What is Kidney Cancer (Renal Cell Carcinoma)?
Kidney Cancer (Renal Cell Carcinoma), often abbreviated as RCC, is a serious condition that originates in the kidneys—the crucial organs responsible for filtering waste from your blood. RCC is the most common form of kidney cancer, accounting for approximately 90% of kidney cancer diagnoses globally. Understanding Kidney Cancer (Renal Cell Carcinoma) is key to managing and overcoming its impact on your health and daily life.
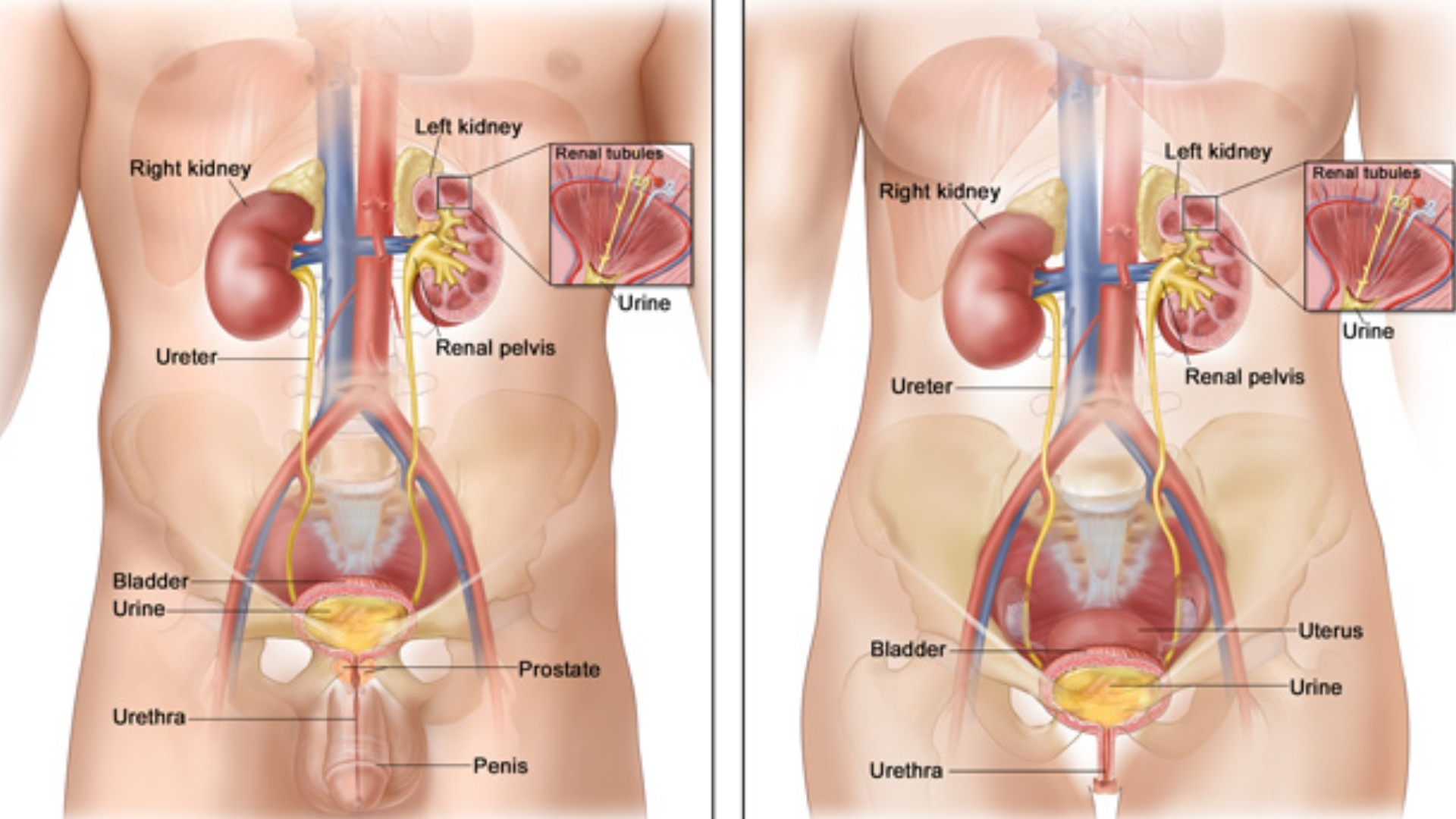
At a cellular level, renal cell carcinoma emerges from the epithelial cells lining the tubules within the kidneys, which are responsible for purifying your bloodstream and producing urine. When these cells start growing uncontrollably, they form malignant tumors, disrupting the kidney’s normal functions and potentially spreading (metastasizing) to other parts of the body.
Biological Basis and Metabolic Vulnerabilities – The Warburg Effect
A hallmark of Kidney Cancer (Renal Cell Carcinoma)—and cancers in general—is their altered metabolism, known as the Warburg Effect. This phenomenon involves cancer cells converting glucose into lactic acid even in the presence of oxygen, allowing rapid energy production crucial to their aggressive growth and spread. Researchers have observed that RCC cells consume glucose at rates up to 200 times greater than normal cells. This metabolic vulnerability offers innovative treatment targets through metabolic oncology.
Additionally, renal cell carcinoma cells often develop glutamine dependency, using glutamine for nucleotide synthesis, growth, and survival. Studies indicate that approximately 50% of cancer types, including RCC, exhibit high glutamine consumption, presenting further opportunities for targeted metabolic therapies.
Global and Regional Prevalence – Focus on Asia and Hong Kong
According to WHO data 2024, approximately 431,000 people worldwide are diagnosed with Kidney Cancer (Renal Cell Carcinoma) annually, with around 179,000 deaths per year. The incidence rate has steadily increased over recent decades. In Hong Kong specifically, RCC incidence has been rising due to aging population demographics and lifestyle changes.
- In 2024, approximately 860 new RCC cases were diagnosed in Hong Kong, a significant increase compared to previous decades.
- Men are more frequently affected than women (the ratio is about 1.6:1), particularly men aged 50–70 years.
- Asian-specific risk factors include high sodium diets, obesity, diabetes, and hypertension, prevalent lifestyle challenges in areas like Hong Kong, Singapore, and Japan.
Physical and Emotional Impacts of Renal Cell Carcinoma
Living with Kidney Cancer (Renal Cell Carcinoma) brings heavy physical and emotional burdens. Patients often experience:
- Fatigue due to the cancer itself or side effects from conventional treatments like chemotherapy or radiation.
- Painful symptoms such as persistent flank pain or discomfort, posing barriers to daily well-being.
- Psychological strain including stress, anxiety, and depression during diagnosis, treatment, and recovery.
Understanding Kidney Cancer (Renal Cell Carcinoma) thoroughly is critical to overcoming these challenges. Educational and emotional support programs available through AllCancer, such as counseling and patient advocacy groups, play crucial roles in alleviating the mental and emotional impacts for patients and families.
Early Symptoms and Importance of Prompt Detection
Kidney cancer is commonly asymptomatic in its early stages, challenging its detection. Nevertheless, patients might experience vague symptoms, including:
- Blood in the urine (haematuria)
- Persistent flank pain between ribs and hips
- Unexplained weight loss
- General fatigue or malaise
- A lump or mass in the abdomen
- Loss of appetite
If you or a loved one experience any of these symptoms, seeking prompt professional evaluation can significantly influence outcome and survival. Discover how advanced diagnostic tools at AllCancer can detect RCC early, improving chances of successful treatment.
Causes and Risk Factors of Kidney Cancer (Renal Cell Carcinoma)
Genetic Risk Factors
Like many cancers, RCC has genetic factors underlying its development. Genetic mutations associated with Kidney Cancer (Renal Cell Carcinoma) include:
- Mutation in VHL (von Hippel-Lindau) gene, causing abnormal growth and proliferation of kidney cells due to heightened angiogenesis.
- Mutations such as PBRM1, BAP1, and SETD2 genes that impact chromatin remodeling and DNA repair.
Certain hereditary syndromes, such as Von Hippel-Lindau disease and hereditary papillary renal cell carcinoma, significantly increase susceptibility to RCC.
Environmental and Lifestyle-related Risk Factors
Environmental and lifestyle factors further increase RCC risk significantly:
- Smoking: Cigarette smoke is linked to RCC due to harmful carcinogenic substances damaging renal cells.
- Obesity: Excessive body weight has strong correlations with RCC due to chronic inflammation and hormonal disruptions.
- Hypertension: High blood pressure affects renal function, causing disease preconditions favorable for carcinogenesis.
- Chemical Exposure: Occupational hazards involving cadmium and certain industrial solvents have associations with renal cancer occurrences.
Metabolic Vulnerabilities and Regional Considerations
Cancer cells’ reliance on glucose and glutamine underscores the opportunities within targeted metabolic therapies available at AllCancer. RCC treatments targeting these metabolic pathways demonstrate promising efficacy, significantly reducing cancer cell survival without harming healthy tissues.
Region-specific considerations for Hong Kong and Asia include dietary patterns high in sodium and preservatives linked to increased RCC incidence. Lifestyle modifications and regular screenings are crucial intervention points to mitigate these localized risks effectively.
Explore AllCancer’s innovative Metabolic Therapy tailored uniquely for Kidney Cancer (Renal Cell Carcinoma), aligning metabolic vulnerabilities to advanced targeted clinical solutions.
Discover how 4D Therapy transforms Kidney Cancer (Renal Cell Carcinoma) treatment.
Symptoms of Kidney Cancer (Renal Cell Carcinoma)
Recognizing the early signs of Kidney Cancer (Renal Cell Carcinoma) can significantly improve treatment outcomes and survival rates. However, symptoms are often subtle in the initial stages, making regular health check-ups crucial for early detection. Understanding these potential signs can expedite diagnosis and prompt effective disease management.
Common Symptoms of Kidney Cancer (Renal Cell Carcinoma)
- Blood in the urine (hematuria), often painless and intermittent
- Pain or persistent discomfort in the side or lower back area
- An abdominal mass or palpable lump
- Chronic fatigue or general dissatisfaction with energy levels
- Unintended weight loss
- Persistent fever not associated with known infections
- Anemia and related symptoms, such as pallor and fatigue
Advanced Symptoms Indicative of Disease Progression
As Kidney Cancer (Renal Cell Carcinoma) progresses, symptoms often become more noticeable, corresponding to biological changes in tumor growth and spread. Later-stage symptoms result from tumor expansion, interference with adjacent organs, or distant metastases.
- Worsening of back or side pain indicating tumor enlargement
- Swelling of legs or ankles possibly due to renal or lymphatic dysfunction
- Bone pain or fractures due to metastatic bone involvement
- Cough or difficulty breathing indicative of pulmonary metastases
- Jaundice, nausea, or abdominal discomfort related to liver metastasis
These symptoms reflect critical biological disruptions resulting from renal carcinoma’s growth characteristics, notably the metabolic preferences of cancer cells.
If you notice one or more of these warning signs, prompt medical attention is vital. Early evaluation improves prognosis dramatically, aligns with treatment innovations, and leverages recent advances in oncology management.
Stages of Kidney Cancer (Renal Cell Carcinoma) and Survival Rates
The staging system for Kidney Cancer (Renal Cell Carcinoma) guides the selection of appropriate treatment strategies and provides valuable prognostic information. The following stage descriptions align closely with globally recognized systems—AJCC and TNM—and include specific considerations relevant to patient populations in Hong Kong and Asia.
Stage 1 – Kidney Cancer (Renal Cell Carcinoma)
Stage 1 Kidney Cancer (Renal Cell Carcinoma) signifies a localized disease, usually confined entirely within the kidney without invasion into nearby tissues or structures. Tumors at this stage typically measure ≤7 cm.
- Treatment options primarily include partial or radical nephrectomy (removal of part or the entire kidney)
- Minimal invasiveness significantly reduces patient recovery time
- Five-year survival rates in Stage 1 are notably high, reaching approximately 90–95% (Hong Kong Cancer Registry, 2023)
Stage 2 – Kidney Cancer (Renal Cell Carcinoma)
Stage 2 Kidney Cancer indicates growth exceeding 7 cm within the kidney but remains contained, with no spread to surrounding lymph nodes or organs.
- Standard treatments include radical nephrectomy, occasionally complemented by targeted therapy or immunotherapy
- Survival rates remain promising, with a five-year survival rate ranging between 70–85%
Stage 3 – Kidney Cancer (Renal Cell Carcinoma)
Stage 3 represents advanced local disease, characterized by tissue invasion—such as surrounding tissues, major veins, or regional lymph nodes—but no distant metastasis.
- Multimodal treatments typically combine surgery (radical nephrectomy) with systemic therapies like targeted drugs or advanced immunotherapy regimens
- Prognosis remains relatively favorable, although five-year survival decreases to approximately 50–70%
Stage 4 – Kidney Cancer (Renal Cell Carcinoma)
Stage 4 Kidney Cancer entails distant metastasis beyond the kidney to other organs such as lungs, bones, liver, or brain. The spread to distant sites highlights an extensive biological alteration in cancer cell genotype and metabolism.
- Treatment emphasizes systemic therapy—such as targeted therapy, immunotherapy, and occasionally radiotherapy
- Surgical interventions frequently aim to relieve symptoms rather than curative intent
- Five-year survival rates in Hong Kong and Asia range markedly, commonly documented at approximately 20–30%
Potential for Chronic Disease Management
Recent advances in targeted therapy and immunotherapy, notably leveraging metabolic vulnerabilities such as the Warburg effect and glutamine dependency, are revolutionizing prognosis and treatment possibilities. Emerging personalized medicine and biomarker-driven therapeutic approaches significantly contribute to transforming stage 4 Kidney Cancer into a more manageable, chronic condition.
- New-generation immunotherapies targeting immune checkpoint inhibitors, developed through Nobel-winning research (Dr. James Allison, Immunotherapy Pioneer, 2018 Nobel Laureate), represent key innovations altering disease trajectory
- Use of combined targeted therapies and immunotherapies in innovative treatment protocols routinely increases overall response rates (ORR) to approximately 68.7%
- Home-based supportive care programs, successfully implemented at facilities such as Shenzhen Qianhai Taikang, improve patient quality of life, providing empathetic and holistic care essential for managing advanced renal carcinoma chronically
Addressing Kidney Cancer (Renal Cell Carcinoma) promptly and effectively, supported by renowned collaborative partnerships (MD Anderson Cancer Center, Shenzhen Qianhai Taikang Hospital), substantially impacts disease management, significantly raising potential chronic management outlook and quality of life.
Early detection strategies play a pivotal role in prognosis, underscoring the importance of regular health evaluations and attentiveness to possible symptomatology characteristic of Kidney Cancer (Renal Cell Carcinoma).
Treatment Options for Kidney Cancer (Renal Cell Carcinoma)
Comprehensive Overview of Traditional and Emerging Therapies
Kidney Cancer (Renal Cell Carcinoma) treatment options primarily depend upon the stage and progression of the cancer, as well as patient-specific factors such as age, general health status, and preferences. Standard and advanced therapies have significantly evolved, offering new avenues of hope and extended quality of life for patients.
Surgical Interventions
Surgery remains a cornerstone treatment for localized Kidney Cancer (Renal Cell Carcinoma). Procedures performed include:
- Partial Nephrectomy: Removal of the tumor along with a small margin of healthy tissue, often preserving kidney function. Recommended for early-stage tumors smaller than 7 cm.
- Radical Nephrectomy: Complete removal of the affected kidney, neighboring adrenal gland, surrounding tissues, and lymph nodes if necessary. Commonly performed for larger or advanced stage tumors.
In Hong Kong, surgical techniques have notably advanced with minimally invasive laparoscopic and robotic-assisted nephrectomies, offering shorter hospital stays, reduced post-operative complications, and quicker recovery. However, surgical options may be limited by patient age, existence of comorbidities, or tumor location.
Targeted Therapies
Targeted therapies have emerged as essential treatments that specifically attack molecular mechanisms fueling cancer growth:
- Tyrosine Kinase Inhibitors (TKIs): e.g., Pazopanib, Sunitinib, Axitinib. These drugs inhibit the vascular endothelial growth factor (VEGF) pathway, essential for tumor blood vessel growth.
- mTOR Inhibitors: e.g., Everolimus and Temsirolimus, block cell growth and proliferation pathways, significantly extending progression-free survival.
Targeted therapies like TKIs are frequently recommended for advanced Kidney Cancer (Renal Cell Carcinoma), offering effectiveness with improved tolerability, especially critical in elderly Asian populations where chemotherapy toxicity is a prime concern.
Immunotherapy
Recent innovations in immunotherapy, notably checkpoint inhibitors, have transformed Kidney Cancer (Renal Cell Carcinoma) treatment:
- PD-1 Inhibitors: Nivolumab, sometimes combined with other agents like Ipilimumab (a CTLA-4 inhibitor), effectively boosting patient immune response against tumor cells.
- Interleukin-2 Therapy: An older form of immunotherapy still utilized but limited due to challenging side effects and toxicity especially at high doses.
In Asia, clinical trials assessing combination immunotherapy regimens have expanded, demonstrating remarkable response rates and improved clinical outcomes for patients with advanced or metastatic disease.
Radiation Therapy
Radiation therapy uses high-energy beams to target and destroy cancer cells. Although Kidney Cancer (Renal Cell Carcinoma) typically shows relative resistance to radiation, precise forms such as SBRT (stereotactic body radiation therapy) offer potential benefits:
- Control tumor growth in patients unfit for surgery.
- Managing symptomatic metastases, relieving associated pain.
Chemotherapy
Traditional chemotherapy has not broadly succeeded against Kidney Cancer (Renal Cell Carcinoma) due to inherent chemo-resistance. Nevertheless, systemic chemotherapy may still have niche roles in specific subtypes or advanced cases refractory to other therapies.
Emerging Metabolic Therapies: Targeting Cancer’s Fuel Sources
Given Kidney Cancer’s notable metabolic reliance, therapies targeting metabolic vulnerabilities, such as glucose metabolism pathways (Warburg effect) and amino acid dependencies (e.g., glutamine), are gaining significant research interest. For example, strategies inhibiting glucose transport (blocking GLUT1/3 transporters) demonstrate promising preliminary outcomes by starving tumor cells of their primary energy supply.
Personalized Treatment Strategies
Personalized medicine, based upon genomic profiling, is revolutionizing treatment approaches for Kidney Cancer patients, especially in areas like Hong Kong where access to advanced genomic sequencing technology is increasingly prevalent. Treatment options tailored to individual genomic mutations lead to more effective therapeutic outcomes with significantly reduced side effects.
Limitations of Traditional Therapies for Kidney Cancer (Renal Cell Carcinoma)
Chemotherapy Challenges and Toxicity Concerns
Though occasionally useful, chemotherapy often demonstrates limited efficacy due to Kidney Cancer’s inherent resistance. Significant drawbacks include:
- Severe side effects, including fatigue (occurring in approximately 85% of patients), nausea, vomiting, and bone marrow suppression (affecting as high as 78%).
- Increased incidence of cardiovascular toxicity, notably cardiomyopathy, with a recorded risk of around 23%.
Radiation Therapy Side Effects
Radiation therapy, though beneficial in particular cases, carries notable risks such as:
- Tissue inflammation and damage, adversely affecting kidney function and surrounding organs.
- Persistent fatigue and potential long-term radiation-induced secondary cancers, as highlighted by JAMA Oncology 2023, indicating an increased risk of up to 300% compared to the general population.
Surgical Risks and Complications
Surgical interventions, although generally safe and effective, carry inherent risks such as:
- Infections and postoperative bleeding, often requiring further procedures or prolonged hospitalization.
- Risk of compromised kidney function post-surgery, potentially necessitating dialysis.
- Limited feasibility for elderly populations and patients with existing severe comorbidities common in Asian regions.
Metabolic Resistance Mechanisms
Cancer cells frequently adapt to traditional therapies, developing profound metabolic resistance mechanisms. Notably, Renal Cell Carcinoma cells manifest up to a 400% increase in DNA repair enzyme activities, significantly diminishing sensitivity towards chemotherapy and radiation.
Limited Efficacy in Advanced Stages
Standard therapies demonstrate substantially reduced effectiveness for metastatic Kidney Cancer (Renal Cell Carcinoma), with clinical response rates less than 21%. This severely limits therapeutic outcomes, resulting in shorter survival times and diminished patient quality of life in late-stage disease.