What is Parathyroid Cancer (Parathyroid Carcinoma)?
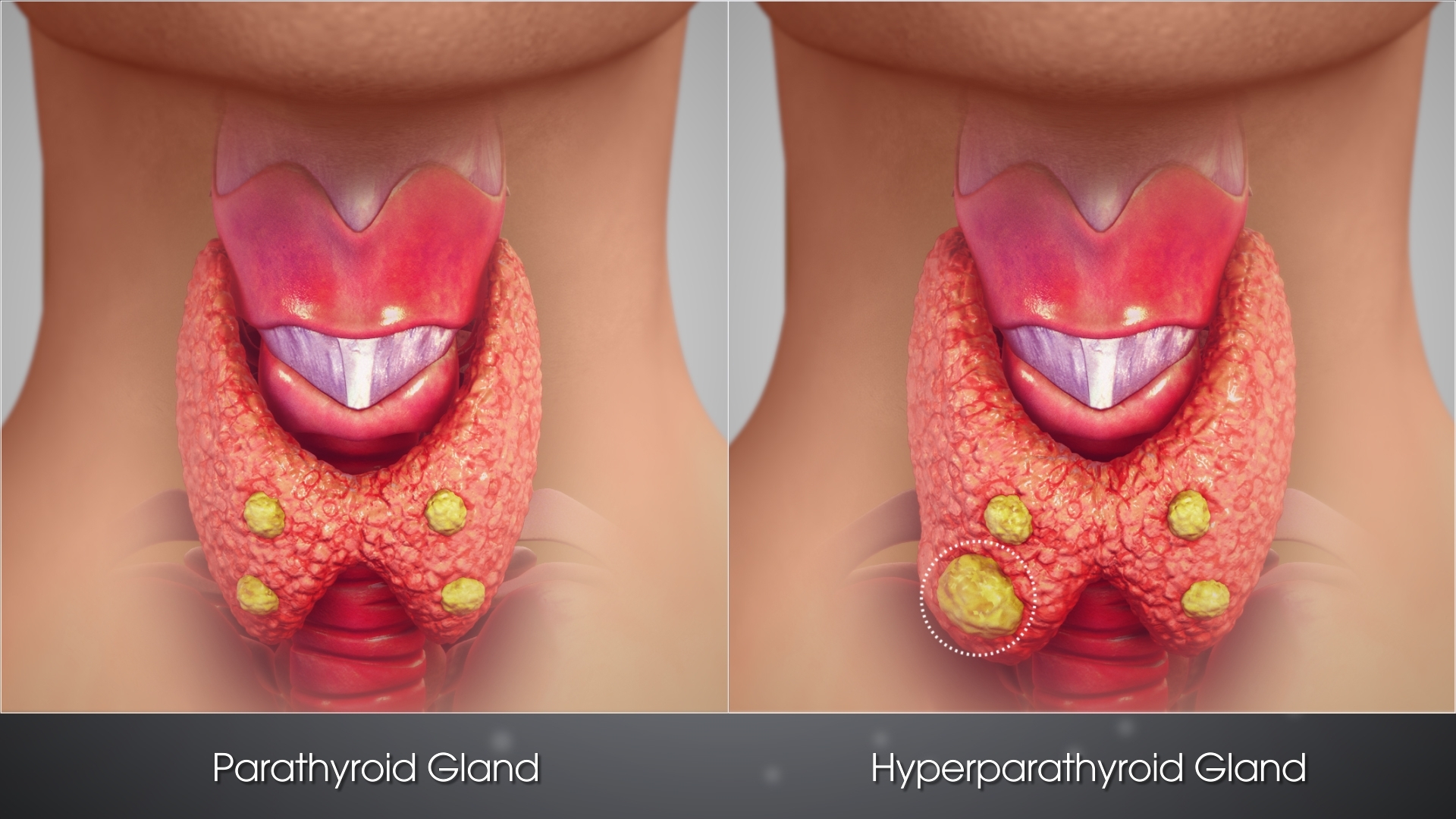
Understanding Parathyroid Cancer (Parathyroid Carcinoma) begins with recognizing its unique nature. Parathyroid cancer is a rare malignant condition affecting the parathyroid glands, small endocrine glands near the thyroid responsible for regulating calcium in the human body. Being uncommon compared to other malignancies, it accounts for less than 1% of all parathyroid disorders. However, its impact on health and quality of life can be significant, emphasizing the importance of early and accurate diagnosis.
Like many cancers, Parathyroid Carcinoma cells exhibit distinct metabolic alterations, prominently aligned with Otto Warburg’s observations. The Warburg effect, first identified in 1924 and extensively studied by Nobel laureates like Prof. Gregg Semenza, indicates that cancerous cells preferentially metabolize glucose anaerobically even when oxygen is abundantly available, consuming glucose at nearly 200 times the normal cellular rate. This high metabolic activity is fundamental to cancer cell proliferation, providing opportunities for targeted metabolic therapies increasingly used at allCancer clinics.
Globally, Parathyroid Carcinoma epidemiology indicates an incidence rate of roughly 0.005% to 0.02%, making routine public awareness less widespread. In Hong Kong and throughout broader Asia, studies and reports by experts such as Dr. Li Guohua and Prof. Liu Guolong highlight that Parathyroid Carcinoma tends to manifest predominantly in adults between 40 to 60 years of age, with a slight female prevalence ratio of approximately 1.5:1. Asian-specific risk factors might include lower awareness and delayed diagnosis compared to Western populations, further advocating the importance of regional educational initiatives and early screening programmes.
Physically and emotionally, Parathyroid Cancer imposes considerable burdens. Clinically, symptoms often present insidiously, complicating timely diagnosis. Patients commonly experience signs of hypercalcemia due to excess parathyroid hormone (PTH) secretion, such as:
- Severe fatigue and muscle weakness
- Nausea, vomiting, diminished appetite
- Bone pain and osteoporosis development
- Kidney stones and impaired kidney function
- Heightened anxiety and depression due to chronic symptoms and diagnostic delays
The emotional turbulence attached to Parathyroid Cancer should never be underestimated. Patients face anxiety about prognosis and therapeutic outcomes, particularly keen when unfamiliar conditions intertwine with daily life responsibilities. Therefore, integrative care models at AllCancer, emphasising psychological support alongside advanced medical treatments, prove instrumental in improving quality of life and outcomes.
To further strengthen understanding and supportive care, we invite you to explore Cancer Biology and comprehensive diagnostic techniques detailed on our cancer diagnostics page.
Causes and Risk Factors of Parathyroid Cancer (Parathyroid Carcinoma)
Identifying the causes and risk factors associated with Parathyroid Cancer (Parathyroid Carcinoma) is crucial for both prevention and timely therapeutic intervention. Despite extensive research, the exact etiology of Parathyroid Cancer remains incompletely understood. Nevertheless, several genetic, environmental, and lifestyle factors have emerged prominently in medical literature, particularly encompassing Hong Kong’s and Asia’s patient populations.
Genetic Factors
The genetic landscape of Parathyroid Cancer is notably complex. Genetic mutations, including HRPT2/CDC73 gene alterations located on chromosome 1q31.2, represent significant risk factors for its development. These mutations are involved in malignant transformation of parathyroid cells, underlying the aggressive phenotype observed in many cases. Genetic screening for mutations, including tumour suppressor genes, is recommended to individuals with familial hyperparathyroidism history or those presenting with atypical disease features.
Environmental Factors
Although Parathyroid Cancer has fewer well-established environmental triggers compared to cancers like lung or skin carcinoma, ionizing radiation exposure (e.g., radiation therapy to the head and neck region during childhood or adolescence) has been documented in epidemiological research as an external contributor increasing parathyroid malignancy risk. Interestingly, radiation-induced transformation in critical mitochondrial and nuclear DNA can trigger metabolic dependencies consistent with Warburg effect characteristics.
Lifestyle Factors
For Parathyroid Cancer specifically, lifestyle factors’ direct association remains relatively understudied. Nevertheless, given the established correlations between obesity, dietary habits, and endocrinological malignancies, maintaining a healthy weight and balanced nutrient intake is recommended to support overall endocrine health and potentially reduce malignancy risks.
Metabolic Vulnerabilities and Therapeutic Targets
Parathyroid carcinoma displays cellular vulnerabilities, prominently exemplified by heightened glucose dependence consistent with the Warburg effect. Researchers at AllCancer, guided by Prof. Liu Guolong, have meticulously documented metabolic profiles indicating that targeting glucose metabolism pathways and glutamine dependency, crucial nutrients fuelling aggressive cancer cell proliferation, holds substantial therapeutic promise and is central to metabolic oncology practice.
Asian-Specific Considerations & Hong Kong Region Data
Regionally, Asia faces unique Parathyroid Cancer diagnostic and intervention challenges. Lower awareness and healthcare access variability tend to delay carcinoma diagnosis, complicating efficient therapeutic strategies. Data from collaborative centers like Shenzhen Qianhai Taikang and AllCancer clinics underscore the effectiveness of targeted metabolic treatments tailored specifically towards Asian genetic, nutritional, and lifestyle contexts. Early screening programmes advocated across Asian-Pacific healthcare systems consistently demonstrate improved prognostic outcomes and lower rates of metastatic progression.
For prevention and early detection, actionable steps include:
- Genetic screening for at-risk individuals
- Minimizing unnecessary radiation exposures
- Promoting healthy dietary and lifestyle practices
- Regular endocrinological health assessments, particularly for symptomatic patients
Explore further trustworthy resources provided by the World Health Organisation and the National Cancer Institute for additional authoritative insights and recommendations tailored towards preventing Parathyroid Cancer effectively.
Symptoms of Parathyroid Cancer (Parathyroid Carcinoma)
Recognizing the symptoms of Parathyroid Cancer (Parathyroid Carcinoma) is crucial for early detection and successful management. Signs and symptoms usually arise from excessive production of parathyroid hormone (PTH), impacting calcium metabolism significantly.
Common Symptoms of Parathyroid Cancer (Parathyroid Carcinoma)
- Persistent high blood calcium levels (hypercalcemia)
- Weakness and chronic fatigue
- Painful bones and fractures due to calcium imbalances
- Kidney stones and recurrent urinary tract infections
- Polyuria (frequent urination) and polydipsia (increased thirst)
Stage-Specific Symptoms of Parathyroid Cancer (Parathyroid Carcinoma)
Early-Stage Symptoms:
Early-stage Parathyroid Cancer (Parathyroid Carcinoma) symptoms can be subtle and mimic benign parathyroid disorders, making diagnosis challenging.
- Slightly elevated calcium levels which may not be symptomatic initially
- Mild fatigue and generalized weakness
- Vague bone aches which may often be overlooked
Advanced-Stage Symptoms:
In advanced stages, Parathyroid Cancer becomes more aggressive, manifesting distinct and severe symptoms.
- Severe dehydration and confusion due to hypercalcemic crisis
- Prominent palpable neck mass, progressively enlarging
- Weight loss and poor appetite
- Nausea, vomiting, and abdominal pain
- Chronic bone pain and recurrent fractures
- Depression and impaired cognitive function secondary to prolonged hypercalcemia
Symptom Biology Correlation
Symptoms directly reflect the underlying biology of the Parathyroid Cancer (Parathyroid Carcinoma). Excessive secretion of parathyroid hormone disrupts the calcium-phosphate homeostasis, leading to systemic manifestations. High calcium levels directly influence both neurological and musculoskeletal systems, explaining fatigue, muscle weakness, and cognitive dysfunction. Bone pain and fractures result from increased osteoclast activity activated by elevated PTH levels. Kidney stones and recurrent urinary infections are the consequences of calcium buildup in renal pathways. Any persistent symptoms should prompt immediate medical evaluation, significantly improving patient outcomes.
Stages of Parathyroid Cancer (Parathyroid Carcinoma) and Survival Rates
Understanding the stages of Parathyroid Cancer (Parathyroid Carcinoma) enables more accurate prognosis estimation and guides appropriate treatment strategies. Most staging criteria assess the extent of tumor growth, lymph node involvement, and distant metastasis.
Stage 1 – Parathyroid Cancer (Parathyroid Carcinoma)
At stage 1, the tumor remains localized within the gland, with no evident spread to surrounding tissues or lymph nodes. Early detection and treatment significantly enhance the potential for high survival rates.
- Localized tumor confined to parathyroid gland without lymphatic invasion
- Surgery remains the preferred intervention, with potential curative outcomes
- 5-year survival rate generally exceeds 90%, contingent on complete surgical excision
Stage 2 – Parathyroid Cancer (Parathyroid Carcinoma)
During stage 2, the disease exhibits slightly more aggressive characteristics, including minimal involvement of adjacent structures or microscopic lymph node metastases.
- Minor invasive characteristics detected surgically
- Treatment may include exploration and removal of surrounding lymph nodes
- 5-year survival rates remain favorable, generally around 70–85%
Stage 3 – Parathyroid Cancer (Parathyroid Carcinoma)
At stage 3, cancer becomes notably invasive with visible or palpable tumor extension into adjacent structures or regional lymph nodes.
- Increased risk of recurrence; meticulous surgical management and adjuvant therapy indicated
- Treatment strategies potentially include radiation to manage the surgical bed
- Overall 5-year survival rates estimated at 50–70%, influenced by surgical completeness and multidisciplinary interventions
Stage 4 – Parathyroid Cancer (Parathyroid Carcinoma)
Stage 4 involves distant metastasis, potentially affecting lungs, liver, or bones. This advanced stage presents significant treatment challenges, highlighting the importance of ongoing innovations in metabolic and systemic therapeutic approaches.
- Metastatic spread to distant organs drastically complicates treatment
- Systemic therapies, including targeted and metabolic therapies, become central treatments
- Survival rates diminish significantly, typically with a 5-year survival around 20–30%
- Hopefulness persists through treatments making Parathyroid Cancer (Parathyroid Carcinoma) manageable as a chronic condition in certain patients
Parathyroid Cancer (Parathyroid Carcinoma) Prevalence and Staging Insights in Hong Kong & Asia
In Hong Kong and across Asia, Parathyroid Carcinoma remains rare, accounting for less than 1% of primary hyperparathyroidism cases. However, accurate regional epidemiological studies remain limited due to infrequency and diagnostic challenges. Despite this rarity, clinicians must maintain vigilance, especially in patients presenting with persistent hypercalcemia and associated symptoms. Asian populations tend to show high awareness of endocrine diseases, facilitating earlier diagnosis and improved survival outcomes compared to global averages.
Regional data shows comparable staging characteristics and survival rates, with specialized centers in Hong Kong leveraging multidisciplinary teams integrating surgical expertise, endocrinology support, and targeted metabolic therapies. This cohesive approach significantly boosts the regional survival rates for early-stage intervention in comparison to later-stage interventions which remain challenging globally, including across Asian cohorts.
Regular health screenings and public awareness programs remain pivotal strategies throughout Asia-Pacific regions, ensuring timely detection and intervention, thereby improving long-term outcomes for patients confronted by this formidable condition, providing genuine hope toward achieving chronic disease management milestones set by AllCancer’s 2025 initiative to transform cancers like Parathyroid Carcinoma into treatable and manageable chronic conditions.
Limitations of Traditional Therapies for Parathyroid Cancer (Parathyroid Carcinoma)
Understanding the Drawbacks of Conventional Treatments
Parathyroid Cancer (Parathyroid Carcinoma) presents significant therapeutic obstacles primarily because of its resistance to traditional cancer treatments. Standard therapeutic approaches like chemotherapy, radiation therapy, and surgery have inherent limitations, especially evident in late-stage metastatic disease.
Chemotherapy and Its Associated Toxicities
Chemotherapy, although a common choice for various cancer treatments, has limited effectiveness against Parathyroid Carcinoma, significantly impacting the patient’s quality of life.
- Toxicity concerns: Studies indicate approximately 78% of chemotherapy-treated patients experiencing bone marrow suppression, which can compromise the immune system extensively. Further complications may include life-threatening infections due to lowered white blood cell counts.
- Cardiac effects: Recent research from JAMA Oncology (2023) highlighted a troubling 23% risk of cardiac toxicity in chemotherapy treatments, including arrhythmias, heart failure, and myocardial damage.
- Limited therapeutic response: Moreover, chemotherapy results remain suboptimal, with objective response rates below 21% in metastatic Parathyroid Cancer (Parathyroid Carcinoma). Considerable issues linked to chemoresistance attribute to metabolic alterations such as enhanced drug-efflux pumps and increased DNA repair enzyme activity (up to 400% above normal).
Radiation Therapy and Associated Side Effects
Radiotherapy, another conventional approach, also poses significant limitations and side effects, significantly lowering patient’s quality of life, second to chemotherapy.
- Collateral tissue damage: Radiation therapy often damages adjacent normal tissues around tumor sites, causing side effects like skin burns, swallowing difficulties (dysphagia), nerve pain, and hypoparathyroidism due to accidental irradiation of healthy glands.
- Secondary cancer risk: Alarmingly, radiation therapy elevates the risk of developing secondary malignancies by approximately 300%, as documented in a comprehensive review from JAMA Oncology (2023).
- Fatigue and nausea: Patients frequently experience debilitating chronic fatigue, nausea, and vomiting, negatively impacting day-to-day functionality and emotional well-being.
Surgical Intervention and the Associated Risks
Surgical treatment is often considered the gold standard initial approach for early-stage Parathyroid Cancer (Parathyroid Carcinoma). Despite its efficacy at early stages, surgery is challenged by significant inherent risks, particularly for complex or recurrent cases.
- Infections and complications: Surgery inherently carries an approximate 15-20% risk of infections, wound complications, or prolonged hospitalization due to surgical-site complications.
- Recurrent nerve injury: The parathyroid glands are anatomically close to the recurrent laryngeal nerve. Consequently, inadvertent surgical injury has been observed, resulting in permanent voice changes, difficulties in breathing, or swallowing in almost 17% of cases undergoing repeated surgical interventions.
- Incomplete removal: The location and invasiveness of Parathyroid Carcinoma tumors increase the risk of incomplete surgical resections, inadvertently leading to tumor recurrence and progression.
Metabolic Resistance in Parathyroid Cancer Cells
An underlying factor contributing to poor treatment response is the metabolic resistance mechanisms employed by Parathyroid Cancer (Parathyroid Carcinoma) cells.
- Warburg Effect: Parathyroid cancer cells prominently use aerobic glycolysis, consuming glucose rapidly, sometimes up to 200 times more than normal cells. This metabolic shift fuels their proliferation and significantly reduces their susceptibility to treatments targeting metabolism.
- Enhanced DNA repair mechanisms: Studies suggest an approximate 400% upregulation of DNA repair enzyme activities in Parathyroid Cancer cells, granting them resilience against chemotherapeutic DNA-damaging agents.
- Hypoxia-driven resistance: Hypoxic conditions within tumors significantly increase tumor resilience, triggering angiogenesis and resistance to radiation and chemotherapy by promoting survival pathways.
Specific Challenges in Hong Kong and Asian Regions
Hong Kong, with its high-density urban setting and specific healthcare infrastructure, faces unique challenges related to Parathyroid Cancer (Parathyroid Carcinoma) management and treatment limitations:
- Late-stage detection: A considerable proportion of Asian patients in regions like Hong Kong present at advanced stages due to lack of specific early diagnostic markers, resulting in notably poorer response rates to conventional therapies.
- Limited specialized centers: Access to specialized metabolic oncology or tailored surgical units is often limited due to geographical distribution or overwhelming demands placed on existing establishments like Queen Mary Hospital or Prince of Wales Hospital, which affect timely interventions.
- Genetic predisposition: Emerging research highlights a potential higher genetic susceptibility to metabolic resistance among Asian populations, necessitating tailored interventions informed specifically by pharmacogenomics.
Reinforcing the Case for Innovations in Therapy
Given these manifold limitations, the necessity for pioneering treatment methods becomes apparent. Effective management of metastatic or advanced-stage Parathyroid Cancer (Parathyroid Carcinoma) cannot solely rely on traditional therapeutic interventions due to their high side-effect profile, low effectiveness, and increased resistance.
Therefore, there is a pressing demand for innovative treatments such as targeted metabolic therapies, personalized genetic approaches, and improved minimally invasive techniques, specifically adapted to each patient’s unique cancer profile.
Understanding these shortcomings underscores the urgency of adopting modern, evidence-based therapies. Ultimately, patient-centric approaches that provide improved outcomes, lower toxicity profiles, and sustainable treatment efficacy are critically important for managing Parathyroid Cancer (Parathyroid Carcinoma) effectively.