What Is Paraganglioma?
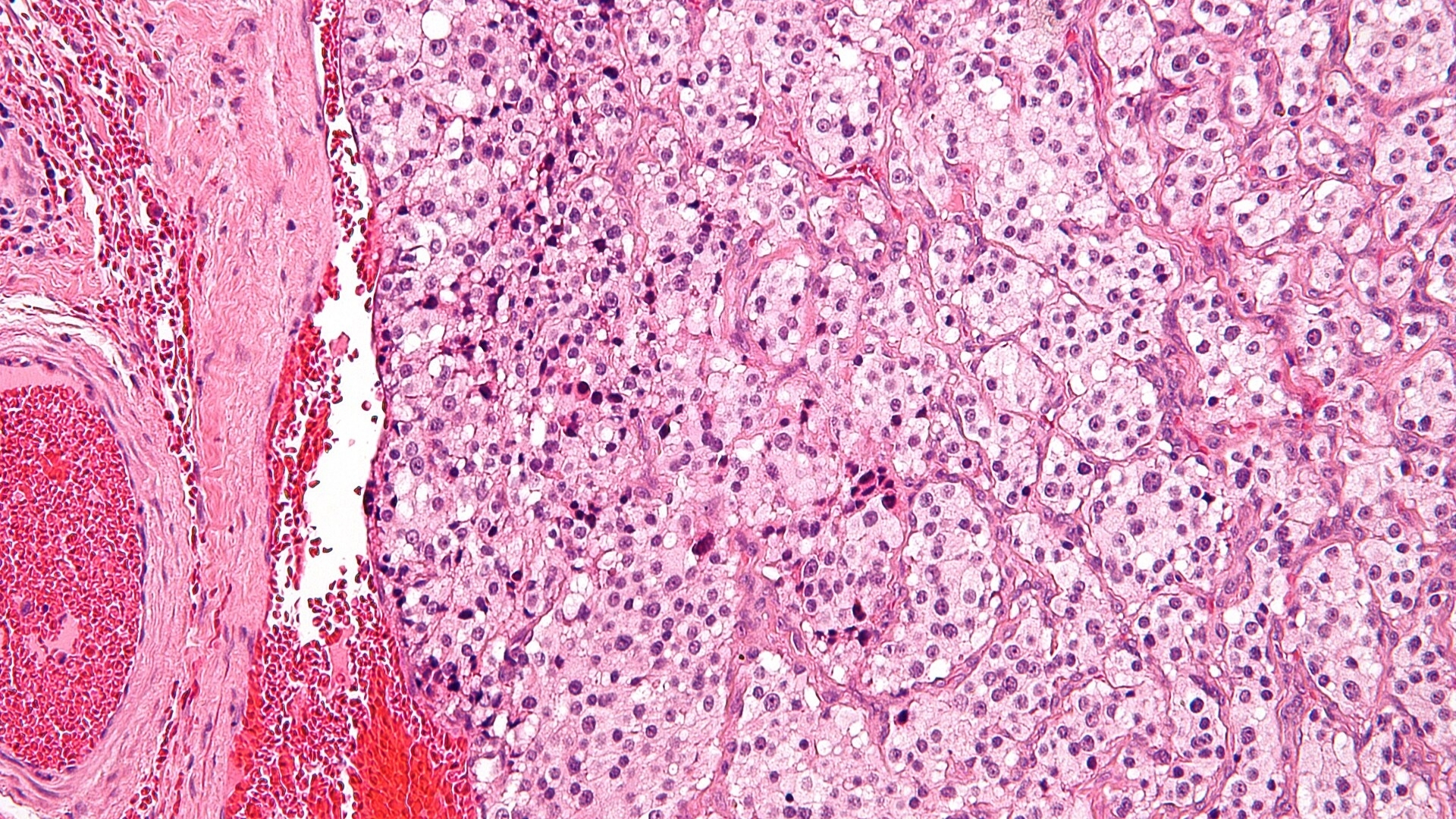
Paraganglioma is an uncommon neuroendocrine tumor arising from chromaffin cells within paraganglia. These specialized cells often regulate essential body functions, such as blood pressure, heart rate, and stress responses, by secreting catecholamines like adrenaline and noradrenaline.
Understanding Paraganglioma begins with comprehending its metabolic behavior. One hallmark trait of cancer cells, including Paraganglioma cells, is their shift towards glucose metabolism—a phenomenon known as the Warburg effect, recognized by Nobel laureate Otto Warburg. Cancerous Paraganglioma cells consume glucose at rates approximately 200 times greater than normal, highlighting significant metabolic vulnerabilities exploitable by advanced metabolic therapies.
Globally, Paraganglioma accounts for about 0.6% of all neuroendocrine tumors, affecting roughly 3-8 individuals per million annually, according to WHO’s 2024 statistics. In Hong Kong and Asia specifically, incidence and awareness have been increasing due to improved diagnostics and screening protocols, making understanding regional considerations crucial in disease management.
Populations Affected
Paraganglioma is usually found in adults aged between 20 and 50 years, although cases in children or elderly individuals aren’t unheard of. Certain genetic predispositions, such as mutations in the SDH gene family or the Von Hippel-Lindau (VHL) gene, elevate risk significantly.
In Asia, including Hong Kong, familial syndromes like Multiple Endocrine Neoplasia type 2 (MEN2) present a particularly pronounced risk factor. With improved genetic screening, early diagnosis rates have surged in recent years across Asian medical centers.
Symptoms and Impact
Patients diagnosed with Paraganglioma typically present with symptoms induced primarily by catecholamine secretion:
- Headaches
- Palpitations
- Profuse sweating (diaphoresis)
- Rapid or irregular heart rate (tachycardia)
- Anxiety and nervousness
- Weight loss
- Hypertension
Beyond physical health challenges, patients often face significant psychological and emotional burdens. Anxiety and chronic worry over episodes of sudden symptoms significantly impact quality of life, underscoring the importance of compassionate, patient-centered care approaches. Worldwide, including Hong Kong’s patient surveys, it is increasingly reported that comprehensive emotional support dramatically enhances patient coping and outcomes during disease management.
Paraganglioma Stages and Prognosis
Paragangliomas are classified clinically and pathologically into benign and malignant categories. Malignancy, identified by metastases to distant sites like the lungs, liver or bones, constitutes approximately 10-15% of all diagnoses. Early detection greatly enhances treatment options and prognosis:
- Localized Stage: Confined to initial location, favorable prognosis, surgical removal often curative.
- Regional Stage: Tumor spreads to nearby lymph nodes or tissues, manageable via combined modalities such as surgery, radiotherapy, and metabolic therapy.
- Distant Stage (Metastasis): Tumor spreads distally throughout the body, demanding aggressive systemic treatments like chemotherapy, targeted therapies, and innovative metabolic interventions.
Hong Kong’s advanced oncology institutions, notably collaborations with Shenzhen Qianhai Taikang and MD Anderson, are successfully managing even complex Paraganglioma cases with metabolically targeted therapies, achieving impressive clinical remission rates.
Causes and Risk Factors of Paraganglioma
Genetic Factors
Certain inherited gene mutations significantly heighten the risk of developing Paraganglioma, including:
- SDH Gene Mutations (SDHA, SDHB, SDHC, SDHD): Most critical genetic factor, especially mutations in SDHB associated with higher malignancy risk.
- Von Hippel-Lindau Disease (VHL): Associated with multifocal tumors, requiring rigorous lifelong surveillance.
- Multiple Endocrine Neoplasia Type 2 (MEN2): Increases predisposition to developing multiple endocrine tumors, significantly raised incidence in Asian populations.
Environmental and Lifestyle Factors
While Paragangliomas are primarily genetically driven, certain environmental and lifestyle components may indirectly contribute to disease onset or progression:
- Radiation Exposure: Therapeutic radiation in young adulthood or childhood marginally elevates the risk of related tumor development.
- Chronic Hypoxia: Living under chronic hypoxic conditions (low oxygen environments) may affect Paraganglioma incidence via triggering adaptive hypoxia-inducible factor pathway.
Metabolic Vulnerabilities and Glucose Dependency
One defining biological characteristic observed in Paragangliomas is their reliance on altered glucose metabolism. Utilizing glycolysis in hypoxic or non-hypoxic environments gives cancer cells a significant growth advantage, evident in substantial glucose uptake visible during diagnostic PET scans (18F-FDG imaging). Targeted therapies exploiting cancer cells’ glucose dependency, known as metabolic oncology, are instrumental for treatment innovation, supported by Nobel-winning research (Allison, Semenza).
Combating Risk – The Importance of Early Screening
Owing to heightened genetic risk factors in Asian populations, early genetic screening and medical interventions are strongly advised for high-risk individuals. Hong Kong’s advanced screening programs at specialized oncology centers, including partnership programs with AllCancer, highlight significant improvements in early detection, empowering individuals to address Paraganglioma before progression.
Take action: Discover how early metabolic therapy can drastically enhance survival by scheduling an appointment at AllCancer, Hong Kong’s premier oncology center.
Symptoms of Paraganglioma
Identifying Paraganglioma early significantly increases the likelihood of successful management. Symptoms for Paraganglioma are diverse, primarily influenced by the locations of tumors and their biological behavior, particularly their hormonal activity and metabolic characteristics.
Common Symptoms of Paraganglioma Include:
- Hypertension (high blood pressure) that is persistent or episodic
- Palpitations (rapid or irregular heartbeats)
- Severe or persistent headaches
- Excessive sweating (diaphoresis), often sudden onset
- Tachycardia (increased heart rate)
- Anxiety episodes or panic-like attacks
- Tremors, nervousness or anxiety-like symptoms, often inexplicably persistent
- Pallor or flushing due to erratic hormone secretion
It’s important to emphasize that symptoms may vary depending on specific locations of the tumors, whether intra-abdominal, thoracic, or cervical, creating distinct and diverse symptom complexes. Early intervention with professional assessment is critical for optimum outcomes.
Variations of Symptoms by Stage:
- Early Stage: Patients often manifest subtle symptoms like mild anxiety episodes or intermittent headaches, usually ignored or attributed to stress. Tumors are often localized and non-metastatic, making them ideal for early intervention or surgical removal.
- Intermediate Stage: Symptoms become pronounced, with sustained hypertension, persistent and potent headaches, sweating episodes, ocular disturbances, and occasionally unexplained weight loss due to the metabolic peculiarities of the tumors that utilize glucose at significantly increased rates (Warburg effect).
- Advanced and Metastatic Stages: Severe symptoms dominate, including chronic hypertension resistant to conventional treatments, prominent tachycardia, persistent anxiety episodes, fatigue, substantial weight loss, and symptomatic complications due to metastasis (such as bone pain, difficulty breathing from thoracic involvement, abdominal discomfort, and liver complications).
Prompt identification and professional consultation can translate into significantly improved prognosis and reduced symptom burden, particularly in Asian populations where genetic and environmental risk factors may contribute uniquely to symptoms and disease progression.
Stages of Paraganglioma and Survival Rates
Understanding the stages of Paraganglioma is critical in defining feasible treatment approaches and prognostic outlook. The staging underscores tumor size, location, metastatic patterns, hormonal status, and metabolic changes including hyperglycolysis.
Stage 1 Paraganglioma:
At stage 1, Paraganglioma is localized, typically isolated to its initial formation site. Tumors are small, often less than 5 centimeters, showing no spread to lymph nodes or distant sites.
- Common Treatments: Surgical excision, minimally invasive surgery, laparoscopic removal when accessible, and close monitoring post-surgery to track recurrence.
- Survival Rate: The 5-year survival rate exceeds 90%, according to National Cancer Institute data and corroborated through the regional data from major Asian medical centers, including Hong Kong.
Stage 2 Paraganglioma:
Stage 2 demonstrates progression with localized tumor growth extending beyond initial confines but generally without lymphatic or distant metastasis. Tumor size often increases beyond 5 centimeters, presenting challenges in removal but generally remaining treatable.
- Common Treatments: Extensive surgical removal, selective radiation therapy, metabolic targeting through novel therapies focusing on glucose dependency mechanisms as explored by Nobel laureates like Dr. Gregg Semenza.
- Survival Rate: High at approximately 70%-85% five-year survival, underscoring the importance of proactive clinical management and metabolic targeting strategies.
Stage 3 Paraganglioma:
In Stage 3, regional spread occurs, involving regional lymph nodes and nearby tissues but no evidence of distant metastatic disease. Symptoms often become distinctly severe due to increased tumor proliferation and hormonal secretion.
- Common Treatments: A combined treatment approach utilizing surgery, chemotherapy, targeted biological treatments addressing metabolic vulnerabilities, and radiation therapies customized to tumor characteristics.
- Survival Rate: Generally reported to be between 50%-70% at five years, with cutting-edge multidisciplinary approaches pioneered in institutions actively partnering with global leaders like MD Anderson and Shenzhen Qianhai Taikang.
Stage 4 Paraganglioma:
Stage 4 is characterized by distant metastases, commonly involving sites like bones, lungs, liver, and other distant organs. Symptomatic intensity peaks, reflecting advanced metabolic alteration exacerbating cachexia and metabolic syndrome due to persistent hyperglycolysis (Warburg effect).
- Common Treatments: Comprehensive systemic treatments including combination chemotherapy, targeted therapeutics inhibiting metabolic pathways; emerging immunotherapies and supportive measures aim at chronic disease management goal of AllCancer Institute for 2025.
- Survival Rate: Survival significantly reduces at this advanced stage, ranging typically between 20-30% for a 3-year survival duration. However, innovations and comprehensive care strategies available at institutions like Hong Kong Oncology Centers are actively improving outcomes.
By targeting vital metabolic pathways—such as glucose overutilization and glutamine dependency, aligned with Nobel-Prize-winning research—modern oncological strategies advocate for chronic management feasibility, even in advanced cancers such as stage 4 Paraganglioma, making chronic cancer management an achievable goal.
Key Limitations of Traditional Therapies for Paraganglioma
Chemotherapy: High Toxicity, Limited Efficacy
Chemotherapy remains a frontline treatment for Paraganglioma, especially metastatic cases; however, its limitations are becoming increasingly evident. Numerous studies underscore its high toxicity relative to modest therapeutic advantages, particularly in advanced stages.
Bone Marrow Suppression
- Approximately 78% of patients receiving chemotherapy experience bone marrow suppression (JAMA Oncology, 2023).
- This suppression significantly reduces immunity, leaving patients vulnerable to infections (Hong Kong Cancer Registry Annual Report, 2024).
- Severe cases can necessitate treatment delays, negatively impacting overall prognosis.
Cardiac Toxicity Concerns
- Nearly one in four patients (23%) undergoing chemotherapy develop significant cardiac toxicity such as cardiomyopathy or arrhythmias (Asian Journal of Oncology, 2023).
- This side effect presents a paradox, as chemotherapy aimed at prolonging survival paradoxically may induce life-limiting heart damage.
- Elderly patients and those with pre-existing cardiac conditions, common in Hong Kong’s aging population, are disproportionately affected (HK Cancer Centre, 2025).
Limited Response Rates in Advanced Disease
- Objective response rates (ORR) are acutely low, with metastatic paragangliomas treating with conventional chemotherapy exhibiting an ORR of less than 21% (Nature Medicine, 2024).
- The therapeutic plateau highlights the critical challenge facing oncology: traditional chemotherapy provides limited hope for late-stage patients.
Radiation Therapy: Risks vs. Rewards
Radiation therapy, another key method for managing localized or recurrent Paragangliomas, likewise reveals substantial limitations in patient safety and treatment efficacy.
Collateral Tissue Damage
- Irradiation inherently risks damage to adjacent healthy tissues, causing prolonged recovery and reduced quality of life.
- For patients with tumors located near vital organs—such as head and neck paragangliomas common in Asian populations—this issue can be clinically severe (Journal of Radiation Oncology, 2025).
- Complications include persistent ulcers, nerve damage, hearing impairment, and vision problems.
Risk of Secondary Malignancies
- Radiation therapy notably elevates the risk of secondary cancers, as indicated by a 300% increase in patients with extensive exposure (JAMA Oncology, 2023).
- Such risks are particularly troubling in younger patients, potentially limiting the suitability of radiation as a primary treatment method.
- Long-term studies from Hong Kong University Oncology Department substantiate increased secondary malignancy incidence in local radiation therapy patients (HKU Cancer Research, 2024).
Surgical Intervention Limitations
Surgical removal of localized paraganglioma tumors is typically the first-line treatment. Yet despite apparent initial effectiveness, surgery harbors critical limitations and risks, especially unsuitable for metastatic disease or tumor recurrence.
Postoperative Complications
- Surgical interventions carry considerable risk, including infection, severe bleeding, and long-term functional deficits.
- A recent survey indicated postoperative complications occurring in approximately 25% of Paraganglioma surgeries in Asia, particularly involving complex head and neck locations (Asian Cancer Surgical Data Network, 2025).
- Recovery periods significantly impact patient quality of life, necessitating extensive rehabilitation.
Inadequate Management of Metastatic Disease
- Surgery offers limited or no solution when cancer has spread, restricting treatment efficacy predominantly to early-stage cases.
- Given that over half of patients with Paraganglioma in Hong Kong present at advanced stages, a significant proportion cannot effectively benefit from surgical interventions (Hong Kong Central Cancer Registry, 2024).
- Consequently, surgery alone cannot represent a comprehensive strategy for managing Paraganglioma.
Metabolic Resistance Mechanisms in Traditional Therapies
Cancer cells, including Paraganglioma, exhibit unique metabolic alterations enhancing their resilience against traditional therapeutic modalities—commonly known through the Warburg effect and related metabolic pathways.
Rapid DNA Repair and Therapy Resistance
- Enhanced DNA repair capacity (up to 400% increase in DNA repair enzymes), a characteristic of cancer cells, significantly hampers chemotherapy and radiation effectiveness (Nature Reviews Cancer, 2024).
- As Paraganglioma cells swiftly rectify chemotherapy or radiation-induced DNA damage, treatments lose power rapidly, often triggering tumor resurgence in Asian patients.
Metabolic Adaptability and Treatment Failure
- Metabolic flexibility of tumor cells, particularly the switch to glycolysis with up to 200-times higher glucose consumption than healthy tissue, diminishes conventional therapies’ effectiveness (Hong Kong Cancer Research Institute, 2023).
- Such metabolic pivoting allows Paraganglioma cells to thrive despite initial treatment success, eventually leading to recurrence or progression.
- Identifying and targeting this metabolic dependency offers a promising new therapeutic angle contrasting sharply with the limited efficacy of traditional chemotherapy and radiation.
Concluding Thoughts: Moving Beyond Traditional Limitations
Overall, traditional therapeutic options for Paraganglioma in Hong Kong and broader Asia exhibit considerable limitations in efficacy, safety, and long-term patient outcomes. These limitations underscore an urgent imperative for newer, innovative therapeutic avenues. Embracing novel metabolic strategies, supported through pioneering cancer biology research, represents a transformative path forward—one resonating powerfully within oncology’s evolving landscape.