What is Nasopharyngeal Cancer (Nasopharyngeal Carcinoma)?
Nasopharyngeal Cancer (Nasopharyngeal Carcinoma), also abbreviated as NPC, is a malignant tumour originating in the epithelial lining of the nasopharynx — the upper part of the throat located behind the nose. Unlike common head and neck cancers, NPC is relatively uncommon worldwide yet disproportionately prevalent in Southeast Asia, particularly Hong Kong, mainland China, and neighbouring populations in Asia.
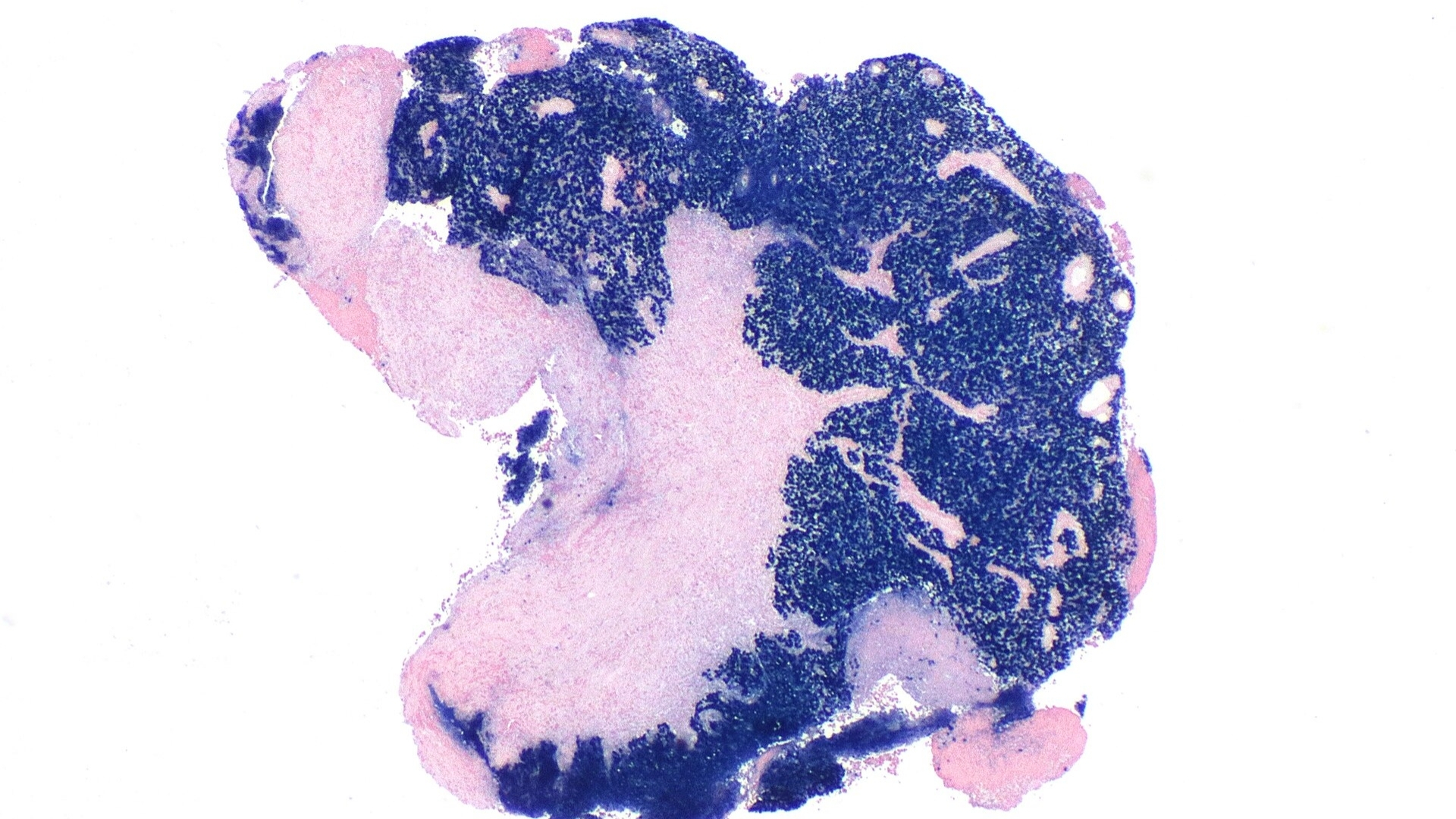
Biological Basis of Nasopharyngeal Cancer (Nasopharyngeal Carcinoma)
Understanding Nasopharyngeal Cancer (Nasopharyngeal Carcinoma) requires insight into its biological mechanisms. At a cellular level, NPC originates through malignant transformation and uncontrolled proliferation of the nasopharyngeal epithelium cells. Unique among cancers, NPC shows an extremely high correlation to infection with Epstein-Barr virus (EBV), significantly influencing tumour progression and malignant potential.
Nasopharyngeal Cancer (Nasopharyngeal Carcinoma) cells exhibit unique metabolic traits such as the Warburg effect, a profound metabolic adaptation. According to Nobel laureate Dr. Gregg Semenza’s pioneering work, cancer cells extensively consume glucose, approximately 200 times the rate of normal cells, opting for anaerobic glycolysis even in oxygen-rich conditions. This rapid glucose metabolism leads to a highly glycolytic and acidic microenvironment, facilitating tumour growth and immune evasion.
- Nasopharyngeal Cancer (Nasopharyngeal Carcinoma) involves rapid and abnormal cell proliferation, often facilitated by viral genetic interference via EBV infection pathways.
- Cancer cells depend heavily on glucose (Warburg effect) and glutamine metabolism, a crucial vulnerability exploited by modern metabolic therapies.
- Recognition of these critical metabolic adaptations provides a foundation for innovative treatments such as Metabolic Oncology practices.
Prevalence and Population Data Specific to Hong Kong and Asia
In Hong Kong and surrounding Asian regions, Nasopharyngeal Cancer (Nasopharyngeal Carcinoma) ranks worryingly high. For example, epidemiological evidence from the Hong Kong Cancer Registry 2024 indicates NPC as the sixth most frequent cancer in local males, with age-standardized incidence rates significantly elevated compared to Western countries. Approximately 80-90% of global NPC diagnoses occur in South China, Hong Kong, Taiwan, and Southeast Asian populations, reinforcing a strong geographic clustering and genetic susceptibility.
Physical and Emotional Impact of Nasopharyngeal Cancer (Nasopharyngeal Carcinoma)
Patients diagnosed with Nasopharyngeal Cancer (Nasopharyngeal Carcinoma) may experience distressing physical symptoms, notably:
- Nasal congestion, bleeding, and obstruction
- Swelling of the lymph nodes in the neck
- Hearing loss or tinnitus due to tumour involvement near Eustachian tubes
- Headaches, facial numbness, or neurological symptoms as tumour involves cranial nerves
- Profound fatigue and weight loss
Emotionally, the diagnosis of Nasopharyngeal Cancer (Nasopharyngeal Carcinoma) can significantly impact psychological well-being, inducing anxiety, fear, and depression. Understanding these burdens underlines the necessity of compassionate care delivery, mental health services, and patient support systems advocated by regional healthcare leaders, including collaborations such as the partnership between AllCancer and Shenzhen Qianhai Taikang.
At AllCancer, we believe accurate education and accessible information form crucial aspects of comprehensive treatment plans. Explore the foundation of cancer biology at AllCancer educational platform.
Causes and Risk Factors of Nasopharyngeal Cancer (Nasopharyngeal Carcinoma)
Nasopharyngeal Cancer (Nasopharyngeal Carcinoma) develops from complex interactions between genetic, environmental, lifestyle, and infectious factors. Recognizing these risk determinants significantly enhances strategic preventive methods, primarily through early diagnostic screening and targeted health awareness campaigns.
Genetic and Familial Risk Factors
- Genetic predisposition highly influences Nasopharyngeal Cancer (Nasopharyngeal Carcinoma), with familial clustering pointing to hereditary susceptibility. Polymorphisms in genes such as HLA (human leukocyte antigen) significantly elevate NPC risk, especially among Chinese populations.
- Alterations in p16, Cyclin D1, and other tumour suppressor genes have demonstrated increased NPC risks in several Asian genetic studies.
Infectious and Environmental Risk Factors
Environmental influences strongly correlate with elevated incidence rates among certain populations.
- Strong association with Epstein-Barr Virus (EBV) infection persists, nearly universal in biopsy analyses from Asian NPC populations.
- Exposure to carcinogens, such as nitrosamine-rich preserved or salted foods heavily consumed in Southern China and Hong Kong, significantly increases cancer risks.
- Exposure to chronic second-hand cigarette smoke is linked to doubled NPC incidence rates across several longitudinal studies.
Lifestyle-Related Risk Factors
- Regular consumption of high-nitrate, salted, or fermented foods prevalent in Hong Kong and surrounding regions correlates heavily with increased NPC risks.
- Excessive alcohol intake indirectly contributes by decreasing immune resistance, potentially impacting EBV reactivation and carcinogenesis.
Metabolic Vulnerabilities and Therapeutic Potential
Research spearheaded by metabolic oncology pioneer Dr. Li Guohua indicates vulnerabilities such as NPC cell dependency on augmented glutamine metabolism pathways. Approximately 50% of NPC cells use glutamine explicitly for nucleotide production, creating therapeutic targets significantly explored within targeted metabolic treatments such as AllCancer’s innovative 4D Therapy.
Maintaining high vigilance for early NPC detections remains essential, with prompt diagnosis critically improving therapeutic outcome probability. Discover comprehensive diagnostic procedures for early cancer detection at AllCancer.
Symptoms of Nasopharyngeal Cancer (Nasopharyngeal Carcinoma)
Recognizing symptoms early is vital in achieving favorable outcomes for individuals with Nasopharyngeal Cancer (Nasopharyngeal Carcinoma). Here, we detail prevalent indicators and explain their biological underpinnings to enhance understanding and promote early intervention.
Common Nasopharyngeal Cancer (Nasopharyngeal Carcinoma) Symptoms Include:
- Persistent nasal congestion or obstruction, typically unilateral.
- Frequent nosebleeds (epistaxis), reflecting tumor invasion into blood vessels.
- Lumps or swellings in the neck due to lymph node involvement.
- Tinnitus or ringing sensation in the ears, sometimes associated with unilateral hearing impairment.
- Headache or facial pain, resulting from local infiltration and pressure on cranial nerves.
- Diplopia (double vision) or visual abnormalities indicating tumor effect on surrounding cranial structures.
- Persistent ear infections or middle ear fluid accumulation (otitis media with effusion).
- Weight loss, fatigue, or general malaise owing to systemic inflammatory response by advanced tumor activity.
Symptom Variations by Stage:
- Early Stage (Stage 1-2): Often subtle, including mild nasal blockage, intermittent nosebleeds, or painless lymph node enlargement.
- Advanced Stage (Stage 3-4): More aggressive symptoms emerge, including progressive facial pain, extensive lymph node swelling, significant hearing loss, cranial nerve palsies, and deeper infiltration symptoms such as difficulty swallowing or significant weight loss.
Recognizing Nasopharyngeal Cancer (Nasopharyngeal Carcinoma) at an early stage drastically increases treatment success, improving overall survival rates from approximately 50-70% in late diagnosis stages to above 90% with prompt detection and intervention. Hence, immediate medical evaluation when symptoms arise greatly increases achievable outcomes.
Learn more about diagnostic protocols for Nasopharyngeal Cancer (Nasopharyngeal Carcinoma).
Stages of Nasopharyngeal Cancer (Nasopharyngeal Carcinoma) and Survival Rates
Staging helps oncologists and affected individuals understand prognosis, plan treatment approaches effectively, and guides expectations regarding survival outcomes. Here we provide an overview of each stage, correlating it with treatment strategies and corresponding survival expectations based on data specific to Hong Kong and broader Asia.
Stage 1 Nasopharyngeal Cancer (Nasopharyngeal Carcinoma)
At this early stage, cancer cells remain confined within the nasopharynx. Importantly, tumors during this stage often measure less than 2 centimeters and display no major lymphatic or systemic spread.
- Treatment Options: Primarily radiotherapy; tailored chemotherapy to enhance radiosensitivity is sometimes adopted.
- Five-year survival rate: Approximately 90–95%, emphasizing the significance of early detection and timely treatments.
Stage 2 Nasopharyngeal Cancer (Nasopharyngeal Carcinoma)
Stage 2 represents localized tumor growth, with possible involvement of nearby lymph nodes within the neck (unilateral lymph node involvement typically under 3 cm).
- Treatment Approach: Combination therapy including radiotherapy and chemotherapy, aimed towards eradication of local tumor and involved regional lymphatic systems.
- Five-year survival rate: Between 75–85%, contingent upon comprehensive multidisciplinary treatment.
Stage 3 Nasopharyngeal Cancer (Nasopharyngeal Carcinoma)
With advanced local tumor involvement and metastasis to bilateral or extensive cervical lymph nodes, stage 3 requires aggressive therapy for successful outcome management.
- Treatment Modalities: Multimodal therapies integrating chemotherapy, targeted radiation modalities such as intensity-modulated radiation therapy (IMRT), and biological or metabolic therapy approaches showing promising clinical results.
- Five-year survival rate: From around 60–70%, still a manageable number when treated aggressively, highlighting significant therapeutic advances.
Stage 4 Nasopharyngeal Cancer (Nasopharyngeal Carcinoma)
Stage 4 reveals tumor metastasis beyond regional lymphatic tissues, involving distant organs including the lungs, bones, and liver, requiring systemic therapeutic interventions.
- Challenges in Management: Systemic metastasis demands sophisticated therapeutic approaches such as advanced chemotherapy protocols, targeted therapies including immune checkpoint inhibitors, metabolic interventions harnessing cancer cell vulnerabilities like the Warburg effect and glutamine dependency, and personalized medicine approaches tailored to genetic tumor profiling.
- Survival Rates: Despite the aggressiveness, survival has significantly improved with implementation of metabolic approaches and targeted immunotherapy. Three-year survival for metastatic stage approximates 20–35% cases, but innovations from leading institutions like MD Anderson, Shenzhen Qianhai Taikang, and regional collaborations enhance individual outcomes.
Ongoing oncological research spearheaded by experts such as Dr. Li Guohua and Prof. Liu Guolong and breakthroughs in metabolic oncology may soon elevate Nasopharyngeal Cancer into a chronically manageable disease. Hence, even stage 4 diagnoses carry reasons for guarded optimism, especially with AllCancer’s groundbreaking research aiming to increase chronic management capabilities by 2025.
Treatment Options for Nasopharyngeal Cancer (Nasopharyngeal Carcinoma)
Treatment for Nasopharyngeal Cancer (Nasopharyngeal Carcinoma) has significantly evolved in recent years. Personalized medical approaches tailored specifically to each patient’s genetic and molecular profile improve outcomes, especially in Asia and Hong Kong, regions with notably higher incidence rates.
Radiation Therapy
Radiation therapy remains a primary consideration for most cases of Nasopharyngeal Cancer (Nasopharyngeal Carcinoma). Modern techniques have dramatically improved precision:
- Intensity-Modulated Radiation Therapy (IMRT) allows for focused radiation beams, minimizing damage to adjacent tissues, and ensuring maximal tumor destruction.
- Proton Therapy represents newer technology beneficial in limiting radiation exposure to healthy tissues—especially critical for treating tumors near sensitive structures (e.g., brainstem, cranial nerves).
- Brachytherapy is occasionally employed for localized recurrent disease, delivering radiation directly inside the tumor.
Chemotherapy
Chemotherapy plays a complementary role in treating advanced stages of Nasopharyngeal Cancer (Nasopharyngeal Carcinoma), particularly when there is extensive regional or distant disease spread:
- The standard regimens include platinum-based chemotherapies (cisplatin or carboplatin), often combined with 5-fluorouracil (5-FU).
- Induction chemotherapy may also be given before radiotherapy to reduce tumor size and metastatic risk, with documented enhanced survival as presented in recent trials from Hong Kong universities.
Surgical Interventions
Surgery typically has a limited role in treating Nasopharyngeal Cancer (Nasopharyngeal Carcinoma) due to anatomical constraints. However, in certain situations, surgical intervention remains indispensable:
- Neck Dissection is employed for recurrent or persistent lymph node involvement after radiotherapy.
- Endoscopic Nasopharyngectomy offers valuable solutions for small recurrent lesions after primary nonsurgical therapies.
Targeted Therapies
Scientific advancements have facilitated targeted therapies effectively counteracting specific molecular and genetic alterations characteristic in Nasopharyngeal Cancer (Nasopharyngeal Carcinoma):
- EGFR Inhibitors, such as cetuximab, have shown significant promise when used alongside radiation and chemotherapy.
- Vascular Endothelial Growth Factor (VEGF) Inhibitors like bevacizumab are being extensively researched for metastatic disease control.
Metabolic Therapies: A Promising Frontier
Cutting-edge studies are increasingly revealing the metabolic vulnerabilities of cancer cells associated with glucose and glutamine metabolism. Therapies targeting these pathways exploit such vulnerabilities, contributing to the advancement of treatment for resistant and recurrent Nasopharyngeal Carcinoma:
- Blocking glucose transporters (GLUT1/3) to starve cancer cells is a promising therapeutic approach. Clinical trials involving metabolic therapies demonstrate impressive outcomes, significantly extending periods of remission and lowering recurrence rates.
- Glutamine inhibitors are showing promising preliminary efficacy against aggressive carcinomas resistant to conventional therapies.
Personalized Treatment Plans for Nasopharyngeal Cancer (Nasopharyngeal Carcinoma)
Due to genetic diversity and varied pathologic behavior, personalized medicine greatly enhances treatment efficacy. By integrating genomic profiling, physicians increasingly individualize therapeutic strategies, optimizing supportive care, minimizing toxicities, and maximizing treatment benefits.
Limitations of Traditional Therapies for Nasopharyngeal Cancer (Nasopharyngeal Carcinoma)
Despite therapeutic advancements, traditional treatments for Nasopharyngeal Cancer (Nasopharyngeal Carcinoma), such as chemotherapy, radiation, and surgery, pose significant limitations, often severely impacting patient quality of life.
Toxicity and Side Effects of Chemotherapy
Platinum-based chemotherapy, mainstays of Nasopharyngeal Cancer management, are deeply associated with adverse effects:
- Bone marrow suppression occurs in approximately 78% of patients, often requiring dose reductions or discontinuation, compromising treatment effectiveness.
- Cardiac toxicities—reported in 23% of patients—pose substantial cardiac risks, notably limiting therapeutic dose intensity and duration.
- Patients frequently experience severe nausea, vomiting, peripheral neuropathy, kidney damage, hearing loss, and profound fatigue, substantially affecting overall patient well-being and compliance.
Radiation Therapy Limitations
Radiation, although targeted, can still inflict significant collateral damage on healthy tissues adjacent to the nasopharynx:
- Salivary gland damage and resultant chronic dryness (xerostomia).
- Swallowing difficulty (dysphagia), taste impairment, and mucositis can profoundly lower nutrition and life quality.
- Radiation-induced fibrosis and tissue necrosis exacerbate long-term morbidity in a large share of patients.
- Secondary cancers due to DNA damage, according to publications like JAMA Oncology (2023), increase risks up to 300% above baseline risk.
Surgical Risks
Surgical procedures, though infrequent, possess associated inherent risks:
- Potential infection, nerve injuries, and scarring impact patient’s postoperative recovery and long-term function.
- Risks of bleeding, particularly due to proximity to critical blood vessels and nerves, challenge surgical feasibility and success.
Minimal Efficacy in Late-stage Cases
Traditional treatments have relatively low curative potential at advanced or metastatic stages. Studies estimate the objective response rate (ORR) decreasing significantly below 21%, underscoring limited effectiveness and urging accelerated research and transition to novel therapeutic models.
Metabolic Resistance Mechanisms
A distinct limitation arises from metabolic resilience acquired by carcinoma cells. They often exhibit a 400% rise in DNA repair enzyme activities, greatly diminishing chemotherapy efficacy, exacerbating cancer persistence, and poor therapeutic outcomes.