What Is Thymic Carcinoma (Malignant Thymus Gland Tumor)?
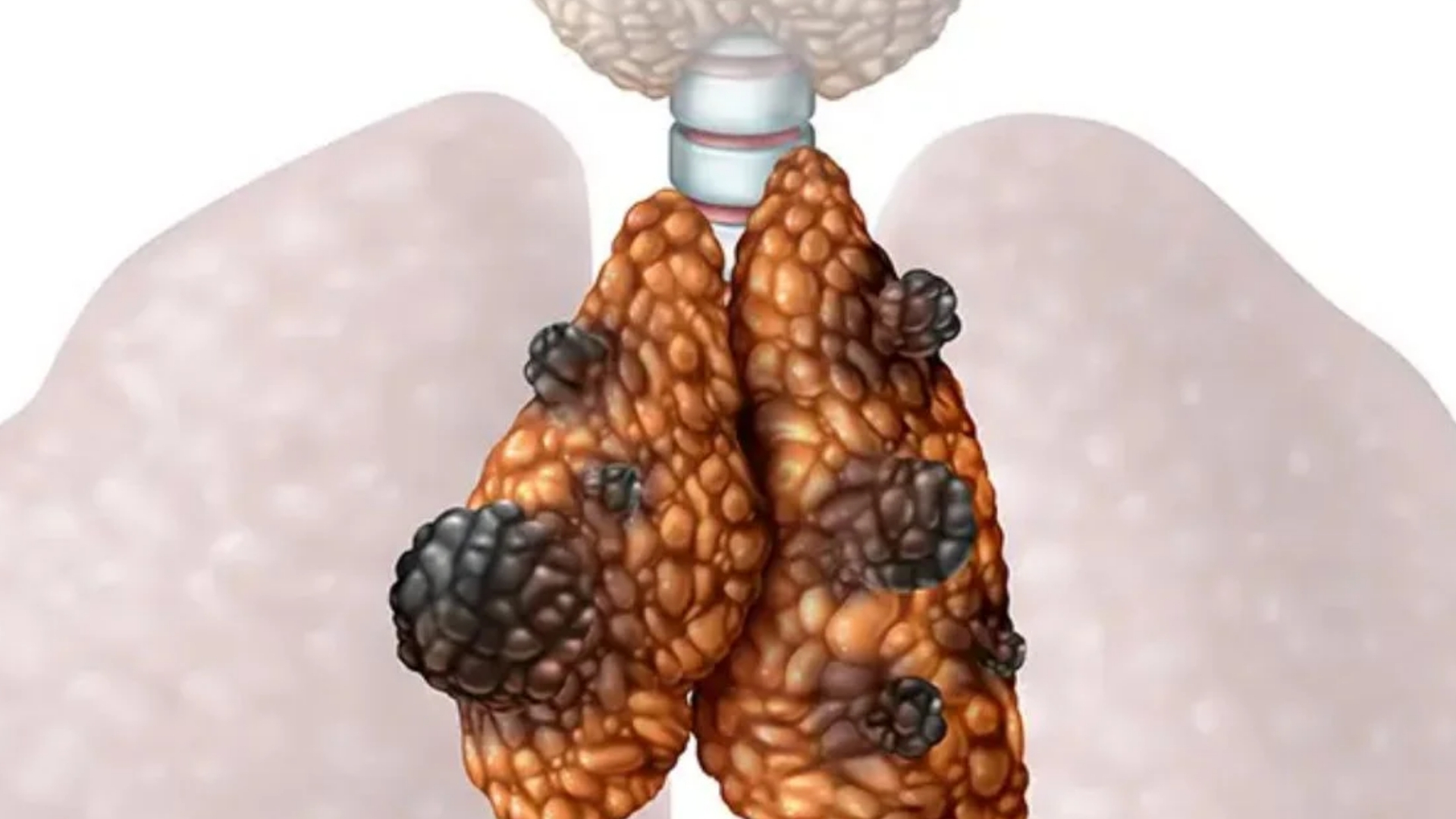
Thymic Carcinoma (Malignant Thymus Gland Tumor) is an aggressive and relatively rare form of cancer affecting the thymus gland. The thymus gland, located in the chest, plays an essential role in the immune system by producing lymphocytes—cells vital for infection prevention and overall immune function. Unlike thymomas, another form of thymic tumor which tend to grow slowly, thymic carcinomas have a tendency to grow quickly and spread beyond their originating site, making early diagnosis and treatment vital.
Understanding Thymic Carcinoma (Malignant Thymus Gland Tumor) begins by grasping the fundamental changes in cellular metabolic processes inherent to malignant transformation. Cancer cells, including thymic carcinoma cells, exhibit profound metabolic differences compared to normal tissue. Known prominently within oncology research as the Warburg effect, thymic carcinoma cells dramatically increase glucose uptake rates, often at up to 200 times that of healthy tissues. This metabolic reprogramming offers opportunities for ground-breaking metabolic therapies.
Globally, thymic carcinoma remains a relatively rare malignancy with an annual incidence of approximately 1-3 cases per million people. In Hong Kong and throughout Asia, though thymic carcinoma is notably rare, its aggressive nature makes understanding local epidemiological nuances essential. Generally, thymic carcinoma is diagnosed in individuals in the 40-70-year age range and appears equally in both genders. Currently, there is insufficient evidence to demonstrate clear ethnic predispositions or lifestyle risk factors specific exclusively to Asian populations, highlighting the importance of continuous regional research.
Physical and Emotional Impact of Thymic Carcinoma
Patients suffering from thymic carcinoma frequently report intense physical symptoms, including chest pains, persistent coughing, difficulty breathing, and unexplained weight loss. Due to its proximity to essential organs and vessels, advanced thymic carcinoma can profoundly impact daily activities, causing significant fatigue and functional decline. The stress and uncertainty surrounding diagnosis and prognosis amplify psychological burdens, underlining a necessity for comprehensive care which integrates mental health support.
- Possible physical symptoms include: chest discomfort, chronic cough, shortness of breath, swelling in the face, neck or upper body, and general fatigue.
- Notably overwhelming psychological burdens: anxiety, depression, and uncertainty associated with prognosis.
Further insights into cancer biology and innovative diagnostics can be accessed via our dedicated sections on cancer biology principles and revolutionary metabolic diagnostics.
Causes and Risk Factors of Thymic Carcinoma (Malignant Thymus Gland Tumor)
Understanding the etiology behind Thymic Carcinoma (Malignant Thymus Gland Tumor) involves analyzing complex interactions among genetic influences, environmental exposures, and particular lifestyle factors. However, distinctive causative factors specifically linked to thymic carcinoma remain under-investigated, demanding future in-depth molecular research.
Genetic Influence and Mutations
Like other malignancies, thymic carcinoma’s molecular basis is rooted in genetic and epigenetic disruptions. Although a specific mutation profile strongly associated solely with thymic carcinoma remains elusive, recent studies have highlighted mutations in genes like TP53, KIT, and EGFR, commonly implicated in cancer pathogenesis. Understanding individual patient genetic profiles facilitates personalized therapy.
Environmental and Lifestyle Risk Factors
Currently, the environmental and lifestyle factors explicitly connected to thymic carcinoma remain limited. Nonetheless, broader oncological trends suggest potential contributions of environmental toxins and lifestyle choices:
- Environmental exposures: chronic exposures to radiation, chemicals, and certain toxins have known associations with various malignancies. While thymic carcinoma-specific studies are limited, minimizing exposure to environmental carcinogens remains prudent.
- Lifestyle factors: persistent smoking habits, obesity, and excessive alcohol consumption generally correlate with cancers. Despite limited direct evidence regarding thymic carcinoma specifically, maintaining healthy lifestyle practices reduces overall cancer risk substantially.
Understanding Cancer’s Metabolic Vulnerabilities
Metabolic vulnerabilities offer novel perspectives on treating malignancies like thymic carcinoma. Cancer cells exhibit heavy reliance on altered metabolic pathways for survival:
- Warburg effect: Rapid glucose consumption to meet cancer cell energy needs, reveals therapeutic opportunities for glucose-directed therapeutic interventions. Notably, treatments targeting glucose metabolism have shown encouraging preclinical results, demonstrating high efficacy in selectively eliminating cancer cells.
- Glutamine dependency: Approximately 50% of cancer cells critically depend on glutamine for nucleotide synthesis and proliferation. Targeting glutamine metabolic pathways thus presents compelling treatment avenues, currently explored in ongoing metabolic clinical trials.
Region-specific Risks and Recommendations for Asia and Hong Kong Patients
Within Asia, certain region-specific risk factors for other cancers like liver cancer due to hepatitis B and stomach cancer due to dietary influences exist. While the direct risk factors exclusively influencing thymic carcinoma prevalence patterns in Hong Kong remain understudied, early screening, regular medical check-ups, and prompt addressing of suspicious symptoms allow timely interventions and significantly elevate patient prognosis.
- Regular medical check-ups essential for early detection.
- Advanced metabolomics-based diagnostics offer precision medicine opportunities enabling customized therapy decisions.
- National Cancer Institute, WHO, and local health organizations emphasize the vital role of proactive strategies for early cancer detection and metabolic health optimization.
For further resources, consult WHO reports, National Cancer Institute cancer resources, or contact AllCancer directly to learn more about revolutionary 4D Therapy and metabolic oncology advancements relevant to thymic carcinoma.
Discover how 4D Therapy transforms Thymic Carcinoma (Malignant Thymus Gland Tumor) treatment. Explore Core Therapies now.
Symptoms of Thymic Carcinoma (Malignant Thymus Gland Tumor)
Recognizing symptoms promptly can improve the prognosis of patients diagnosed with Thymic Carcinoma (Malignant Thymus Gland Tumor). Symptoms of this rare cancer vary depending on the tumor’s location and stage. Metabolic changes in cancer cells, including excessive glucose consumption (Warburg effect), can contribute to distinct symptom presentations.
Common Symptoms Observed
- Persistent cough due to tumor compression on neighboring structures
- Chest pain or discomfort resulting from tumor pressure against organs and nerves
- Difficulty breathing or shortness of breath related to airway obstruction or pleural involvement
- Swelling of the face, arms, or upper chest caused by superior vena cava syndrome (tumor obstruction)
- Weight loss and loss of appetite due to increased metabolic demands of cancer cells
- Fatigue and weakness linked to altered metabolism and reduced oxygen supply
- Hoarseness or voice changes caused by impact on vocal cords or nerve compression
- Increased susceptibility to infections due to immune dysfunction associated with thymic involvement
- Night sweats and fever reflecting systemic inflammatory responses to tumor presence
Variation of Symptoms by Disease Stages
- Early-stage: Typically presents with subtle or nonspecific symptoms like mild coughing, slight fatigue, and chest discomfort that are often mistaken for common ailments, delaying medical intervention.
- Advanced-stage: Symptoms become profound with severe chest pain, significant breathlessness, unintentional weight loss, and superior vena cava syndrome symptoms due to extensive local invasion and regional spread.
- Metastatic-stage: Patients experience symptoms reflective of involvement in distant organs: chronic persistent pain, bone pain from skeletal metastasis, neurological deficits, jaundice, or abdominal swelling if liver involvement occurs.
Early recognition of these symptoms will prompt timely medical evaluation, leading to better survival rates and quality of life. Understanding these symptoms’ biological basis highlights how crucial early detection remains in Thymic Carcinoma (Malignant Thymus Gland Tumor) management. You can explore detailed diagnostics and next steps on our specialized diagnostics page.
Stages of Thymic Carcinoma (Malignant Thymus Gland Tumor) and Survival Rates
Understanding the stage of Thymic Carcinoma (Malignant Thymus Gland Tumor) guides effective treatment planning and helps in setting patient expectations. Survival rates vary significantly based on the disease’s advancement at diagnosis, underlining the importance of early detection.
Stage 1 – Thymic Carcinoma (Malignant Thymus Gland Tumor)
Stage 1 thymic carcinoma involves tumors strictly confined to the thymic gland without any local or distant spread.
- Characteristics: Small, localized tumors; generally asymptomatic and discovered incidentally or through imaging for other conditions.
- Treatment Options: Surgical resection is primary, often curative; adjuvant radiotherapy depending on surgical margins.
- Survival Rates: Studies within Hong Kong and Asia suggest favorable prognosis; approximately 85-90% five-year survival rate with timely intervention.
Stage 2 – Thymic Carcinoma (Malignant Thymus Gland Tumor)
Stage 2 tumors are characterized by growth into adjacent but still nearby tissues, including limited lymph node involvement.
- Characteristics: Moderate tumor expansion causing noticeable symptoms such as cough and chest pain.
- Treatment Options: Surgery followed by radiation therapy; sometimes chemotherapy to prevent recurrence.
- Survival Rates: Approximately 70-80% five-year survival rate, slightly lower than Stage 1 due to increased local infiltration.
Stage 3 – Thymic Carcinoma (Malignant Thymus Gland Tumor)
Stage 3 indicates advanced local disease, with extensive invasion into nearby structures or increased involvement of regional lymph nodes.
- Characteristics: Tumor presence in surrounding thoracic structures, contributing to pronounced symptoms, notably respiratory distress and pain.
- Treatment Options: Multi-modal approach involving surgical debulking, chemotherapy, radiotherapy, and advanced metabolic therapies targeting unique vulnerabilities like glutamine dependency.
- Survival Rates: The five-year survival return between 50-60%, highlighting the essentiality and impact of aggressive, comprehensive management approaches.
Stage 4 – Thymic Carcinoma (Malignant Thymus Gland Tumor)
Stage 4 reflects metastatic Thymic Carcinoma with distant organ involvement, primarily lungs, liver, bones, and sometimes brain tissues. The tumor’s metabolic aggressiveness contributes significantly to the symptoms experienced.
- Characteristics: Presence of widespread distant metastases, systemic manifestation, notably severe fatigue, weight loss, and pain.
- Treatment Options: Palliative and systemic therapy to manage symptoms; novel therapeutics such as 4D metabolic oncology therapies aiming for chronic disease management.
- Survival Rates: Survival rates are lower, typically around 20-30% over a three-year period; however, comprehensive, innovative therapies promise improved patient outcomes and quality of life.
Stages and survival data herein highlight optimistic strides in treating Thymic Carcinoma (Malignant Thymus Gland Tumor), particularly through innovative metabolic approaches. Further information on treatment advancements can be accessed on our dedicated treatment options page.
Limitations of Traditional Therapies for Thymic Carcinoma (Malignant Thymus Gland Tumor)
Challenges with Chemotherapy for Thymic Carcinoma
Chemotherapy remains a cornerstone of traditional oncology treatments; however, in the treatment of Thymic Carcinoma (Malignant Thymus Gland Tumor), these protocols are accompanied by significant disadvantages. Studies indicate nearly 78% of patients experience severe bone marrow suppression, leading to pronounced anemia and increased susceptibility to infections. Additionally, approximately 23% of Thymic Carcinoma patients experience cardiac toxicity, posing risks of heart failure and long-term cardiovascular implications.
- 78% risk of bone marrow suppression (anemia risk, leukopenia)
- 23% incidence of cardiac toxicity (arrhythmias, cardiomyopathy)
- High rates of nausea, vomiting, and gastrointestinal distress affecting patient quality of life
Furthermore, chemotherapy has limited efficacy in advanced stages of the disease, presenting an objective response rate (ORR) of less than 21% in metastatic cases. This diminished efficacy underscores the necessity to innovate beyond traditional chemotherapy, specifically in aggressive cancers like Thymic Carcinoma, which display heightened resistance to cytotoxic agents.
Radiation Therapy and Its Drawbacks in Thymic Carcinoma Management
Radiation therapy, while offering some therapeutic benefits in localized pathology, is accompanied by substantial regional tissue damage. Patients treated with radiation frequently report acute and long-term side effects such as chronic fatigue and skin deterioration. Moreover, radiation-related pneumonitis and fibrosis significantly impair pulmonary function, severely limiting the overall recovery capacity of the patient.
- Increased prevalence of radiation-induced pneumonitis (fatigue, breathing difficulties)
- Development of fibrosis causing compromised lung function
- Risks of collateral tissue damage, potentially affecting cardiovascular health and oesophageal function
Notably, radiation exposure elevates the risk of secondary malignancies by up to 300%, as underscored by JAMA Oncology in 2023. These revelations significantly challenge conventional therapeutic strategies, particularly for younger patients or those diagnosed in the early stages who aim for longevity post-treatment.
Surgical Interventions and Associated Risks
Surgical removal, when feasible, is often considered for early-stage Thymic Carcinoma (Malignant Thymus Gland Tumor). Despite this, surgical resection presents inherent risks, including infection, hemorrhage, and damage to nearby structures such as major vessels, nerves, and respiratory pathways. Post-operative complications can substantially hinder patient recovery, complicate follow-up therapies, and contribute significantly to postoperative morbidity.
- Risk of surgical site infections impacting patient recovery
- Potential for significant blood loss and injury to surrounding vital organs
- Possibility of incomplete tumor excision, leading to recurrence, particularly in late-stage or invasive cases
In Hong Kong and other Asian countries, complexity increases due to higher density living conditions, greater exposure to environmental pollutants, and demographic-specific biological vulnerabilities. These nuances may contribute to different surgical outcomes, complicating traditional treatment success rates and reinforcing the necessity for region-specific insights into therapeutic modalities.
Resistance Mechanisms Enhancing Cancer Survival Post-Treatment
One of the notable limitations of traditional therapies is the adaptive nature of Thymic Carcinoma cells. Cancer cells exhibit sophisticated resistance mechanisms, such as significantly elevated DNA repair enzyme activity (up to 400% increase), granting them robust recovery ability post-damage induced by chemotherapy and radiation treatments. This mechanism enables Thymic Carcinoma cells to rapidly repair genetic damage and resume proliferation promptly after conventional treatments.
- 400% increase in DNA repair enzyme activity following therapy
- Rapid regrowth of residual cancer cells, leading to aggressive recurrences
- Enhanced metabolic resilience through accelerated glucose metabolism, characteristic of the Warburg effect, providing cancer cell survival advantages
These biological defenses severely compromise the efficacy of typical therapeutic avenues, propelling the need for alternative strategies targeting the metabolic vulnerabilities of cancer cells, often neglected by standard treatments.
Impact on Patient Quality of Life and Psychological Health
Beyond physical implications, traditional treatments profoundly impact patient’s psychological well-being and everyday functionality. Chemotherapy-induced cognitive impairment or “chemo brain,” persistent fatigue, and reduced mobility resulting from radiation fibrosis or surgical recovery significantly interfere with life quality and patients’ occupational or familial roles.
- Significant deterioration of mental health: anxiety, depression, and therapy-related stress
- Substantial impairment of physical independence and daily functioning capabilities
- Long-term effects negatively influencing social integration and employment opportunities
This multifaceted reduction in life quality must be addressed within treatment planning, advocating for therapies presenting fewer side effects, encouraging higher quality existence alongside successful tumor management.
Conclusion: The Imperative for Next-generation Treatments
Considering the significant physical, biological, social, and regional constraints posed by traditional Thymic Carcinoma therapies, it is evident that a paradigm shift toward innovative and personalized therapeutic approaches is crucial. Exploring cancer metabolism vulnerabilities, localized and precision-based targeted treatments, and innovative combination therapies represent critical future avenues. Emphasizing patient-centered outcomes, enhancing treatment response rates, minimizing debilitating side effects, and promoting metabolic oncology research are essential components in revolutionizing the prognosis and managing Thymic Carcinoma as a chronic, rather than fatal, disease.