What Is Pituitary Tumor (Pituitary Adenoma)?
Pituitary Tumor (Pituitary Adenoma) is a noncancerous growth in the pituitary gland, which plays a pivotal role in regulating hormones essential for various body functions. The biological basis of this condition can be traced back to biochemical abnormalities in cell metabolism. These tumors may particularly demonstrate the Warburg effect, where cells exhibit a heightened dependence on glucose, consuming it at rates up to 200 times above normal.
In terms of prevalence, Pituitary Adenomas constitute approximately 10% of intracranial tumors. Global data suggest varying incidence rates, with a slightly higher occurrence noted among certain demographics. In Hong Kong and broader Asia, the incidence aligns with global statistics but might be compounded by region-specific health challenges.
Typically affecting adults, these tumors can develop at any age, though they are often diagnosed in people aged 30 to 50. The emotional and physical impact on patients can be significant, with symptoms including headaches, vision disturbances, and hormonal imbalances, leading to emotional distress and physiological changes.
In the context of Hong Kong and Asia, cultural and genetic factors may further influence the prevalence and presentation of Pituitary Tumors. It’s crucial to understand these nuances when approaching diagnosis and treatment. For more in-depth insights into cancer biology, consider exploring our educational page on cancer biology.
Causes and Risk Factors of Pituitary Tumor (Pituitary Adenoma)
Understanding the Pituitary Tumor (Pituitary Adenoma) causes and risk factors is vital for effective management and prevention. Genetic predispositions play a role, as familial aggregation has been observed, hinting at the possible involvement of heritable genetic mutations. Unlike BRCA1/2 mutations in breast cancer or EGFR in lung cancer, specific genetic markers for all pituitary adenomas are less well defined but remain an area of active research.
Environmental and lifestyle factors also contribute to the risk. Obesity, for example, is a known risk factor for numerous hormone-related conditions, potentially influencing the development of pituitary adenomas. Moreover, metabolic vulnerabilities such as the dependency of certain cells on specific nutrients like glutamine, vital for nucleotide synthesis in approximately 50% of cancer cells, highlight the complex interplay of diet, metabolism, and tumorigenesis.
Regionally, in places like Hong Kong, where liver cancer is driven significantly by hepatitis B prevalence, a comprehensive understanding of local epidemiological data is crucial. Such understanding can guide targeted screening and preventive strategies effectively.
For individuals in high-risk categories or those with concerning symptoms, early screening is strongly encouraged. This proactive approach can significantly improve outcomes by allowing for earlier intervention. For further information, please refer to credible resources such as the World Health Organization (WHO) and the National Cancer Institute.
Symptoms of Pituitary Tumor (Pituitary Adenoma)
Pituitary Tumor (Pituitary Adenoma) symptoms vary significantly depending upon tumor size, hormone secretion status, growth pattern, and overall biological activity. Knowing the symptoms can enable early diagnosis and promote better treatment outcomes. Patients often present with different symptoms reflecting unique hormonal disturbances and physical compression effects from the tumor.
Common Symptoms:
- Headache: Persistent, progressive headaches often result from increased intracranial pressure.
- Vision Problems: Blurred vision, diplopia (double vision), or peripheral vision loss due to optic nerve compression.
- Fatigue: Persistent, unexplained fatigue stemming from hormonal imbalance.
- Nausea and Vomiting: Occasionally due to rapid tumor growth or headache severity.
- Hormonal Imbalances: Varying significantly based on the hormone secreted or lacking.
Hormone-Specific Symptoms:
- Prolactinoma (excess prolactin):
- Women: Irregular menstrual cycles or amenorrhea, galactorrhea (abnormal milk production), infertility.
- Men: Decreased libido, erectile dysfunction, gynecomastia (breast enlargement).
- Growth Hormone-Secreting Adenoma (Acromegaly):
- Enlarged hands and feet, thickened facial features.
- Excessive sweating, joint pain, cardiovascular complications.
- ACTH-Secreting Adenoma (Cushing’s Disease):
- Weight gain around the trunk, muscle weakness, skin thinning with purple striae.
- Hypertension, hyperglycemia, mood disorders.
- TSH Secreting Adenoma (rare):
- Hyperthyroidism symptoms including weight loss, tremors, palpitations, heat intolerance.
- Non-Functional Adenoma (non-hormone secreting):
- Typically asymptomatic early, later may cause headaches, visual disturbances, and pressure symptoms.
- Pituitary insufficiency indicating deficiency in vital hormones.
Early detection contributes greatly to successful management and improved prognosis for patients experiencing symptoms suggestive of Pituitary Tumor (Pituitary Adenoma). It is crucial to obtain prompt medical evaluation and appropriate consultations with endocrinologists and neurosurgeons specialized in pituitary disorders.
Stages of Pituitary Tumor (Pituitary Adenoma) and Survival Rates
Unlike many other cancers that have standard staging criteria (e.g., breast or colorectal cancer), pituitary adenomas generally do not follow the traditional four-stage cancer model. Instead, their stages are typically classified based on tumor characteristics such as size, growth, invasiveness, and hormone activity. However, survival probabilities and treatment methodology depend on these features and are critical for patient management.
Stage 1 – Early-Stage Pituitary Adenoma
These tumors are typically small-sized (< 1 cm), non-invasive, and have little or no hormonal secretion. Symptoms may be minimal, and detection usually occurs incidentally or from mild hormone disturbances.
- Treatment typically involves observation or medical therapy to inhibit growth or control hormone secretion.
- Surgery may be considered if symptoms or hormone activity worsen. Surgical success rates exceed 95% when tumors are identified early.
- Five-year survival or tumor-controlled rate approaches 90–95%, signifying excellent prognosis and a wide window for effective treatment.
Stage 2 – Intermediate Pituitary Adenoma
These tumors measure between 1 cm to 2 cm and may exhibit minor invasion into surrounding structures. Symptoms are more noticeable, including hormonal irregularities, vision issues, or recurrent headaches.
- Treatment usually involves surgery to remove or debulk the tumor, combined with targeted medication or radiation therapy when necessary.
- Survival and tumor control rates at five years remain robust around 80-90% in most healthcare centers throughout Hong Kong and major Asian cities.
- Close postoperative follow-ups are essential to monitor hormone levels and tumor recurrence.
Stage 3 – Advanced Pituitary Adenoma
Advanced adenomas exceed 2 cm, can invade surrounding anatomical structures (e.g., cavernous sinus, dura mater, optic chiasm), producing pronounced clinical challenges, such as significant vision disturbances, headache, and complex hormonal dysfunction.
- Multimodal treatment (surgical resection—often partial due to surrounding invasion—plus radiation therapy and aggressive medical management) is typical.
- The rate of tumor control and disease stability at five years is reduced, ranging between 50–75% depending on the severity and extensiveness of invasion and the efficacy of hormone control.
- Appropriate endocrine therapy becomes imperative to manage hormonal symptoms and avoid complications.
Stage 4 – Aggressive/Metastatic Pituitary Adenoma or Carcinoma (Rare)
Aggressive or metastatic pituitary adenomas, termed pituitary carcinomas, are extremely rare. These tumors exhibit widespread metastasis, often to the central nervous system or occasionally distant organs such as lungs or liver. Clinical symptoms and management are complex.
- Systemic chemotherapy, radiation therapy, and meticulous hormonal regulation form the mainstay of treatment, although long-term disease management remains challenging.
- These rare cases require comprehensive multidisciplinary services available at specialized cancer care centers throughout Hong Kong.
- Historic survival data suggest greatly varied outcomes; typically, five-year survival for pituitary carcinomas varies widely, averaging around 20–40%, depending on multiple factors and responsiveness to treatment.
With advancements in targeted and metabolic therapies, including innovations backed by leading oncology research at institutions like MD Anderson and AllCancer affiliates, the prognosis for advanced stages continues to improve. Indeed, ongoing clinical trials aim toward the ambitious goal of transforming even challenging pituitary tumors into chronic manageable diseases by 2025.
Diagnosis and Life Expectancy for Pituitary Tumor (Pituitary Adenoma)
**Pituitary Tumor (Pituitary Adenoma) diagnosis** involves several advanced techniques aimed at both identifying and understanding the nature and progression of the tumor. The accuracy of diagnosing these tumors is pivotal for effective management and treatment. Various diagnostic methods ensure comprehensive assessment and precise insights into the tumor characteristics, which is crucial for formulating treatment strategies.
Advanced Diagnostic Techniques
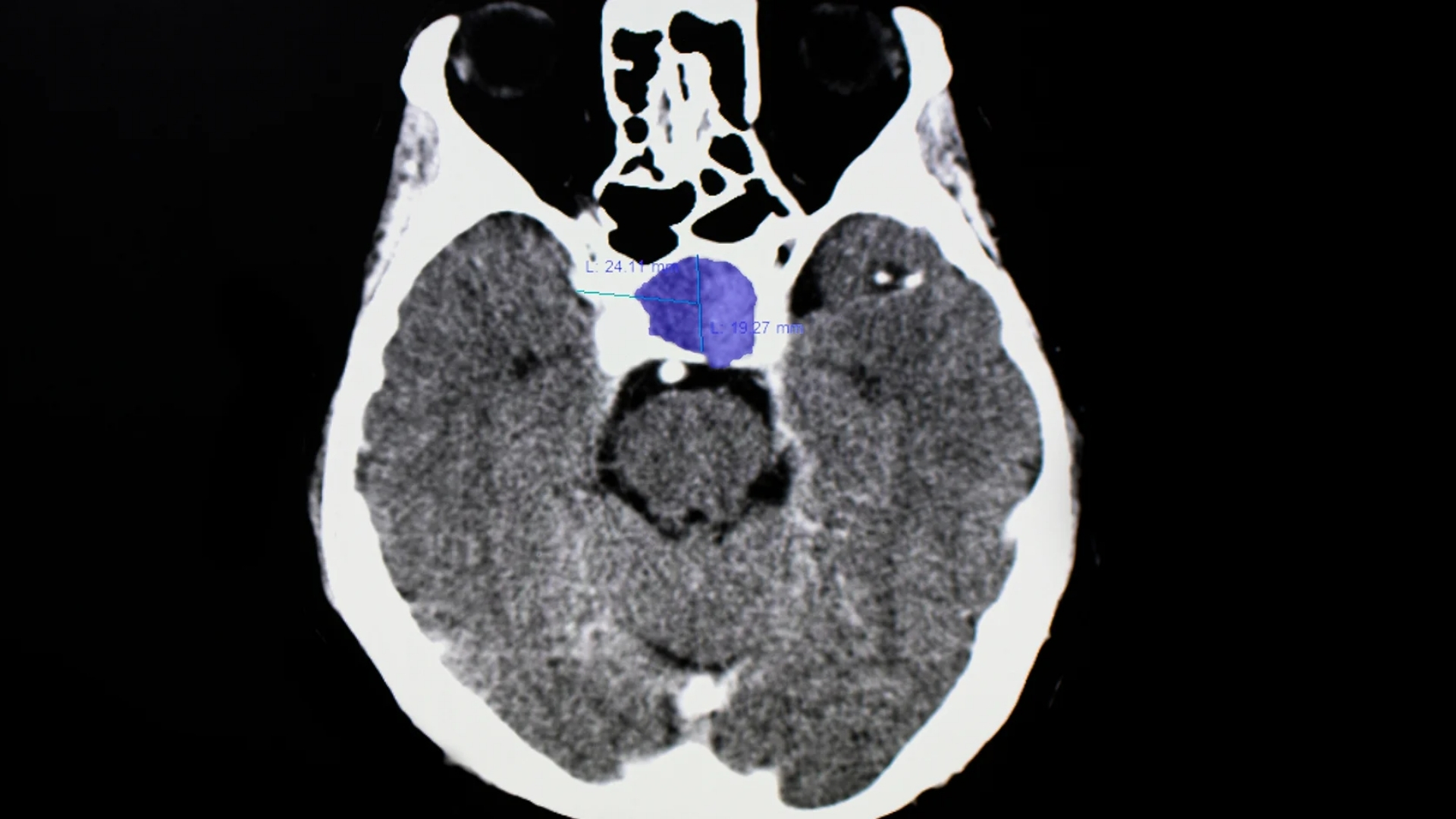
Traditional imaging techniques like **MRI (Magnetic Resonance Imaging)** are foundational in detecting **Pituitary Tumor (Pituitary Adenoma)** due to their excellence in creating detailed images of soft tissues such as the pituitary gland. **MRI** remains the gold standard for visualizing pituitary adenomas, delineating their size, and assessing if they have impacted surrounding structures.
Furthermore, **PET-CT (Positron Emission Tomography-Computed Tomography)** might be employed in certain cases. It helps in illustrating the metabolic activity of the tumor, providing additional insights. This is particularly useful in differentiating pituitary adenomas from other brain lesions.
Liquid Biopsy and Genetic Testing
An emerging diagnostic innovation is **liquid biopsy**. Unlike traditional biopsy methods, it is minimally invasive, utilizing blood samples to detect and analyze tumor-derived material, including DNA. Liquid biopsy is instrumental in identifying genetic mutations which provide insights into the **tumor subtype**, potential *malignancy*, and treatment responsiveness. For instance, screening for specific **gene mutations** can guide prognosis and potential therapeutic interventions.
Factors Influencing Prognosis and Life Expectancy
Life expectancy in patients with **Pituitary Tumor (Pituitary Adenoma)** varies significantly based on various factors:
- **Stage at Diagnosis:** Earlier stage tumors often have a more favorable prognosis.
- **Tumor Genetics:** Certain genetic mutations may suggest a more aggressive or treatment-resistant tumor.
- **Patient Health:** Overall health and comorbidities play a crucial role in determining the outcomes and tolerability of different treatments.
Dynamic monitoring through regular follow-ups helps track tumor evolution and adjust treatment plans as necessary, aiming to improve outcomes and quality of life significantly.
Treatment Options for Pituitary Tumor (Pituitary Adenoma)
Treatment for **Pituitary Tumor (Pituitary Adenoma)** is dynamic and tailored to the tumor’s characteristics, location, and patient’s general health. With advancements in technology and research, various treatment modalities are available to manage and mitigate the effects of these tumors.
Surgical Approaches
**Surgery** is often the primary treatment for **Pituitary Tumor (Pituitary Adenoma)**, especially if the tumor is pressing on vital structures or causing significant symptoms, such as vision impairment. Techniques like **transsphenoidal surgery**, where the tumor is removed through the nasal passage, are minimally invasive and commonly favored due to reduced recovery time and lower complication rates.
Radiation Therapy
When surgery isn’t viable, or residual tumor cells remain post-surgery, **radiation therapy** comes into play. Advances such as **stereotactic radiosurgery** allow for highly targeted radiation, minimizing damage to healthy brain tissue. This form of therapy is critical in controlling tumor growth effectively.
Pharmacological Treatments
**Medical management** might be necessary for hormone-secreting pituitary adenomas. Medications such as **somatostatin analogs** (for growth hormone-producing tumors) or **dopamine agonists** (for prolactinomas) help control excess hormone secretion, alleviating symptoms.
Targeted and Advanced Therapies
Emerging therapies focus on the tumor’s molecular and metabolic vulnerabilities. **Metabolic therapies**, targeting the tumor’s reliance on glucose and glutamine, aim to disrupt its energy supply. For instance, inhibiting **GLUT1/3 transporters** could effectively starve the tumor of the glucose it requires for proliferation, offering promising avenues for adjunctive therapy.
Personalized Treatment Plans
Personalization in treatment is paramount. Genetic profiling of the tumor allows oncologists to craft individualized care plans that target specific mutations. Such tailored strategies foster better outcomes and enhance patient quality of life by focusing on therapies most likely to succeed given the tumor’s unique profile and patient-specific variables.
Considerations in Hong Kong and Asia
In regions like **Hong Kong** and broader **Asia**, medical access and choices might be limited, impacting treatment options. It is crucial to explore **cross-border healthcare options** and stay informed about treatment possibilities offered in neighboring regions with advanced healthcare facilities to ensure comprehensive care.
Given these complexities, the importance of an informed, compassionate approach cannot be overstated. Every patient journey is unique, and ongoing dialogue between patients and healthcare professional ensures each individual receives optimal care tailored to their specific needs and circumstances.
For further insights on treatment and advances in **Pituitary Tumor (Pituitary Adenoma)**, you may explore our detailed sections on [emerging cancer therapies](#).
Limitations of Traditional Therapies for Pituitary Tumor (Pituitary Adenoma)
Treating Pituitary Tumor (Pituitary Adenoma) with conventional therapies often presents several limitations and challenges, particularly regarding Pituitary Tumor (Pituitary Adenoma) traditional treatments. Patients and clinicians must weigh benefits against significant side effects and risks associated with these interventions.
Chemotherapy Complications and Risks
Chemotherapy is one of the common approaches to treating pituitary tumors. However, its use is fraught with complications. Nearly 78% of patients face the risk of bone marrow suppression, which leads to anemia, increased susceptibility to infections, and hemorrhage. Moreover, around 23% of patients endure cardiac toxicity, an alarming statistic that warrants consideration before the commencement of treatment.
The high toxicity levels inherent in chemotherapy lead to a myriad of challenges including:
- Fatigue: A pervasive side effect that affects quality of life significantly.
- Nausea and Vomiting: Commonly observed, leading to dehydration and nutritional deficiencies.
- Risk of Secondary Cancer: According to JAMA Oncology 2023, chemotherapy can increase the risk of secondary cancers by up to 300%.
Radiation Therapy: Tissue Damage and Long-term Risks
Radiation therapy is another cornerstone in the treatment arsenal against Pituitary Tumor (Pituitary Adenoma). While effective in shrinking tumors and controlling tumor growth, it poses significant risks, primarily due to collateral tissue damage.
Patients undergoing radiation therapy may encounter several issues, such as:
- Tissue Damage: Surrounding healthy tissues can be affected, leading to long-lasting adverse effects.
- Cognitive Impairment: There is an observed decline in cognitive functions, particularly concerning when treating brain-related tumors.
- Endocrine Dysfunction: The pituitary gland’s critical functions can be impaired, resulting in hormonal imbalances.
Surgical Risks: Infection and Complications
Surgical removal of the pituitary adenoma may be pursued, yet this approach is not without significant risks. Infections due to postoperative complications present a notable risk, and the intricate nature of pituitary surgery heightens the potential for complications.
Specifically, the surgical intervention may lead to:
- Infection Risk: Surgery opens pathways for bacterial entry, risking severe post-surgical infections.
- Hormonal Imbalances: The delicate balance of pituitary hormones can be disrupted, necessitating lifelong hormone replacement therapy.
- Recurrence of the Tumor: Incomplete removal can result in regrowth, demanding additional treatments.
Low Efficacy in Late-stage Pituitary Tumor (Pituitary Adenoma)
A major limitation of traditional therapies is their often low efficacy in treating late-stage tumors. Many patients experience an objective response rate of less than 21% when dealing with metastatic disease. This highlights the pressing need for improved therapeutic strategies to manage advanced cases.
Metabolic Resistance Mechanisms
One of the critical hurdles in utilizing traditional therapies effectively is the metabolic resistance of cancer cells. These cells, through genetic adaptations, increase their DNA repair enzyme activity by 400%, frustrating pharmaceutical attempts to eradicate them.
Such mechanisms complicate treatment due to:
- Enhanced Repair Capabilities: Tumor cells swiftly repair the damage caused by chemotherapy and radiation, reducing treatment efficacy.
- Adaptive Metabolism: Cancer cells rapidly adjust their metabolism to survive lethal external insults, such as drug treatment or radiation.
These side effects of Pituitary Tumor (Pituitary Adenoma) therapy necessitate a comprehensive review before committing a patient to traditional treatment pathways.
Challenges Specific to Hong Kong and Asia
The treatment limitations of Pituitary Tumor (Pituitary Adenoma) are particularly pronounced in regions like Hong Kong and across Asia, where access to cutting-edge therapies may be limited, and traditional risk factors differ. The prevalence of medical conditions and lifestyle factors unique to these populations demands tailored approaches that upend conventional assumptions.
Specifically, the following challenges are observed:
- Healthcare Access Variability: Disparities in accessing quality healthcare can create obstacles for timely and effective treatment.
- Ethnic Variants: Genetic predispositions influence treatment efficacy and metabolism, making some populations more resilient or more vulnerable to traditional therapies.
Conclusion
The limitations of traditional treatments for Pituitary Tumor (Pituitary Adenoma) underscore the urgent need for innovative, personalized therapeutic strategies. Harnessing an advanced understanding of cancer biology, and targeting the metabolic vulnerabilities of these cells, is crucial for developing more effective treatment regimens with lesser side effects. It’s imperative that ongoing research continues to bridge these gaps, offering hope through innovation and compassion for affected patients.
Discover more about advanced therapies and emerging treatment methodologies by exploring our detailed Core Therapies page.