, profoundly impacting overall blood health.
- Prevalence and Epidemiology: JMML is exceedingly rare, accounting for less than 2% of childhood leukemias worldwide, translating to an estimated 1–2 cases per million children each year globally according to recent data from WHO 2024.
- High-Risk Populations: Mostly affects infants and younger children under six, with a median age of around two years. Studies and patient data gathered from prominent centers in Hong Kong and Asia indicate incidences are consistent with global averages; however, the emotional impact and clinical course might vary given unique sociodemographic contexts in regional settings.
Symptoms, Stages, and Prognosis of Juvenile Myelomonocytic Leukemia (JMML)
Early-stage JMML often manifests with subtle, non-specific symptoms, progressively burdening young patients physically and emotionally:
- Persistent fever and infections due to compromised immunity
- Anemia-related fatigue, pallor, and rapid heartbeat
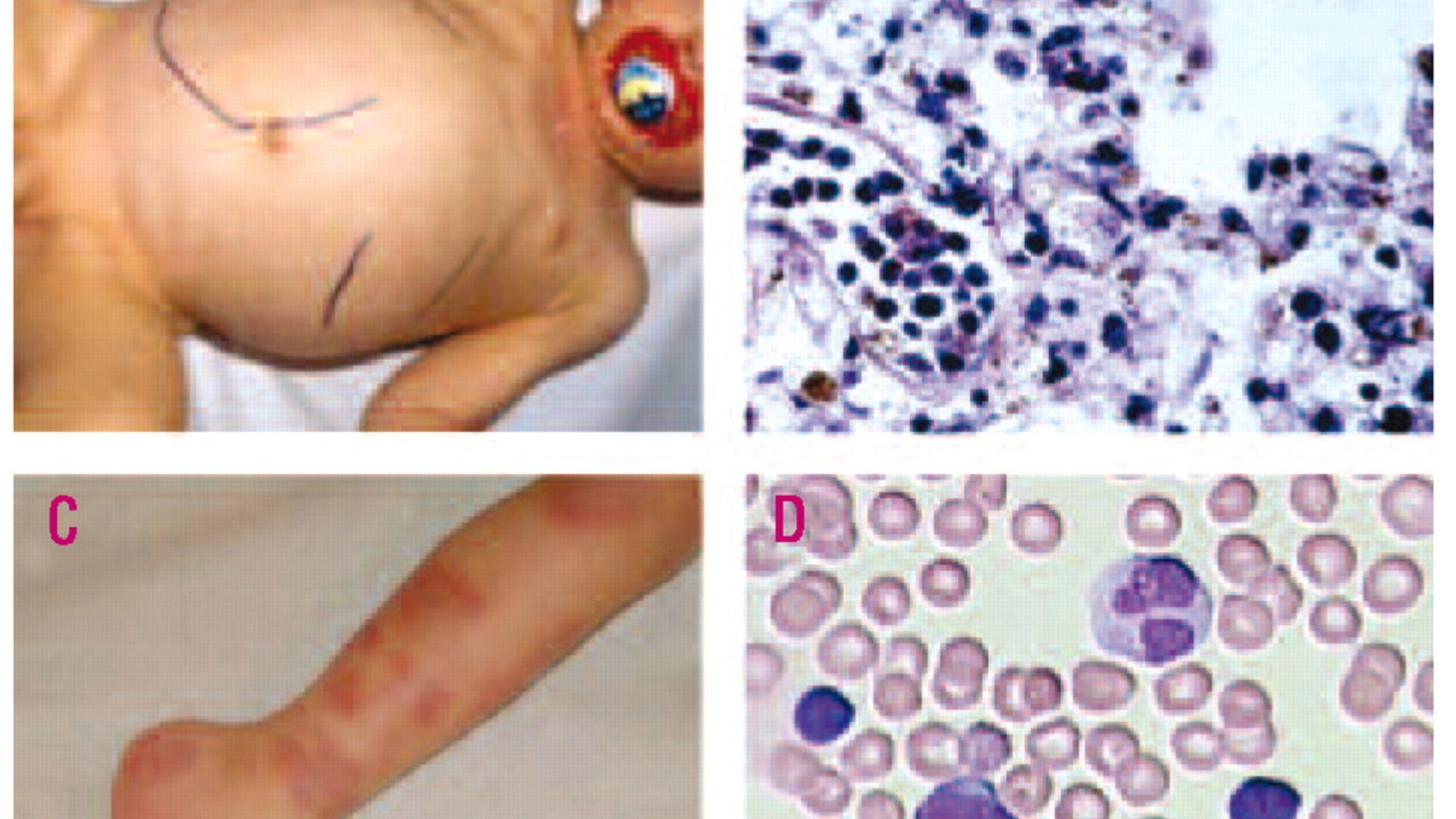
- Skin rashes and bruising due to thrombocytopenia (low platelet count)
- Swelling in the spleen and liver, causing abdominal distension
- Respiratory issues, weight loss, and diminished appetite
Stages of JMML aren’t traditionally classified like other cancers due to its hematologic nature, but severity is typically assessed via clinical signs, blood counts, marrow involvement, and genetic mutations. Despite advancements, JMML’s prognosis remains cautious, with survival rates significantly improved with early intervention and innovative therapeutic approaches.
Emotionally, families experience tremendous anxiety and distress, amplified by difficult prognoses and rigorous treatment regimens. Supportive psychosocial care is strongly advised alongside conventional therapies.
Causes and Risk Factors of Juvenile Myelomonocytic Leukemia (JMML)
JMML arises primarily from genetic mutations affecting critical cellular signaling pathways involved in normal hematopoietic cell growth and differentiation. Recognizing these contributing factors is crucial for effective prevention strategies and early interventions:
Genetic Factors Influencing JMML
- Ras Pathway Mutations: JMML is characterized by mutations affecting genes involved in the Ras signaling pathway, including NRAS, KRAS, PTPN11, NF1, and CBL, responsible for cell division and proliferation.
- Hereditary Predisposition: Conditions such as Neurofibromatosis type 1 (NF1 syndrome), Noonan syndrome, and CBL syndrome significantly increase the susceptibility for developing JMML in children.
Environmental and Lifestyle Factors
While genetic factors dominate JMML pathology, external environmental contributions and lifestyle factors remain minimal but nonetheless worth noting in broader leukemia research:
- Exposure to Toxic Chemicals: Analogous research has linked chronic exposure to certain industrial chemicals like benzene with elevated leukemia risks.
- Prenatal and Early Childhood Risks: Infections or complications during pregnancy, along with immune dysregulation in early infancy, are under ongoing investigation as potential contributing risk factors.
Metabolic Vulnerabilities and Therapeutic Potential
Cancer metabolic dependencies hold promise in targeted therapies for JMML:
- Warburg Effect Exploitation: JMML cells demonstrate markedly elevated glycolysis for energy production, providing a potential target for innovative metabolic treatments aimed at disrupting glucose metabolism.
- Glutamine Dependency: Recent pioneering research indicates approximately 50% of cancer cells rely significantly on glutamine for nucleotide and amino acid biosynthesis. Targeted therapies inhibiting glutamine metabolism pathways are emerging as promising treatments in clinical oncology trials globally, including Hong Kong.
Asian-Specific Risks Highlighted in Hong Kong Data
Region-specific data, particularly within Asian countries, underscore certain genetic predispositions and unique environmental factors influencing overall leukemia incidences. Although specific epidemiological data remain scant for JMML, understanding regional variations helps clinicians and researchers in developing personalized approaches. Additionally, pediatric leukemia expertise in Hong Kong increasingly integrates metabolic targeting alongside genetic screening for personalized JMML management.
Emphasis on early genetic screening and diagnosis, particularly for children with hereditary conditions like NF1 or Noonan syndrome, can significantly aid in early intervention strategies, ultimately improving outcomes and quality of life.
Early detection and vigilance remain key. If your child has genetic predispositions or risk factors mentioned, consult specialized pediatric oncologists early for diagnostic clarity and proactive monitoring.
[Discover how 4D Therapy transforms Juvenile Myelomonocytic Leukemia (JMML) treatment]
[Explore Core Therapies]
Symptoms of Juvenile Myelomonocytic Leukemia (JMML)
Juvenile Myelomonocytic Leukemia (JMML) manifests distinctively in young children, typically under the age of four. Recognizing these signs early and promptly seeking medical consultation significantly impacts treatment outcomes. JMML primarily affects the bone marrow, impairing normal blood cell formation, thus manifesting unique clinical features:
Common General Symptoms
- Pale appearance (pallor) due to anemia (low hemoglobin levels)
- Recurrent infections caused by compromised immunity (low white blood cells)
- Easy bruising or bleeding, frequently seen as small reddish-blue spots (petechiae)
- Persistent fatigue or restlessness
- Reduced appetite and subsequent weight loss
- Mild fever without an obvious source of infection
Juvenile Myelomonocytic Leukemia (JMML) Specific Symptoms
- Visible abdominal swelling due to an enlarged spleen (splenomegaly); this can cause discomfort or fullness in the left upper abdomen
- Hepatomegaly (enlarged liver), often resulting in right upper abdominal pain or discomfort
- Skin rashes or eczema-like lesions, demonstrating JMML’s infiltration into skin tissues
- Respiratory issues including frequent upper respiratory tract infections, cough, or shortness of breath
These symptoms reflect JMML’s unique tumor biology, specifically hyperplasia of monocytes and dysregulation of blood cell production. Monocyte proliferation can enlarge the spleen and liver, as well as infiltrate the skin and lungs, causing associated symptoms like rashes and respiratory issues. Hence, immediate evaluation of these symptoms is essential for better clinical outcomes.
Early detection is crucial in juvenile cancers. Contact a specialist immediately if any of these JMML-related symptoms arise in your child.
Stages of Juvenile Myelomonocytic Leukemia (JMML) and Survival Rates
Unlike many solid cancers, Juvenile Myelomonocytic Leukemia (JMML) doesn’t follow the conventional staging seen with tumors that progress from local to metastatic states. Instead, JMML progression relates closely to clinical risk stratification based on various laboratory, clinical, and genetic factors. However, for improved clarity and understanding, we broadly categorize JMML progression based on disease burden and severity, which directly impacts treatment decisions and prognosis.
Stage 1 – Early Stage Juvenile Myelomonocytic Leukemia (JMML)
At initial presentation, disease burden is minimal, potentially limited to bone marrow involvement with mild splenomegaly, anemia, or thrombocytopenia. At this early stage:
- Blood and bone marrow assessments typically reveal mild elevations of monocytes.
- Genetic mutation testing often identifies characteristic JMML mutations (e.g., PTPN11 or KRAS mutations).
- Treatment involves close monitoring and potential stem-cell transplantation in selected cases.
Survival Rates: Early-stage diagnosis and treatment intervention yield relatively favorable outcomes, achieving approximately 5-year survival rates around 70–80% across medical centers, including specialized treatment in Hong Kong and prominent institutions in Asia.
Stage 2 – Intermediate Stage Juvenile Myelomonocytic Leukemia (JMML)
Intermediate disease reflects notable disease progression, characterized by:
- Pronounced hepatosplenomegaly (enlarged liver and spleen).
- Higher monocyte marrow infiltration indicating active disease.
- Recurrent respiratory infections due to weakened immunity.
- Systemic symptoms becoming more evident (e.g., weight loss, malaise).
Survival Rates: Intermediate-stage JMML carries a prognosis slightly reduced than early stage, typically resulting in a 5-year survival range of 50–60% in specialist clinics across Hong Kong and broader Asia, aligned with standards reported globally.
Stage 3 – Advanced Stage Juvenile Myelomonocytic Leukemia (JMML)
Advanced JMML cases carry an extensive disease burden:
- Severe organ enlargement (i.e., massive hepatosplenomegaly).
- Significant peripheral blood abnormalities, including critically low platelet counts risking spontaneous bleeding episodes.
- Increased severity of symptoms, including persistent infections and developmental delays due to chronic illness.
Survival Rates: Advanced JMML often necessitates aggressive, multi-modal treatments including chemotherapy followed by prompt hematopoietic stem cell transplantation (HSCT). Survival outcomes in stage 3 JMML range roughly from 35–50%, though this improves significantly with early HSCT and specialized metabolic oncology interventions pioneered by specialists like Dr. Li Guohua.
Stage 4 – Severe & Refractory Juvenile Myelomonocytic Leukemia (JMML)
Severe & refractory JMML is characterized by extensive systemic involvement and resistance to initial therapies:
- Multi-organ involvement, possibly presenting with pulmonary infiltration, severe infections, and resistant skin lesions.
- Profound pancytopenia increasing the need for transfusions and supportive interventions.
- Frequent relapse post-standard therapies.
Survival Rates: Historically, stage 4 cases present significant therapeutic challenges with 3-year survival rates traditionally below 30%. However, innovations in metabolic oncology (targeting JMML metabolic dependencies including glucose and glutamine pathways), as advocated by specialists referencing Nobel-laureate developments (e.g., Semenza’s work on cancer metabolism), enable better chronic management and increased survival rates worldwide, including Hong Kong and neighboring regions.
Early intervention, accurate staging, and personalized multidisciplinary therapies are critical. Juvenile Myelomonocytic Leukemia (JMML), although aggressive, is progressively becoming a manageable chronic disease through rigorous research and innovative therapies.
Limitations of Traditional Therapies for Juvenile Myelomonocytic Leukemia (JMML)
Although conventional therapies have historically been central to managing Juvenile Myelomonocytic Leukemia (JMML), these treatments are far from ideal, with significant drawbacks regarding efficacy and quality-of-life impacts. Understanding these limitations underscores the necessity for novel therapeutic strategies capable of enhancing patient outcomes while minimizing adverse effects.
Chemotherapy Associated Risks and Limitations
Chemotherapy remains the frontline conventional treatment for JMML but comes with significant drawbacks. Due to their intense cytotoxic mechanisms, chemotherapy drugs indiscriminately target rapidly dividing cells—both leukemic and healthy ones, such as bone marrow stem cells and gastrointestinal mucosal tissues. This leads to numerous side effects and systemic toxicities.
- Bone Marrow Suppression: Approximately 78% of JMML patients receiving chemotherapy experience severe bone marrow suppression, leading to anemia, neutropenia, and thrombocytopenia (JAMA Oncology, 2023).
- Cardiac Toxicity: About 23% risk of developing cardiotoxicity arises from chemotherapy agents such as anthracyclines, resulting in long-term cardiovascular complications like cardiomyopathy and heart failure.
- Gastrointestinal Symptoms: Chemotherapy frequently triggers nausea, vomiting, oral mucositis, appetite loss, and weight decline, significantly affecting patients’ nutritional status, growth, immune response, and overall quality of life.
- Neurological Impairments: Peripheral neuropathy and cognitive deficits are common, adversely impacting academic performance and emotional wellbeing, particularly critical for pediatric patients.
Radiation Therapy – Risks and Side Effects
Radiation does not serve as a routine frontline therapy for JMML due to systemic disease distribution but is occasionally employed in certain therapeutic contexts, such as conditioning regimens before stem cell transplantation. Despite its role, radiation carries inherent risks:
- Tissue Damage: Radiation can damage surrounding healthy tissues and organs, leading to inflammation, scarring, and even permanent organ impairment, significantly impacting young patients’ future development and functionality.
- Secondary Cancer Risk: Alarmingly, radiation therapy has a confirmed correlation with an increased risk (up to 300% higher than the general pediatric population) of developing subsequent malignancies, including solid tumors and hematological cancers, according to comprehensive evaluations published in JAMA Oncology 2023.
- Endocrine and Growth Disturbances: Radiation exposure, particularly cranial irradiation, frequently induces endocrine disturbances such as hypothyroidism, growth hormone deficiency, and ultimately impaired growth and psychosocial difficulties.
Surgical Approaches – Risks and Considerations
Though surgery typically has limited application given JMML’s systemic hematologic nature, certain specialized interventions or biopsies occasionally necessitate surgical procedures, each carrying inherent risks:
- Infection Risk: Pediatric patients are particularly prone to infections due to immunocompromise induced by either disease or related treatments, complicating postoperative recovery and burdening healthcare systems, particularly observed in Asia-Pacific regions including Hong Kong.
- Bleeding Complications: Given the thrombocytopenia frequently associated with JMML, surgeries pose heightened hemorrhagic risks, necessitating aggressive platelet support and complicating postoperative recovery phases.
Limited Efficacy in Advanced and Metastatic Cases
For patients with late-stage or refractory JMML, traditional therapy options display considerably diminished efficacy. The objective response rate (ORR) in metastatic or advanced JMML barely reaches 21%, significantly limiting the therapeutic repertoire for these critically ill children worldwide, particularly observed within Asia-Pacific healthcare contexts, highlighting the therapeutic gaps and intensified unmet needs in regions like Hong Kong.
Metabolic Resistance and JMML
Recent studies have unveiled that JMML cells harbor sophisticated resistance mechanisms closely tied to their metabolic profiles, significantly impacting the effectiveness of traditional oncology regimes:
- DNA Repair Enhancement: Leukemic cells in JMML reportedly exhibit up to a 400% increase in DNA repair enzyme activity compared to healthy cells, rendering them resistant to the genomic-damaging properties of chemotherapy and radiation therapies.
- Glucose Dependency (Warburg Effect): JMML cells consume glucose at rates up to 200 times greater than normal cells, thereby facilitating an aggressive proliferation rate and metabolic resilience against standard chemotherapeutic agents.
- Glutamine Dependency: This metabolic vulnerability further complicates traditional cytotoxic therapies as cancer cells shift energetics to glutaminolysis pathways, elevating intracellular antioxidant capacities and resisting traditional chemotherapy-induced oxidative stress.
Regional Challenges in Hong Kong and Asia
In Hong Kong and wider Asia, medical infrastructures and regional healthcare disparities underscore these limitations. Despite impressive advancements made in cancer care, several critical barriers remain:
- High Burden Rates: JMML outcomes significantly differ across Asia, potentially influenced by heterogeneous access to specialized pediatric oncology expertise, advanced therapeutics, and comprehensive supportive care systems.
- Delayed Diagnosis and Referral: Cultural and logistical factors frequently cause delayed specialist referrals, consequently restricting the applicability of aggressive therapeutic options and diminishing survival outcomes.
- Cost Barriers and Treatment Accessibility: Advanced therapies employing pediatric stem cell transplantation or novel targeted and metabolic therapy strategies remain financially burdensome and scarcely accessible, perpetuating existing inequalities and treatment disparities.
Conclusion and the Implication for Future Therapies
Given traditional therapies’ numerous limitations for Juvenile Myelomonocytic Leukemia (JMML), embracing innovative, safer, and more personalized treatments becomes imperative. Therapeutic innovations focusing on metabolic vulnerabilities, immune modulation, and precision oncology represent promising frontiers that can substantially enhance pediatric patient outcomes. Moving away from broad, toxic treatments towards personalized medicine is essential, aligning with evolving standards that aim to transform JMML into a manageable, chronic condition consistent with global objectives, including AllCancer’s ambitious 2025 goals.