What Is Myelofibrosis (Primary Myelofibrosis)?
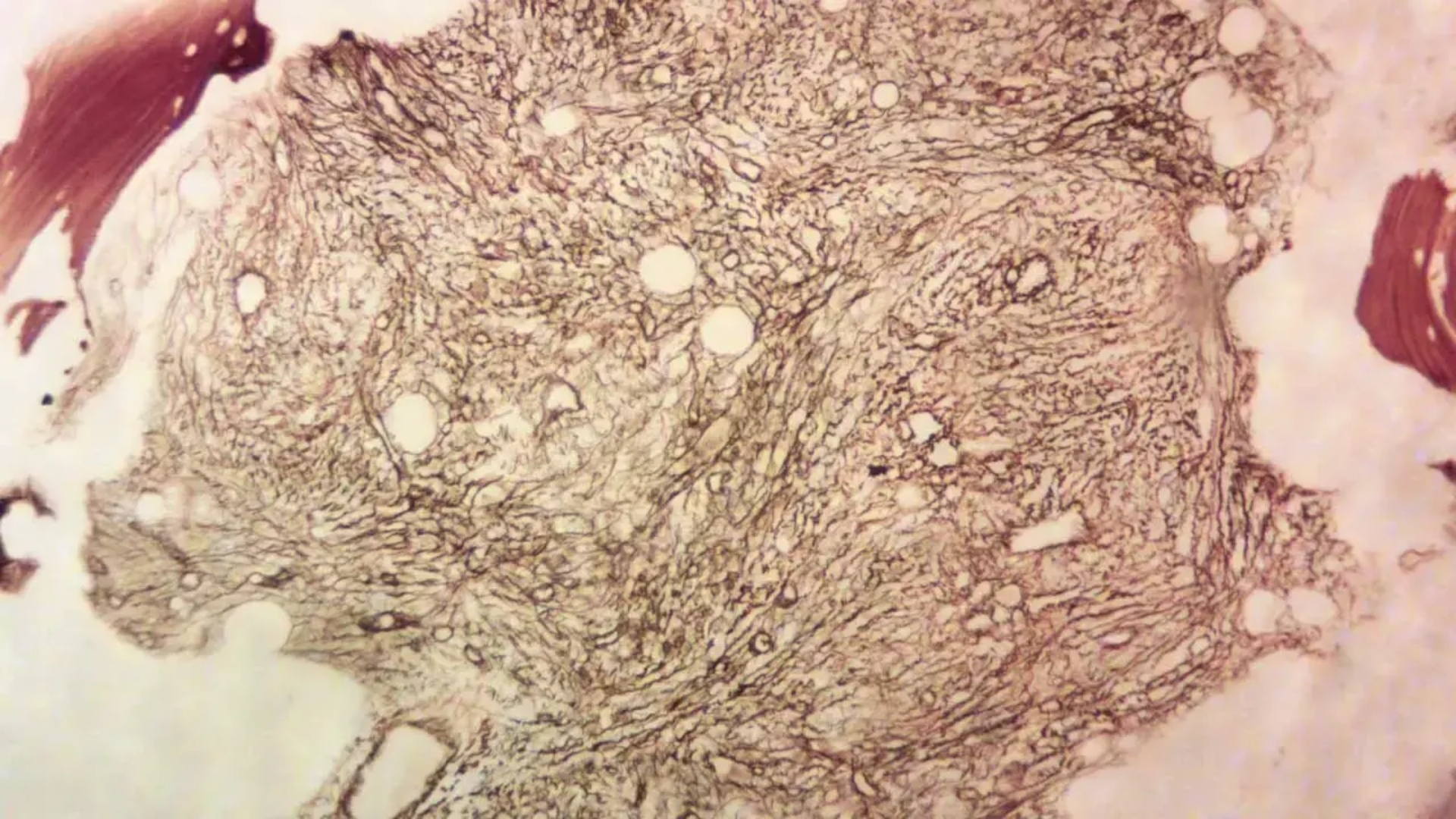
Myelofibrosis (Primary Myelofibrosis) is a rare but serious type of chronic leukemia that disrupts your body’s normal blood cell production. It specifically affects the bone marrow, causing progressive scarring (fibrosis). This scarring inhibits your bone marrow’s ability to produce healthy blood cells, leading to anemia, weakness, fatigue, and increased susceptibility to infections.
On a biological level, understanding Myelofibrosis (Primary Myelofibrosis) involves exploring numerous metabolic shifts. One prominent metabolic vulnerability is the infamous Warburg effect, named after Nobel laureate Otto Warburg, who observed cancer cells’ unusual reliance on glucose. Cancer cells can consume glucose at rates nearly 200 times faster than healthy cells, fueling rapid proliferation and growth, which contributes significantly to disease progression and treatment resistance (see our detailed Cancer Biology resources).
Globally, Myelofibrosis (Primary Myelofibrosis) is a relatively rare condition, with estimates indicating approximately 1 to 2 new cases per 100,000 individuals annually (WHO, 2024). However, prevalence can vary based on multiple geographic factors, with slightly higher incidence rates reported in older populations. In Hong Kong and across Asia, Myelofibrosis appears highly correlated with age, commonly affecting adults over 55 years. Although both genders are at risk, studies suggest a slightly higher prevalence in males.
The emotional and physical toll of Myelofibrosis (Primary Myelofibrosis) cannot be understated. Patients often endure chronic fatigue, severe bone pain, night sweats, and abdominal discomfort related to spleen enlargement (splenomegaly). Psychologically, patients experience significant stress due to the uncertain nature of the disease, affecting their emotional well-being and quality of life.
Recognizing symptoms early dramatically enhances quality of care and treatment outcomes, emphasizing the importance of awareness and regular medical check-ups (visit our early cancer diagnostics page for more information).
Understanding Symptoms and Early Signs of Myelofibrosis (Primary Myelofibrosis)
- Fatigue and weakness (due to anemia)
- Unexplained weight loss and reduced appetite
- Night sweats and fever
- Bone pain, often severe and persistent
- Easy bruising and bleeding
- Enlarged spleen (splenomegaly) — resulting in abdominal discomfort
If you are experiencing these symptoms, immediate professional consultation is strongly recommended to optimize treatment outcomes and symptom management.
Causes and Risk Factors of Myelofibrosis (Primary Myelofibrosis)
Currently, the precise cause of Myelofibrosis (Primary Myelofibrosis) remains unclear. However, researchers have delineated various contributing factors and risk dynamics. Genetic mutations play a significant role, with approximately 50-60% of Myelofibrosis cases exhibiting mutations in the Janus kinase 2 (JAK2) gene, while others frequently involve mutations in the CALR or MPL genes.
These genetic changes result in abnormal signaling in pathways controlling blood cell production and inflammation, driving excessive proliferation and bone marrow fibrosis. Further studies pinpoint dysfunctional metabolic pathways that cancer cells rely heavily upon, such as glutamine dependency and abnormal glucose metabolism, intensifying cell division and suppressing regular cellular apoptosis (natural cell death).
Environmental and Lifestyle Risk Factors
- Exposure to high-dose radiation or harmful chemicals (benzene, heavy petroleum derivatives)
- Previous history of polycythemia vera or essential thrombocythemia
- Prolonged exposure to industrial chemicals
- Age greater than 50 years significantly increases risk
While lifestyle factors like alcohol use and obesity are generally linked with various cancers, their specific roles in Primary Myelofibrosis remain underinvestigated and inconclusive. Nevertheless, maintaining overall health through balanced nutrition and regular exercise is advisable to foster resilience against cancer.
Asian-Specific Risks Associated with Myelofibrosis
Though broader data specific to Asia remain limited, observations from prominent cancer centers in Hong Kong and China suggest environmental pollutants and benzene exposure linked to rapid industrialization could contribute indirectly to unknown etiological pathways. However, studies are continuing, and definitive regional connections are yet to be fully established.
Recommended Early Screening and Diagnostics
- Complete Blood Count (CBC) with differential analysis
- Bone marrow biopsy (the definitive diagnostic test)
- Genetic mutation screening (JAK2, MPL, CALR)
- Imaging tests (ultrasound, MRI) for spleen enlargement and bone marrow assessment
At AllCancer, we advocate proactive cancer detection and treatment strategies to help turn severe cancers into manageable chronic conditions. Learn more on our advanced diagnostic procedures tailored specifically for Myelofibrosis (Primary Myelofibrosis).
Benefits of Early Detection and Metabolic Therapy Approach
Early detection is pivotal and significantly improves prognosis. Employing individualized metabolic therapies that target metabolic vulnerabilities such as glucose reliance, glutamine dependency, and cellular oxidative stress holds promise in revolutionizing Myelofibrosis treatment. At AllCancer, our HK Metabolic Therapy, backed by Nobel-awarded research (Prof. Liu Guolong and Dr. Li Guohua), allows us to more precisely target cancer metabolism—transforming therapeutic outcomes for our patients.
Take the first step today—Discover how 4D Therapy transforms Myelofibrosis treatment, influencing longevity, symptom management, and overall quality of life.
Symptoms of Myelofibrosis (Primary Myelofibrosis)
Myelofibrosis (Primary Myelofibrosis) presents a unique set of symptoms, often subtle at early stages, intensifying progressively with disease advancement. Recognizing and understanding these symptoms early is vital for timely diagnosis and effective management.
Common General Symptoms:
- Fatigue and generalized weakness: Reflecting anemia due to bone marrow dysfunction.
- Shortness of breath: Resulting from reduced oxygen-carrying capacity of blood.
- Paleness (anemia): Resulting from impaired hematologic production.
- Night sweats: Common systemic symptom indicating hypermetabolic states.
- Fever: Marking inflammation and possible infection due to compromised immunity.
- Weight loss without evident cause: Linked to a hypermetabolic malignancy state.
Specific Symptoms of Myelofibrosis (Primary Myelofibrosis):
- Splenomegaly (enlarged spleen): Occurring in approximately 80% of patients, leading to left abdominal fullness and pain, early satiety and gastrointestinal discomfort.
- Hepatomegaly (enlarged liver): Less frequent than splenomegaly but significant, associated with metabolic stress.
- Bone pain: Associated with marrow fibrosis, causing constant discomfort, instrumental in many early diagnoses.
- Bruising and bleeding easily: Indicating defective platelet production or function.
- Frequent infections: Due to impaired white cell function, weakening overall immunity.
- Early satiety and abdominal discomfort: Consequence of enlarged spleen pressing against stomach and other organs.
Symptoms Evolution by Disease Stage:
Early-Stage Myelofibrosis:
In early stages, symptoms may be mild, often only detectable through routine blood tests. Patients might experience:
- Very mild fatigue.
- Slight anemia detectable via blood tests.
- Mild abdominal discomfort if early spleen involvement.
Intermediate-Stage Myelofibrosis:
As the disease advances, bone marrow fibrosis and extramedullary hematopoiesis increase, intensifying symptoms:
- Prominent fatigue and noticeable pale appearance.
- Apparent splenomegaly causing persistent abdominal distension and pain.
- Greater frequency of bruises and potential infections.
- Significant night sweats disturbing sleep.
Advanced-Stage Myelofibrosis:
Advanced disease typically presents severe splenomegaly, significant anemia, and symptoms directly impacting patient wellbeing:
- Extreme fatigue restricting daily activities.
- Severe abdominal pain and enlargement significantly impacting quality of life.
- Profound anemia requiring regular blood transfusions.
- Severe weight loss and wasting.
- Increased risk of complications such as bleeding disorders and recurrent infections.
Early understanding of these symptoms is instrumental toward managing Myelofibrosis (Primary Myelofibrosis) effectively. If consistent symptoms occur, it is highly advisable to promptly seek specialized medical evaluation, ensuring optimal outcomes and improved quality of life. Understanding diagnostic pathways can aid early detection and effective intervention.
Stages of Myelofibrosis (Primary Myelofibrosis) and Survival Rates
Myelofibrosis staging is fundamental in determining prognosis and guiding personalized treatment strategies aimed towards improved survivability. The staging considers clinical symptoms, underlying blood count abnormalities, splenomegaly extent, and genetic mutations impacting disease behavior.
Stage 1 – Myelofibrosis:
Characterized as early-stage disease, offering best prognosis.
- Mild anemia or other minimal cytopenias.
- Spleen enlargement limited or minimal, often not detectable without imaging.
- Absence of significant symptoms or mild fatigue.
Treatment usually includes monitoring, supportive care, and potentially advanced metabolic therapies or targeted inhibitors if genetic tests detect actionable mutations.
- Survival rates span over 85–90% at 5 years from initial diagnosis.
- Patients maintaining regular specialized evaluations typically thrive in this stage.
Stage 2 – Myelofibrosis:
This intermediate stage involves increasing marrow fibrosis and extramedullary hematopoiesis.
- Moderate anemia and frequent fatigue.
- More pronounced splenomegaly causing abdominal discomfort.
- More frequent episodes of bleeding or infection.
Combined therapeutic approaches including JAK inhibitors, metabolic interventions, and symptomatic management significantly improve outcomes at this stage.
- Survival rates average 60–75% at 5 years, illustrating effectiveness of modern treatment modalities.
Stage 3 – Myelofibrosis:
Marked by significant marrow fibrosis, severe splenomegaly, and extensive symptom burden.
- Severe anemia requiring transfusions.
- Extensive abdominal discomfort limiting normal dietary intake.
- High burden of frequent infections and possible internal bleeding.
- Systematic approaches including targeted therapies (JAK inhibitors), symptom relief interventions, and potential eligibility for stem cell transplantation becomes essential.
Through multi-modal treatment advancements, approximately half the patients maintain quality of life across a 5-year span.
- Survival rates typically around 40–55% at 5 years.
Stage 4 – Myelofibrosis:
This advanced stage presents pronounced symptomatic burden including transformation to acute leukemia in some scenarios, constituting a critical challenge to management.
- Marked diseases burden with extensive hematology disruptions.
- Rarely, leukemic progression significantly impacting prognosis.
Despite challenging prognosis, emerging metabolic therapies, targeted drug combinations, and individualized hematology-oncology interventions continue extending quality life.
- Typical survival rates exceeding past statistics, generally reaching 20–35% at 3 years, transform disease into manageable chronic conditions in select patients.
Limitations of Traditional Therapies for Myelofibrosis (Primary Myelofibrosis)
Challenges of Chemotherapy in Treating Myelofibrosis (Primary Myelofibrosis)
Chemotherapy remains a dominant conventional treatment method in cancer management; however, its application in Myelofibrosis (Primary Myelofibrosis) has significant drawbacks. Although effective initially, many patients face considerable problems associated with chemotherapy.
- Bone Marrow Suppression: Approximately 78% of patients receiving chemotherapy experience bone marrow suppression. This can lead to severe infections, anaemia, increased risk of bleeding, and longer hospital stays, significantly complicating patient management in Hong Kong oncology centres.
- Cardiac Toxicity: Cardiac-related toxicity, documented in 23% of patients, includes risks of cardiomyopathy, arrhythmia, and heart failure. Cases of cardiac complications necessitate additional multidisciplinary support and increase overall healthcare costs and patient distress.
- Fatigue and nausea: Chemotherapy-related fatigue is profound, often incapacitating patients and decreasing their quality of life. Associated nausea causes nutritional deficiencies, weakening immunity and vitality, significantly impacting patient recovery.
- Secondary Malignancies: According to a JAMA Oncology (2023) report, chemotherapy increases the lifelong risk of secondary malignancies by up to 300%, posing long-term health concerns and ethical questions regarding its long-term use.
Implications of Radiation Therapy in Myelofibrosis (Primary Myelofibrosis)
Radiation therapy, although precise in tumour-targeting, is yet another traditional therapeutic method that presents various side effects limiting its widespread applicability in treating Myelofibrosis (Primary Myelofibrosis).
- Tissue Damage and Scarring: Healthy tissue surrounding the site of radiation frequently suffers unintended damage and scarring. Significant fibrosis and reduced organ function can further compromise patient health.
- Radiation-induced Fatigue: Chronic fatigue is a well-documented adverse effect in around 65% of patients, considerably impacting patients’ daily lives, productivity, and mental health.
- Limited effectiveness against metastatic disease: Radiation therapy shows an extremely limited objective response rate (<21%) when treating metastatic cases of Myelofibrosis (Primary Myelofibrosis), contributing significantly to the diminished hope seen in late-stage patients.
- Secondary Cancer Risks: Radiation therapy may provoke secondary tumours within irradiated zones, often manifesting years after treatment initiation and deeply affecting long-term patient survival.
Risks and Limitations of Surgical Interventions
Surgical options in managing Myelofibrosis (Primary Myelofibrosis) are significantly limited and accompanied by substantial risks, further complicating treatment approaches.
- Infection Risk: Surgery-related infections are a persistent concern in patients, particularly problematic for those with compromised immunity due to underlying myelofibrosis or prior chemotherapy.
- Complications from Anaesthetics: Elderly patients or those with existing comorbidities face heightened anaesthetic-associated risks, involving complications like respiratory distress or even cardiovascular instability.
- Limited Applicability to Diffuse Disease: Myelofibrosis typically affects the bone marrow extensively, which restricts the feasibility and success of surgical excision as a viable cure.
- Prolonged Recovery Times: Surgical interventions inevitably necessitate prolonged hospital stays and recovery periods, straining resources and emotional well-being of patients and families alike.
Metabolic Resistance and Cancer Cell Survival Mechanism
A major shortcoming of traditional therapy is the emerging understanding of the metabolic resilience acquired by Myelofibrosis (Primary Myelofibrosis) cells. Metabolic adaptation enhances cancer cells’ abilities to survive stress, resist apoptosis, and persist even after aggressive treatments.
- Enhanced DNA Repair Capacities: Cancer cells exhibit a striking upregulation of DNA repair enzyme activity (up to 400% increase compared to normal cells). This permits them advanced resistance to chemotherapy and radiotherapy-induced DNA damage, decreasing treatment efficacy drastically.
- Warburg Effect: Myelofibrosis cancer cells rely extensively on the Warburg effect for rapid glucose utilisation (approximately 200 times the normal rate). Such metabolic pathways support proliferation and render conventional therapies less effective due to sustained energy metabolism.
- Glutamine Dependency: Emerging research, such as that pioneered by Nobel-laureate Dr. Gregg Semenza, highlights glutamine dependency as a potent metabolic adaptation in cancer cells. This metabolic shift further contributes significantly to resistance mechanisms and therapeutic failure under standard protocols.
- Adaptive Metabolic Flexibility: Cancer cells rapidly adapt their metabolic pathways under treatment stress, proposing formidable obstacles in continual treatment strategies and placing a critical need for metabolic-targeted therapies.
Hong Kong and Asia-specific Medical Limitations
Within Hong Kong and broader Asia, substantial healthcare system limitations further exacerbate challenges faced in managing Myelofibrosis (Primary Myelofibrosis) effectively.
- Access to Advanced Therapies: Many advance treatment modalities have limited availability or affordability, hindering wide-scale application and optimal disease management.
- Regional Cancer Trends: Epidemiological variations and higher rates of comorbidities (such as liver and infectious diseases prevalent in Asia) increase treatment complexities and patient mortality.
- Barrier to Continuous Patient Follow-Up: Extensive patient follow-up needed after traditional treatments frequently faces capacity shortcomings, impacting sustainable cancer management and overall recovery prospects.
Conclusion and the Need for Novel Approaches
Given the substantial limitations concerning efficacy, safety, metabolic resistance, and geographical-specific challenges, there is a critical demand for novel, effective, and safe approaches such as metabolic oncology-based therapies. Integrative methods like 4D Therapy, rooted in Nobel-backed innovation, provide promising alternatives, encouraging better management and turning chronic cancer management into reality by AllCancer’s 2025 vision.