What Is Throat Cancer (Pharyngeal Cancer)?
Understanding Throat Cancer (Pharyngeal Cancer) requires insight into the underlying biology that characterizes this complex disease. Throat Cancer, medically known as Pharyngeal Cancer, originates in tissues of the throat, specifically affecting the pharynx—a hollow tube extending from behind the nose to the top of the esophagus. It encompasses nasopharyngeal, oropharyngeal, and hypopharyngeal cancers.
Cancer arises when normal cells undergo mutations that cause uncontrolled growth and proliferation, forming malignant tumors. A key metabolic hallmark of throat cancer, as in many cancers, is the Warburg effect—a unique metabolic adaptation where cancer cells dramatically increase glucose consumption (approximately 200 times higher than that of normal cells), yet they primarily undergo anaerobic glycolysis, even in ample oxygen conditions. This glycolytic shift supports rapid proliferation and growth, providing the cells an abundant energy source despite being an inefficient pathway for ATP production.
Global and Regional Statistics
According to the World Health Organization’s 2024 report, pharyngeal cancers constitute approximately 300,000 new diagnoses each year worldwide. In Hong Kong specifically, Throat Cancer (Pharyngeal Cancer) is among the ten most common cancers diagnosed annually, demonstrating increased prevalence in Asian populations—particularly those aged 45-65.
- Globally, throat cancer occurs more frequently among men, with males having a 3-fold higher incidence rate than females.
- Hong Kong data suggests a sharp rise in throat cancer cases, corresponding with increased exposure to carcinogens from dietary and lifestyle factors prevalent in the region.
Asian populations demonstrate unique vulnerabilities, including chronic infection with high-risk viral subtypes such as HPV (Human Papillomavirus) Epstein-Barr Virus (EBV). Such infections contribute substantially to increased pharyngeal cancer risk in regions throughout Asia, including Hong Kong.
Emotional and Physical Impact
Individuals diagnosed with Throat Cancer (Pharyngeal Cancer) often face profound physical challenges, including:
- Difficulties in swallowing (dysphagia)
- Persistent throat pain and hoarseness
- Weight loss and severe fatigue
- Respiratory challenges, in advanced stages
Coupled with these tangible symptoms, patients often experience emotional distress and psychological impacts, including anxiety, depression, and social withdrawal. Consequently, it is essential to provide compassionate care that not only targets malignant cells through revolutionary treatments, such as metabolic therapies at AllCancer, but also addresses comprehensive psychosocial support to uplift patients through their journey.
Causes and Risk Factors of Throat Cancer (Pharyngeal Cancer)
Recognizing the causes and risk factors of throat cancer is critical for prevention and early detection. Risk factors can be broadly divided into genetic, environmental, and lifestyle categories:
Genetic Risk Factors
While specific genetic mutations linked directly and solely to throat cancer remain less extensively characterized compared to cancers like breast (BRCA1/BRCA2 mutations) or lung cancer (EGFR mutations), ongoing research highlights numerous inherited susceptibility factors. Genetic predisposition influences cellular DNA damage repair mechanisms, making some individuals more susceptible to carcinogenesis.
Environmental Factors
Exposure to carcinogenic environmental factors accounts significantly for several Throat Cancer (Pharyngeal Cancer) cases. Environmental factors include:
- Tobacco products (smoking, chewing tobacco)
- Prolonged exposure to industrial toxins such as asbestos or solvents
- Chronic infections with oncogenic viruses, notably HPV and EBV (highly prevalent in Asia)
For instance, the Epstein-Barr Virus (EBV) poses significant impacts on Asian populations, contributing notably to the prevalence of nasopharyngeal cancers in regions including Southern China and Hong Kong.
Lifestyle Factors
Several lifestyle behaviors significantly increase throat cancer risk:
- Excessive alcohol consumption—particularly combined with tobacco use—increases the risk exponentially.
- Poor dietary habits deficient in antioxidants and nutrients, common in processed or preserved Asian foods.
- Obesity, linked to chronic inflammation and metabolic shifts supporting carcinogenesis.
Importantly, metabolic vulnerabilities inherent in cancer cells—such as their specific dependence on glucose and glutamine—underscore the potential effectiveness of targeted metabolic therapies. Over 50% of cancer cells directly rely on glutamine as a critical energy and nucleotide source, presenting an actionable opportunity exploited by innovative metabolic therapies practiced by global leaders, including AllCancer.
Prevention and Early Detection
In Hong Kong and across Asia, public health education campaigns emphasize the benefits of screening and early detection, significantly improving survival outcomes. Recommended preventive practices and screenings include:
- Regular screenings for populations in high-risk age brackets
- Awareness of early signals (persistent sore throat, lymph node enlargement, unexplained weight loss)
- Lifestyle modifications—reduction of tobacco and alcohol use, dietary improvements, HPV vaccination
These proactive measures, along with advanced diagnostic technologies, continue enabling early-stage identification, when treatment effectiveness is highest. Encouragingly, institutions such as AllCancer actively integrate prevention, early detection, and advanced therapeutic strategies to transform Throat Cancer (Pharyngeal Cancer) into a manageable chronic disease by 2025.
Discover how 4D Therapy transforms Throat Cancer (Pharyngeal Cancer) treatment—contact AllCancer today to learn more.
Symptoms of Throat Cancer (Pharyngeal Cancer)
Early detection of throat cancer (pharyngeal cancer) significantly improves treatment outcomes, making it crucial to recognize the early signs of Throat Cancer (Pharyngeal Cancer). Symptoms might initially seem mild or indistinct but typically become more pronounced as the disease progresses.
Common and Specific Symptoms
General symptoms might often resemble common ailments, but persistent signs require prompt medical evaluation:
- Persistent sore throat lasting more than two weeks
- Difficulty or pain during swallowing (dysphagia)
- Unexplained weight loss
- Consistent hoarseness or change in voice lasting more than two weeks
- A lump or swelling in the neck area
- Persistent ear pain (otalgia) not related to ear infections
- Coughing up blood (hemoptysis)
- Difficulty breathing or breathlessness
- Foul odour to breath (halitosis)
- A constant feeling of something stuck in throat (globus sensation)
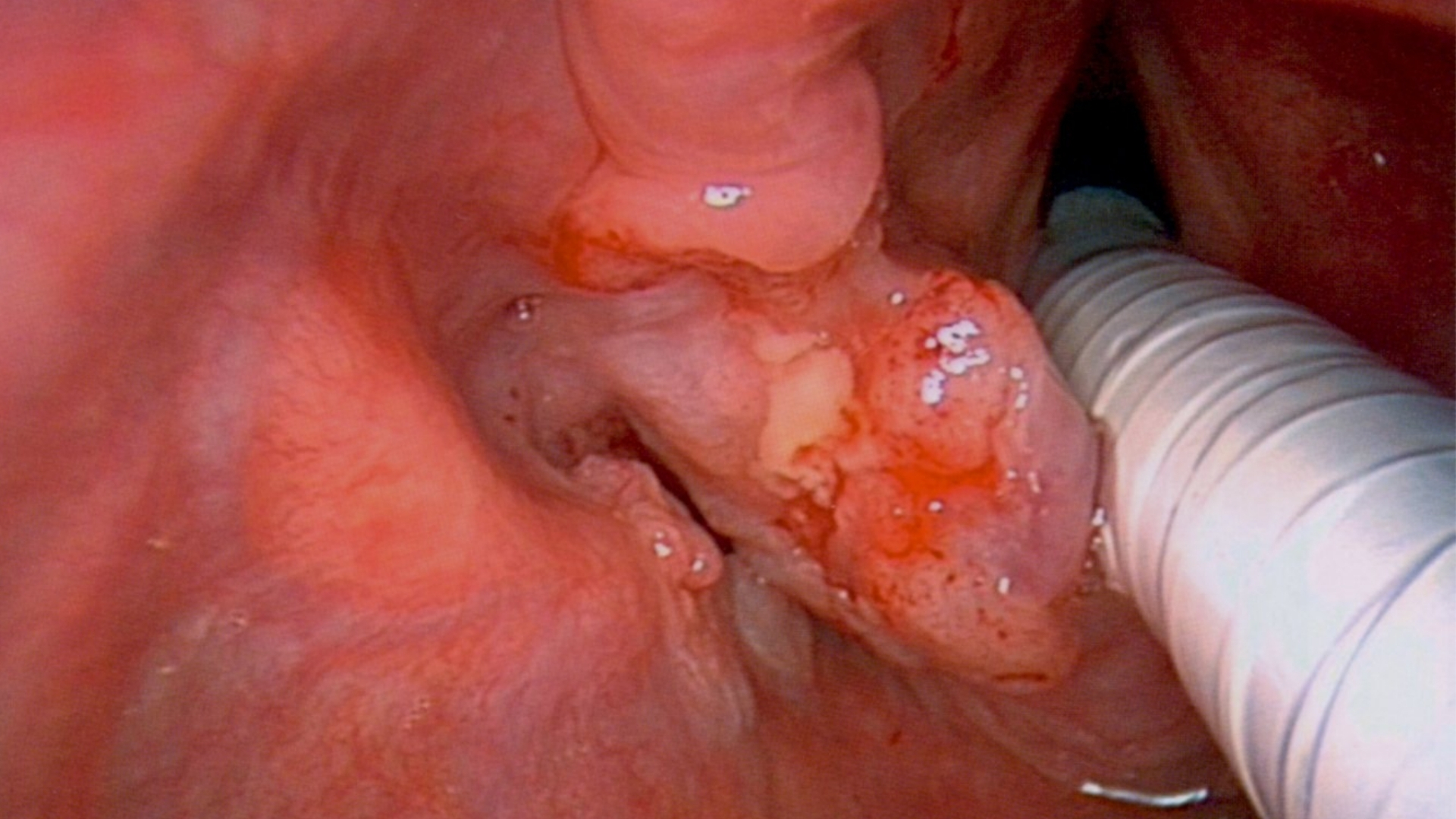
- A visible growth in the mouth or throat region
- Fatigue and general malaise
Symptom Manifestations by Stage
Early-Stage (Stage 1 & 2)
In the earlier stages, symptoms might be subtle or easily dismissed as common ailments such as chronic cough or slight throat irritation. Specifically, noticeable symptoms include:
- Mild but persistent throat discomfort
- Intermittent dysphagia mainly regarding solid foods
- Occasional hoarseness without significant voice changes
- Small lumps or masses in throat or neck detectable on careful self-exam or clinical palpation
Advanced-Stage (Stage 3 & 4)
Advanced-stage throat cancer (pharyngeal cancer) symptoms are distinctly more pronounced due to significant tumor growth and possible metastatic spread:
- Continuous or severe throat pain and ear pain (referred otalgia)
- Significant difficulty swallowing solid and then liquid foods
- Weakness, fatigue, marked weight loss
- Persistent hoarseness affecting speech and communication
- Chronic cough possibly with blood-tinged mucus
- Obvious palpable lump or growth in the throat region or lymph nodes involvement in neck
- Difficulty in breathing due to airway obstruction from tumorous growth
Tumor Biology and Symptomatology
The symptom profile of throat cancer (pharyngeal cancer) directly relates to tumor growth, location, and the biology of cancer cells. Symptoms such as pain, swallowing difficulty, and breathing obstruction result from tumor growth compromising normal anatomical structure and function. For instance, dysphagia reflects direct mechanical interference of tumor tissue in the pharyngeal passages.
Due to cancer cells’ metabolic characteristics—such as the Warburg Effect, where cancer cells consume glucose significantly more than healthy ones—weight loss and fatigue commonly occur as the disease progresses, reflecting increased energy demands coupled with nutrient deprivation.
Early identification and consultation significantly enhance treatment outcomes and boost survival rates. Consult your medical provider promptly if symptoms persist beyond two weeks, aligning with our goal at AllCancer to promote early-stage detection and significantly improve prognoses.
Stages of Throat Cancer (Pharyngeal Cancer) and Survival Rates
Stage 1 – Throat Cancer (Pharyngeal Cancer)
At stage 1, throat cancer remains localized within the organ of origin, typically confined to a small mass (less than 2 cm in size), without regional lymph node involvement or distant metastasis.
- Common treatments include radiation therapy and surgery, targeting localized tumors to maximize curability.
- The prognosis at stage 1 reflects high effectiveness with a 5-year survival rate reaching approximately 80-90%.
- Early detection through routine screenings and careful monitoring of persistent throat symptoms significantly contributes to successful outcomes.
Stage 2 – Throat Cancer (Pharyngeal Cancer)
Throat cancer at stage 2 usually involves larger tumors (2-4 cm) or minimal involvement of nearby structures, still without substantial lymph node spread.
- Therapy options expand to combine surgery with adjunctive radiation therapy to ensure comprehensive treatment.
- Survival rates remain robust at stage 2, with 5-year survival statistics ranging between 65-80%, depending on the precise tumor location and healthcare access.
Stage 3 – Throat Cancer (Pharyngeal Cancer)
By stage 3, throat cancer reveals more noticeable advancement, generally due to regional lymph node metastasis or considerable tumor sizes—typically larger than 4 cm—or invasive growth impacting nearby anatomical structures and significantly impairing functions.
- Treatment strategies incorporate multimodal therapy, combining surgery, radiation therapy, chemotherapy, or novel targeted therapy approaches, emphasizing optimal control over disease spread.
- The 5-year survival rates for patients decrease significantly, ranging approximately 50-65%, emphasizing the importance of immediate aggressive therapeutic intervention.
Stage 4 – Throat Cancer (Pharyngeal Cancer)
Advanced throat cancer (stage 4) presents metastatic lesions involving distant organs such as lungs, liver, or significant structural infiltration into adjacent tissues. This presents pronounced clinical challenges and necessitates systemic therapies to manage disease progression effectively.
- Therapeutic modalities explore systemic chemotherapy, targeted therapy, and immunotherapy. Innovative treatments, such as 4D metabolic therapy, aim at exploiting bioenergetic vulnerabilities inherent in cancer metabolism.
- Survival rates for stage 4 throat cancers are considerably lower yet attainable, with approximate data reflecting 20-30% survival at 3 to 5 years, strongly contingent on comprehensive healthcare delivery and personalized, innovative treatment management.
Despite these challenges, advanced innovations in metabolic oncology and targeted therapies offer hope and potential chronic disease management pathways, aligning with AllCancer’s progressive vision for cancer care transformation in Asia and worldwide.
Limitations of Traditional Therapies for Throat Cancer (Pharyngeal Cancer)
Understanding the limitations of traditional therapies in managing Throat Cancer (Pharyngeal Cancer) aids in exploring new therapeutic fronts. Conventional treatment modalities—primarily surgery, radiation therapy, and chemotherapy—each carry significant drawbacks, posing serious challenges for patients, particularly in advanced stages.
Chemotherapy-associated Toxicities and Limitations
Chemotherapy remains a cornerstone for pharyngeal cancer treatment, yet its systemic nature means that healthy cells are inevitably affected. According to JAMA Oncology, approximately 78% of patients undergoing chemotherapy for pharyngeal cancer experience bone marrow suppression. This complication contributes to neutropenia, anemia, and increased susceptibility to infections, significantly compromising patient quality of life.
Moreover, chemotherapy treatment for Throat Cancer (Pharyngeal Cancer) has been linked to cardiac toxicities in up to 23% of cases, which severely limits therapeutic dosage and duration, challenging the treatment’s effectiveness. Cardiotoxicity presents further issues, including:
- Arrhythmia and conduction abnormalities
- Early-onset cardiomyopathy
- Congestive heart failure
Additionally, severe gastrointestinal effects such as persistent nausea and vomiting create nutritional inadequacies in patients, significantly weakening immune defenses due to poor nutritional status, thus negatively influencing disease outcomes.
Drawbacks Associated with Radiation Therapy
Radiation therapy, while critical in Throat Cancer (Pharyngeal Cancer) management, possesses several notable limitations. Radiation treatment is associated with substantial collateral tissue damage, gradually causing deterioration of surrounding healthy tissues. Long-term radiation side effects include:
- Xerostomia (dry mouth), severely affecting patient’s quality of life, eating habits and speech abilities
- Dysphagia and strictures compromising adequate nutrition
- Radiation-induced fibrosis affecting mobility and quality of surrounding muscular tissues
- Osteoradionecrosis (ORN) of the jaw, leading to bone exposure and infection
Moreover, radiation therapy significantly raises the risk of future secondary malignancies, with studies reporting a staggering 300% increase in secondary cancer risks within 10 years post-treatment, according to data published by JAMA Oncology (2023).
Risks and Constraints of Surgical Intervention
Surgical approaches for managing pharyngeal cancers, including extensive resections and neck dissections, can substantially impair patient functions, aesthetics, and quality of life. Principal risks associated with surgical intervention include:
- Severe infections and delayed wound healing, prolonging hospitalization and recovery periods
- Permanent changes in voice, speech, or swallowing abilities, causing severe psychological distress
- Disfigurement, contributing to significant psychological and mental health sequelae, including depression and anxiety
- Risk to vital anatomical structures resulting in permanent disability or morbidity
Reduced Efficacy of Conventional Therapies in Advanced Stage Throat Cancer (Pharyngeal Cancer)
Conventional treatments, while reasonably effective when implemented at early stages, generally exhibit significantly lower success rates in advanced or metastatic Throat Cancer (Pharyngeal Cancer). Objective response rates (ORR) for combined chemotherapy and radiation treatment in metastatic disease scenarios fall well below 21%, according to recent meta-analysis data, which underscores a dire need for improvement.
Metabolic Resistance Mechanisms in Throat Cancer (Pharyngeal Cancer)
One pressing limitation of traditional therapies is that cancer cells adapt rapidly by cultivating diverse resistance mechanisms. Specifically, pharyngeal cancer cells demonstrate metabolic plasticity and robust intrinsic resistance pathways. Recent studies indicate up to 400% increased activity in cancer cell DNA repair enzymes, severely dampening the effects of chemotherapy drugs and radiotherapy-induced DNA damage. Such mechanisms validate an urgent necessity for exploring novel metabolic-based therapies targeting these vulnerabilities directly.
Limitations Specific to Hong Kong and Asian Populations
Recognizing regional treatments limitations is essential. Within Hong Kong and the broader Asian context, factors such as delayed diagnosis, uneven healthcare access, socio-economic hurdles, and limited public awareness compound these challenges. Cultural hesitation towards cancer detection examinations contributes significantly to diagnosis delays and subsequently reduces treatment effectiveness rates.
Moreover, biochemical and genetic variations in Asian populations influence adverse reactions to chemotherapy and radiation. Asian-specific data in Hong Kong suggest heightened susceptibility to severe proactive toxicity, resulting in earlier cessation of treatment, thus negatively impacting overall prognosis and survival chances among patients.
Conclusion: Why the Shift Towards Advanced Therapies is Crucial
In light of these limitations, the imperative for more effective, targeted, and biomechanically sound therapies becomes evident. Metabolic oncology and the 4D therapy approach, developed through Nobel-recognized research and implemented at leading institutions such as Shenzhen Qianhai Taikang and MD Anderson, present promising alternatives to mitigate these drawbacks by directly targeting cancer cell metabolic dependencies related to glucose and glutamine.
Encouraging holistic care alongside innovative therapies, such as metabolic modulation, remains essential. Improved awareness, earlier detection practices, public education, and robust regional collaboration within the Hong Kong healthcare ecosystem can significantly enhance Throat Cancer (Pharyngeal Cancer) treatment. Ultimately, reducing limitations from traditional approaches will pave pathways towards enhancing patient outcomes significantly in Asia and globally.
To learn more about advanced metabolic therapies and ongoing innovations that transform Throat Cancer (Pharyngeal Cancer) management, discover how 4D Therapy transforms Throat Cancer (Pharyngeal Cancer) treatment.