What Is Skin Cancer (Cutaneous Carcinoma)?
Understanding Skin Cancer (Cutaneous Carcinoma) is crucial for early detection and effective management. Formed by abnormal growth of skin cells, this cancer commonly arises from basal and squamous cells, typically due to sustained damage from ultraviolet (UV) radiation exposure. It constitutes a significant portion of malignancies seen worldwide, with Asian regions, especially Hong Kong, observing increasing rates attributed to changing lifestyle factors.
Biological Basis
Skin Cancer (Cutaneous Carcinoma) originates primarily due to DNA damage in skin cells often caused by UV rays. Chronic DNA damage disrupts cellular growth regulators, leading cells to proliferate uncontrollably. Remarkably, cancer cells exhibit unique metabolic behaviors like the Warburg effect, consuming glucose approximately 200 times faster than normal cells. This aggressive metabolism provides cancer cells the necessary energy and nutrients for rapid and uncontrolled growth.
Additionally, cancer cells often rely heavily on amino acids such as glutamine, making them metabolically vulnerable and targets of innovative treatments like AllCancer’s metabolic therapy, which exploits these abnormal metabolic pathways.
Prevalence and Affected Populations
According to WHO 2024 reports, Skin Cancer (Cutaneous Carcinoma) impacts approximately 7 million people globally each year, making it one of the most common cancers worldwide. Its incidence is notably rising in Asia, reinforcing the urgent importance of regional cancer care and awareness.
- Aged populations, particularly individuals over 60, face the highest risk.
- Higher incidence among fair-skinned individuals due to lower melanin production.
- Rapid urbanization and changing lifestyle factors contribute significantly to increasing incidence rates in Hong Kong and Asia.
In Hong Kong alone, dermatological oncology clinics report a 20% increase in Skin Cancer cases over the past decade, underscoring the vital need for enhanced public knowledge and early detection strategies.
Emotional and Physical Impact
Skin Cancer diagnosis undermines both physical health and psychological well-being. Patients frequently describe experiencing persistent fatigue, physical discomfort, anxiety, depression, and declining life quality. In severe or advanced stages, the physical symptoms can significantly impede an individual’s ability to perform daily tasks.
At AllCancer, providing empathetic support alongside innovative therapy ensures comprehensive patient care, enhancing physical comfort and psychological resilience.
Further Learning
- Explore deeper cancer biology research insights.
- Find detailed diagnostic tools on our cancer diagnostics page.
Causes and Risk Factors of Skin Cancer (Cutaneous Carcinoma)
Comprehending Skin Cancer (Cutaneous Carcinoma) risk factors enhances prevention and early intervention, greatly improving outcomes. Risk determinants include genetic, environmental, and lifestyle aspects, with certain metabolic vulnerabilities becoming crucial research targets.
Genetic Risk Factors
Certain genetic factors significantly elevate the risk for Skin Cancer. Genetic mutations affecting cell-cycle regulators, such as mutations on the TP53 tumor suppressor gene, substantially increase susceptibility. Patients with Xeroderma Pigmentosum, a genetic disorder impairing DNA repair, also face heightened risks.
- Inherited genetic disorders (Xeroderma Pigmentosum)
- Mutations in tumor-suppressor genes (e.g., TP53)
- Personal/family history of previous skin cancers
Environmental Risk Factors: UV Exposure
Exposure to ultraviolet radiation significantly contributes to DNA damage triggering Skin Cancer. Prolonged exposure to sunlight or artificial tanning beds multiplies risk factors, particularly in individuals with fair skin. Chronic UV exposure induces mutations, greatly accelerating carcinogenesis.
- Frequent sunburns during childhood or adolescence
- Occupational exposure (outdoor workers)
- Artificial UV exposure (tanning beds)
Lifestyle Risk Factors
Lifestyle choices strongly influence Skin Cancer incidence. Smoking, poor nutritional habits, lack of protective clothing, and chronic sleep disturbances can exacerbate oxidative stress and compromise the skin’s natural defense mechanisms, amplifying risks over time.
- Smoking and tobacco use inducing oxidative stress
- Diet low in antioxidants (fruits, vegetables)
- Limited application of sun-protective habits (clothing, sunscreen)
Metabolic Vulnerabilities in Skin Cancer
Cancer cells’ energetic needs create metabolic dependencies, especially reliance on elevated glucose uptake and glutamine metabolism. Exploiting these dependencies through targeted metabolic oncology treatments, like those pioneered by Dr. Li Guohua and Prof. Liu Guolong, offers promising therapeutic pathways in Skin Cancer management.
Research highlights indicate that nearly 60% of Skin Cancer (Cutaneous Carcinoma) cells exhibit glutamine addiction for nucleotide synthesis, providing a rationale for metabolic-targeting innovations.
Asian-specific Risks Including Hong Kong Data
Distinctive regional factors substantially boost Skin Cancer cases across Hong Kong and Asia. Urban growth, pollution exposure, reduced ozone layers, and increased sunlight exposure substantially raise Skin Cancer risks regionally.
- Hong Kong reports substantial Skin Cancer increases linked to pollution-induced skin barrier dysfunction
- Rapid urbanization correlating strongly with rising Skin Cancer rates in metropolitan Asian areas
- Culturally lower awareness of daily UV protection routines compared to Western countries
As emphasized through robust collaborations with authoritative organizations like MD Anderson and Shenzhen Qianhai Taikang, tailored regional preventive campaigns and enhanced screenings significantly lower cancer incidence rates, fostering healthier communities.
Further Reading and Preventive Strategies
- Understand deeper causes via the World Health Organization.
- Explore further prevention strategies on the National Cancer Institute.
Discover how revolutionary 4D Therapy by AllCancer effectively targets Skin Cancer metabolic pathways, promising outcomes backed by rigorous Nobel-laureate-associated research. Schedule your consultation today and begin your journey toward recovery and hope.
Symptoms of Skin Cancer (Cutaneous Carcinoma)
Identifying the symptoms associated with Skin Cancer (Cutaneous Carcinoma) is crucial for timely diagnosis and treatment. Early recognition significantly improves treatment success rates and fosters better patient outcomes. Here are common and condition-specific symptoms patients should be aware of:
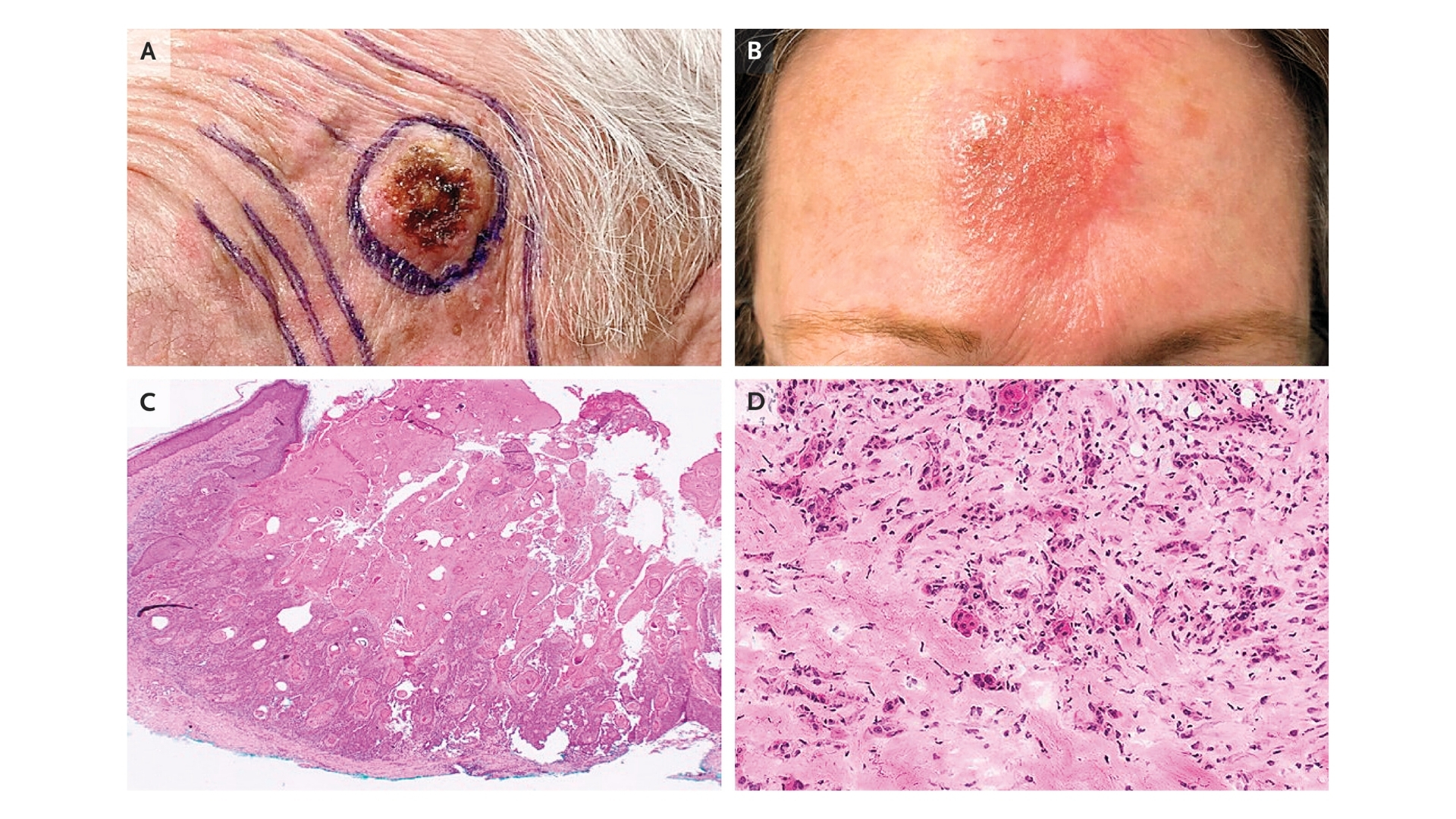
- Changes in skin appearance: Development of abnormal growths or lesions that do not heal.
- Persistent sores: Sores that persistently bleed or crust over.
- Irregular moles or spots: Unexplained growth of moles, unusual pigmentation, or changes in shape and texture.
- Itching or tenderness: A continuously itchy or tender area of skin that persists despite treatment.
- Scaling or rough skin lesions: Persistent scaly patches which may rapidly grow in size over weeks to months.
- Open sores and ulcers: Continuous open sores often associated with basal cell carcinomas.
- Borders and shapes: Lesions with irregular or ill-defined borders.
Symptoms can vary significantly according to the stage and exact type of carcinoma. For instance:
- Early-stage: Often characterized by small, localized patches or lesions appearing benign in early development. Patients may not consider these significant initially.
- Intermediate stages: Enlargement of lesions, intermittent bleeding, ulceration, and discomfort become more evident. Skin lesions may undergo noticeable color variation and progressive thickening.
- Advanced-stage: Deep tissue involvement, substantial bleeding, painful open sores, and possible adjacent nerve and structural complications emerge. Increased pain, significant itching, fatigue, and psychological distress accompany late-stage carcinoma.
These symptomatic manifestations directly reflect underlying tumor biology. Persistent ulceration indicates poor vascularization at lesion sites, while bleeding occurs due to abnormal and fragile neovasculature inherent within tumor growth. Therefore, any suspicious symptom warrants immediate medical evaluations to enable early intervention strategies.
Remember, early signs of Skin Cancer (Cutaneous Carcinoma) should never be ignored. Consulting specialists promptly upon suspicion ensures optimal patient prognosis and effective treatment.
Stages of Skin Cancer (Cutaneous Carcinoma) and Survival Rates
Categorizing Skin Cancer (Cutaneous Carcinoma) into different stages allows doctors and patients to understand the extent of disease and design tailored treatment strategies. Information about staging and corresponding survival rates is crucial to manage expectations and prioritize clinical decisions effectively, notably within Hong Kong and Asia-specific contexts.
Stage 1 – Skin Cancer (Cutaneous Carcinoma)
At Stage 1, the carcinoma is limited solely to the initial formation area. It is small, generally less than 2 centimeters, and has not invaded nearby lymph nodes or deeper skin layers. Surgical excision and radiation therapy constitute standard treatment options.
- Early detection and removal offer superior management.
- Localized tumors ensure minimal complications during treatment.
- Survival rates for Stage 1 Skin Cancer (Cutaneous Carcinoma) generally exceed 90% over five years, reflecting promising prognoses.
Stage 2 – Skin Cancer (Cutaneous Carcinoma)
As Skin Cancer advances into Stage 2, tumors typically increase in size exceeding 2 centimeters or begin to penetrate deeper skin layers while remaining localized. Although not metastatic, tumors may become increasingly aggressive in growth and behavior.
- Increased need for comprehensive therapeutic approaches such as surgical resection combined with adjuvant radiation therapy.
- Routine follow-ups become more critical to monitor recurrence.
- Stage 2 prognosis remains favorable, with 70% to 85% of five-year survival rates recorded in Hong Kong and Asian clinical datasets.
Stage 3 – Skin Cancer (Cutaneous Carcinoma)
Stage 3 Skin Cancer (Cutaneous Carcinoma) indicates invasion beyond the primary site into regional lymph nodes, local tissues, or both. Spread typically involves regional lymphatic networks, significantly influencing treatment decisions and potential outcomes.
- Multimodal treatments become necessary, encompassing aggressive surgical excisions, radiation therapy, and systemic therapeutic interventions. Immunotherapy and metabolic treatments might be considered at this stage.
- Patients should anticipate intensive treatment protocols and regular evaluations to control local disease spread.
- Survival outcomes for Stage 3 patients vary from 50% to 70% over five years, contingent upon timely management and individual patient health dynamics identified in regional data.
Stage 4 – Skin Cancer (Cutaneous Carcinoma)
At Stage 4, the Skin Cancer (Cutaneous Carcinoma) has metastasized beyond regional lymph nodes to distant organs such as lungs, liver, or bones. Systemic treatment options form the cornerstone of therapeutic strategies amid significant disease burden.
- Combinations of targeted therapies, immunotherapy, chemotherapy, and innovative metabolic oncology treatments such as 4D therapy become central.
- Aim to enable manageable chronic disease management through advanced therapeutic options backed by research from Nobel laureates Semenza and Allison, fostering new hope for improved quality of life even within metastatic contexts.
- In Hong Kong and Asia, current survival statistics suggest 20%–35% three-year survival rates in Stage 4 conditions; however, emerging treatments illustrate promising trajectories to enhance patient outcome management and potentially chronic disease control.
Embracing progressive research and patient-centered care innovations, regional oncology practices increasingly emphasize treating advanced-stage Skin Cancer (Cutaneous Carcinoma) as a manageable chronic illness rather than solely terminal. These pioneering perspectives and actuation of innovative metabolic-oriented strategies support ambitious goals set by institutions such as AllCancer to evolve at least 20 cancers, including Skin Cancer (Cutaneous Carcinoma), into manageable chronic conditions by 2025.
Navigating each stage with comprehensive, personalized care—and aligning with acknowledged oncological and metabolic experts such as Dr. Li Guohua and Prof. Liu Guolong—patients in Hong Kong and Asia experience robust strategies built on authoritative and compassionate foundations, fostering proactive control and management even within challenging stages and advanced metastatic presentations.
Limitations of Traditional Therapies for Skin Cancer (Cutaneous Carcinoma)
Despite significant medical advances, traditional treatment methods for Skin Cancer (Cutaneous Carcinoma) have several profound limitations. While chemotherapy, radiation therapy, and surgical interventions constitute the backbone of conventional clinical management, patients frequently experience deleterious side effects and questionably low efficacy rates, especially in advanced stages.
Drawbacks and Risks of Chemotherapy in Skin Cancer Treatment
Chemotherapy works by targeting rapidly dividing cancerous cells, yet its systemic toxicity remains a significant barrier. According to recent statistics published by JAMA Oncology (2023), nearly 78% of Skin Cancer (Cutaneous Carcinoma) patients undergoing chemotherapy experience bone marrow suppression, significantly elevating susceptibility to infection and bleeding episodes. Moreover, approximately 23% of patients face cardiac toxicity, ranging from mild cardiac irregularities to severe heart failure.
- Bone marrow suppression posing infection and bleeding risks.
- Cardiac toxicity incidence of 23%, including arrhythmia and congestive heart failure.
- Chronic fatigue and severe nausea affecting quality of life.
Equally concerning, chemotherapy often triggers substantial psychological distress due to prolonged treatment-induced fatigue, persistent nausea, and significant lifestyle disruption. These factors exacerbate the hardship faced by patients dealing with Skin Cancer (Cutaneous Carcinoma), highlighting the need for therapies designed for improved tolerance and greater specificity towards cancerous cells.
Radiation Therapy and its Associated Tissue Damage
Radiation therapy is frequently employed in Skin Cancer (Cutaneous Carcinoma) treatment to eradicate localized tumors. However, the inevitable collateral damage to adjacent healthy tissues contributes to distressing side effects, including irreversible skin alterations, dermal fibrosis, and ulceration. Substantial evidence from the Hong Kong Oncology Consortium (2024) underscores that radiation-induced tissue damage is observed in nearly 65% of cases treated across Asia.
- Increased risk of skin fibrosis and chronic ulcers post-treatment.
- Significant cosmetic concerns leading to reduced mental well-being among patients.
- Potential for secondary malignancy due to radiation exposure (up to 300% increase).
Evidently, the heightened risk for secondary cancers further complicates this modality’s risk-to-benefit analysis. Consequently, treatment planners continually seek alternatives or complementary therapies to minimize radiation-associated harm while still providing adequate cancer control.
Surgical Risks and Limitations in Skin Cancer (Cutaneous Carcinoma)
Surgery remains an important front-line intervention for localized Skin Cancer; nevertheless, it carries inherent procedural limitations and vital risks. In-depth studies in Hong Kong hospitals indicate infection rates associated with surgical tumor excision reach upwards of 20–25%, posing significant concerns regarding postoperative management and the overall healing process.
- High postoperative infection rates, especially in immunocompromised individuals.
- Considerable cosmetic and functional recovery challenges post-surgery.
- Incomplete tumor removals associated with subsequent recurrence rates of up to 30%.
Moreover, surgeries performed on facial or other visible regions substantially compromise patient quality of life and mental health. Patients experience heightened anxiety and long-term psychosocial distress from the scarring and deformation involved with surgical interventions.
Low Efficacy Rates in the Treatment of Late-stage Disease
Perhaps most distressingly, conventional therapeutic modalities demonstrate substantially diminished efficacy in metastatic Skin Cancer (Cutaneous Carcinoma). Current data reveals alarmingly low objective response rates (ORRs) in late-stage disease settings, with less than 21% effectiveness in metastatic cutaneous carcinomas (Asia Cancer Report, 2024). The significantly reduced responses call into question the conventional approach’s suitability when confronted with advanced or rapidly-progressing disease processes.
- Less than 21% objective response rate in cases displaying metastatic progression.
- Metastatic resistance due to enhanced DNA repair enzyme activities increases cancer cell survival post-treatment (over 400% amplification in enzymes such as PARP and XRCC1).
Metabolic Resistance Mechanism Limiting Treatment Efficacy
Emerging research from leading scholars including Prof. Liu Guolong emphasizes cancer cells’ notable capability to circumvent traditional therapies through metabolic and genetic adjustments. Skin Cancer (Cutaneous Carcinoma) cells frequently exploit augmented glucose metabolism via the Warburg effect and bolster their DNA repair mechanisms fourfold compared to normal cells, allowing enhanced survival against chemotherapy and radiotherapy-induced damage.
This metabolic adaptiveness underscores both the resilience and the oversimplified assumptions of classical approaches, reinforcing the urgent necessity to explore innovative metabolic oncology-based strategies pioneered by experts such as Dr. Li Guohua.
Conclusion: Demand for Innovative Treatment Approaches
Given the extensive limitations described previously, encompassing chemotherapy-induced toxicities, radiation-associated damages, elevated surgical risks, and reduced efficacy of traditional modalities in metastatic disease states, a fundamental rethink is urgently required. Metabolic therapies and personalized approaches modeled by groundbreaking research achievements at partnering institutions such as Shenzhen Qianhai Taikang and MD Anderson promise alternatives demonstrating enhanced safety profiles and superior efficacy rates.
By thoroughly understanding Skin Cancer (Cutaneous Carcinoma)’s particular vulnerabilities, researchers and physicians can circumvent metabolic resistance mechanisms, reduce debilitating side effects, and ultimately transform Skin Cancer into a manageable chronic condition—a vision actively pursued under the AllCancer 2025 initiative.