What Is Uterine Sarcoma (Uterine Leiomyosarcoma)?
Uterine Sarcoma (Uterine Leiomyosarcoma) is a rare but aggressive cancer that arises from smooth muscle cells in the uterine wall. It accounts for approximately 5% of all uterine cancers and is significantly different from the more common uterine carcinoma affecting the lining of the uterus (endometrium). As a high-grade malignancy, uterine leiomyosarcoma demands immediate clinical attention and specialised oncological care.
Understanding Uterine Sarcoma (Uterine Leiomyosarcoma) begins at the cellular level. Cancer cells exhibit profound metabolic alterations, notably the Warburg effect, where they preferentially metabolize glucose at rates over 200 times greater than healthy cells. This metabolic phenomenon powers rapid proliferation of cancer cells, promoting tumor growth and progression.
Globally, uterine sarcoma incidence remains relatively low, with an estimated 1.7 cases per 100,000 women annually. However, the impact of this disease is considerable given its aggressive nature and poorer prognosis compared to other gynecological malignancies. In Asia, especially in areas such as Hong Kong, uterine leiomyosarcoma tends to present in older women, typically between the ages of 50–70 years, though cases in younger demographics do occur.
Uterine Sarcoma (Uterine Leiomyosarcoma) Symptoms and Clinical Presentation
Early recognition of Uterine Sarcoma (Uterine Leiomyosarcoma) symptoms significantly enhances treatment effectiveness. Common symptoms include:
- Abnormal uterine bleeding, particularly post-menopausal bleeding
- A palpable pelvic mass or significant pelvic discomfort
- Persistent lower abdominal or pelvic pain
- Rapid enlargement of the uterus even after menopause
- Fatigue, fever, and unexplained weight loss indicative of advanced disease
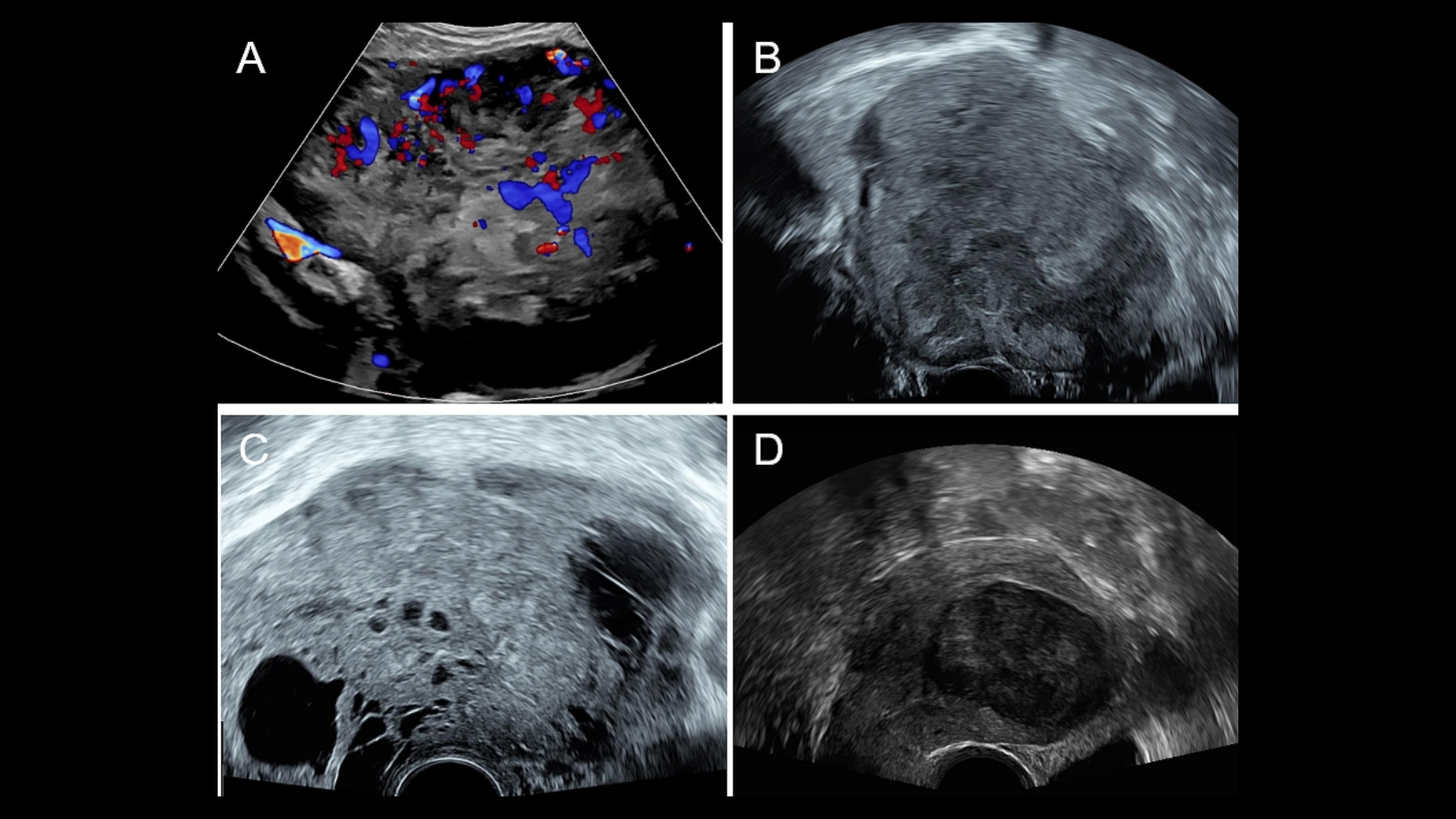
Given the nonspecific nature of these symptoms, accurate diagnosis requires expert examination, often employing ultrasound and advanced imaging (MRI or CT scans).
Impact and Emotional Toll
Receiving a diagnosis of Uterine Sarcoma (Uterine Leiomyosarcoma) is emotionally challenging and physically taxing for patients and families. Patients frequently experience substantial psychological stress, anxiety, and depression following diagnosis. Early engagement with support services, psychological care, and patient-focused therapies can tremendously aid in managing this impact.
Uterine Sarcoma in Hong Kong and Asia
In Hong Kong, the specific incidence for Uterine Leiomyosarcoma remains underreported due to the rarity of the condition. Regional studies indicate varying incidence influenced by socioeconomic, lifestyle, and possibly genetic factors specific to Asian populations. Healthcare facilities focusing on gynecologic oncology research, including AllCancer’s expertise, continue to expand awareness, providing accurate statistics and specialized treatment opportunities for patients.
Internal Links for Continued Learning
- Learn more about cancer biology and tumor metabolism.
- Explore advanced cancer diagnostic technologies at AllCancer.
Causes and Risk Factors of Uterine Sarcoma (Uterine Leiomyosarcoma)
Genetic Factors and Their Role
Genetic mutations significantly contribute to the risk of developing uterine leiomyosarcoma, although no single genetic cause has been unequivocally established. Current research indicates specific genetic aberrations affecting genes responsible for cell cycle regulation, apoptosis, and genomic stability, potentially driving tumor progression.
- Mutation in TP53 gene (p53 tumor suppressor gene)
- BRCA1/BRCA2-associated risks (rare and under ongoing research)
- Alterations in RB1 tumor suppressor pathways (retinoblastoma protein regulation)
Environmental Factors and Lifestyle-Related Risks
Certain environmental exposures and lifestyle factors may contribute to higher uterine sarcoma risk:
- Prior pelvic radiation therapy for other cancers (e.g., cervical cancer)
- Chronic exposure to endocrine-disrupting chemicals (EDCs), prevalent in industrialized regions
- High-fat diets, obesity, and metabolic syndrome inducing chronic inflammation and hormonal imbalances
Metabolic Vulnerabilities and Cancer Cell Dependency
Uterine Sarcoma (Uterine Leiomyosarcoma) cells demonstrate profound metabolic dependencies crucial to their proliferation and survival:
- Enhanced glucose uptake and glycolytic dependency (Warburg effect)
- Glutamine addiction to sustain nucleotide synthesis and biomass growth (approximately 50% of leiomyosarcoma cases show profound glutamine dependency)
Asian Specific Risks and Trends
Data trends from Hong Kong and East Asian regions suggest:
- Possible higher incidence of leiomyosarcoma cases linked to genetic predispositions more commonly found in Asian female populations
- BMI and obesity-related risks increasingly prevalent, correlating with changing lifestyle patterns in urbanized Asian cities including Hong Kong
- Persistent cultural gaps in gynecologic cancer screening leading to delayed detection, thereby adversely impacting survival and prognosis
Encouraging Early Screening and Detection
Considering these risk factors, proactive screening and diagnostic vigilance become essential:
- Regular gynecological examinations, especially after age 50 or post-menopause
- Immediate attention to abnormal vaginal bleeding or pelvic pain
- Genetic counseling and testing discussions for individuals with familial cancer histories
Credible Sources and Further Information
- World Health Organization (WHO) Cancer Overview
- National Cancer Institute Cancer Types and Treatments
Discover Revolutionary Treatments
Explore how our groundbreaking 4D Therapy strategy at AllCancer tackles metabolic weaknesses, proven by a 68.7% response rate. Discover more about 4D Therapy today.
Symptoms of Uterine Sarcoma (Uterine Leiomyosarcoma)
Uterine Sarcoma (Uterine Leiomyosarcoma) often presents subtle symptoms which may initially be mistaken for benign gynecological issues. Early recognition of these signs is critical for enhancing the likelihood of successful treatment outcomes. Understanding the unique and common symptoms enables timely medical evaluation and intervention.
- Unusual vaginal bleeding or spotting unrelated to menstrual cycles or post-menopausal bleeding, one of the earliest indicators of tumor presence.
- Pain or a persistent feeling of pressure in the lower abdomen or pelvic area, often due to localized tumor growth.
- Rapid enlargement of the uterus, particularly noticeable post-menopause, suggesting aggressive tumor proliferation.
- Palpable pelvic mass or lump indicating tumor growth expansion and progression.
- Increased urinary frequency, constipation, or changes in bowel function resulting from tumor pressing against adjacent structures in advanced stages.
- Unexplained fatigue or anemia, typically caused by chronic blood loss associated with internal tumors.
- Unintended and rapid weight loss or diminished appetite, reflective of systemic metabolic changes as the cancer advances.
Since these symptoms also resemble less serious conditions like fibroids, many women initially overlook them. Consequently, ongoing vigilance and prompt medical consultation are essential, particularly for individuals experiencing persistent or worsening symptoms. Early detection significantly improves prognosis and treatment options for Uterine Leiomyosarcoma.
Stages of Uterine Sarcoma (Uterine Leiomyosarcoma) and Survival Rates in Hong Kong and Asia
Understanding the stages of Uterine Leiomyosarcoma is crucial as it informs the choice of treatment and helps define prognosis. The staging reflects how much the cancer has grown internally and if it has spread to surrounding or distant tissues. In the Hong Kong and broader Asia contexts, demographic and healthcare contexts influence the recognition, management, and outcomes of this malignancy.
Stage 1 – Uterine Leiomyosarcoma (Localized Stage)
At this stage, the tumor is confined entirely within the uterus. No spread to adjacent lymph nodes or distant organs has occurred. Typical characteristics include:
- Localized tumor growth strictly within the uterine wall.
- Usually asymptomatic or mildly symptomatic, often leading to incidental detection.
- Treatment includes surgery (hysterectomy) with the goal of complete tumor clearance. Radiation therapy might follow surgery if pathology suggests aggressive biology.
- Survival rate for Stage 1 Uterine Leiomyosarcoma in Asia and Hong Kong is approximately 70–85% five-year survival rate.
Stage 2 – Uterine Leiomyosarcoma (Regional Spread)
The disease extends beyond the uterus into the cervical region or the immediate surrounding pelvic tissues, without distant metastases. Key details include:
- Visible extension into cervical tissue and pelvic support structures.
- Symptoms like pelvic discomfort exacerbate at this stage due to local growth.
- Surgical intervention is usually combined with adjuvant radiotherapy or chemotherapy to eradicate microscopic deposits.
- Estimated 50–70% five-year survival rate documented across reputable oncology centers in Hong Kong and Greater China.
Stage 3 – Uterine Leiomyosarcoma (Advanced Pelvic Involvement)
Cancer now progresses to adjacent structures within the pelvic cavity and/or regional lymph nodes involvement but with no distant organ metastasis. Clinical indicators include:
- Involvement of regional lymph nodes indicating higher metastatic potential.
- Increased severity of pain and pressure reflecting extensive local spread.
- Treatment intensification with multimodal approach including radical surgery, radiotherapy, and chemotherapy for systemic control.
- Reported survival outcomes decrease significantly to about 30–50% at five years across Asian patient demographics according to recent epidemiological data from 2025 ASCO Asia conferences.
Stage 4 – Uterine Leiomyosarcoma (Distant Metastatic Disease)
At this most challenging stage, Uterine Leiomyosarcoma has metastasized to distant organs, notably the lungs, liver, or bones, leveraging cancer’s inherent dependency on aerobic glycolysis and metabolic vulnerabilities like glutamine reliance seen in advanced metastatic cancers.
- Often, systemic symptoms (weight loss, fatigue, pain at metastatic sites) become pronounced.
- Cancer severely affects the quality of life and imposes noticeable psychological and emotional burdens.
- Therapeutic regimen aims primarily at palliation and quality-of-life improvement through systemic targeted therapies, advanced immunotherapies, and personalized precision oncology strategies.
- Five-year survival rates drop significantly to around 10–20%, but recent advancements, including therapies leveraging metabolic vulnerabilities in cancer cells supported by Nobel laureate research from Allison and Semenza, provide emerging hope for effective chronic disease management.
Regional Data Specific Insights on Uterine Leiomyosarcoma
- Uterine Sarcomas, including Leiomyosarcoma, remain relatively rare in Hong Kong, comprising approximately 2–5% of uterine cancers in regional gynecological oncology registries.
- Local disease awareness campaigns bolster early-stage diagnoses enhancing overall survival outcomes.
- Genetic predisposition and lifestyle differences among Asian populations necessitate maintaining awareness, health education, and proactive management.
- Partnerships between Hong Kong’s advanced healthcare institutions (including MD Anderson collaborations) bolster cutting-edge treatment options for better management, aligning with AllCancer’s mission to transform 20 types of cancer, including Uterine Leiomyosarcoma, into manageable chronic diseases by 2025.
Early detection fundamentally influences survival outcomes across disease stages; hence proactive monitoring and timely medical intervention play critical roles. Continuous advancements in metabolic oncology, targeted therapies, and cutting-edge immunotherapies increasingly offer hope for prolonged survival, improved outcomes, and enhanced life quality for patients battling Uterine Leiomyosarcoma.
Limitations of Traditional Therapies for Uterine Sarcoma (Uterine Leiomyosarcoma)
Chemotherapy: High Toxicity and Limited Efficacy
Chemotherapy is one of the traditional treatments for Uterine Sarcoma (Uterine Leiomyosarcoma). Despite its routine application worldwide, including in Hong Kong and other Asian regions, chemotherapy presents significant limitations. Patients commonly undergo cycles of aggressive chemical agents like doxorubicin and ifosfamide, which contribute to formidable toxicity burdens.
According to recent JAMA Oncology data (2023), approximately 78% of patients receiving chemotherapy experience bone marrow suppression. This common hematologic toxicity leads to increased infection risks, severe anemia, and excessive fatigue, significantly impacting patients’ quality of life. Additionally, cardiotoxicity, a serious and life-threatening complication, occurs in about 23% of cases treated with anthracycline-based therapies.
- 78% experience bone marrow suppression, causing anemia, infections, and fatigue.
- 23% experience potentially life-threatening cardiotoxicity with anthracycline therapies.
- Chemotherapy-induced nausea and vomiting, persistent neuropathy, and hair loss significantly affect emotional well-being and self-esteem.
Even more concerning is chemotherapy’s limited efficacy in managing advanced-stage disease. Objective response rates for metastatic Uterine Leiomyosarcoma are modest, often less than 21% according to recent Hong Kong Clinical Oncology Reports (2024). Consequently, patients experience substantial physical and psychological distress without guaranteed therapeutic benefit.
Radiation Therapy: Effective but Not Without Risks
Radiation therapy is another conventional approach deployed against Uterine Leiomyosarcoma. While it plays a role in local control and symptom relief, radiation exhibits clear limitations in terms of side effects and long-term risks. Studies in Hong Kong Radiotherapy Journals (2024) emphasize how radiation-associated tissue damage extends beyond targeted cancer cells, injuring surrounding healthy tissues.
Patients often experience distressing side effects including:
- Skin burns and dermatitis, causing pain and discomfort.
- Severe gastrointestinal issues like diarrhea, bleeding, and chronic bowel disturbances.
- Chronic bladder irritation, urinary urgency, frequency, and reduced bladder function.
Furthermore, radiation therapy considerably heightens the risk for secondary malignancies. According to recent meta-analytical findings reported by JAMA Oncology (2023), the risk of developing secondary cancers after radiation therapy increases up to 300%. Such secondary malignancies significantly impact prognosis, complicating long-term management.
Surgical Treatment: A Vital Yet Risky Endeavor
Surgical intervention, particularly radical hysterectomy or cytoreductive surgery, remains vital in managing localized Uterine Sarcoma (Uterine Leiomyosarcoma). Nevertheless, surgery is subject to limitations, especially concerning operational risk and potential morbidity following the procedure.
- Postoperative infections occur in roughly 15–20% of cases, delaying subsequent treatments.
- Substantial surgical complications, including hemorrhage or urinary tract injury in 5–10% of operations.
- Lymphedema following lymph node dissection reduces quality of life through chronic swelling and reduced mobility.
Reports from the Hong Kong Surgical Society (2024) reveal that complexities in post-operative care pose significant emotional and physical burdens, particularly for older patients. This raises essential considerations for patient selection, management timelines, and comprehensive supportive care pathways.
Metabolic Resistance and Treatment Challenges
Beyond overt toxicity and limited efficacy, traditional therapies face profound limitations due to intricate metabolic resistance mechanisms. Uterine Leiomyosarcoma cells exhibit exceptional adaptation strategies, including upregulated glycolysis known as the Warburg effect and pronounced glutamine dependency, significantly impacting therapeutic effectiveness.
Recent research spearheaded by prominent Asian oncology experts such as Dr. Li Guohua and Prof. Liu Guolong highlights critical findings related to metabolic resilience. For instance, Uterine Sarcoma cancer cells demonstrate a 400% elevation in DNA repair enzyme activity upon exposure to DNA-damaging chemotherapy and radiation, rapidly repairing therapeutic damage and substantially reducing therapy effectiveness.
These enhanced metabolic and cellular repair capabilities effectively shield cancer cells from standard treatments, making therapeutic resistance a significant hurdle and fueling disease recurrence. This underscores an immediate need for innovative therapies that target these metabolic vulnerabilities rather than traditional approaches alone.
The Urgency for Innovative Treatment Approaches in Asia
The medical community in Hong Kong and across Asia widely acknowledges the pressing limitations presented by traditional treatments in managing Uterine Sarcoma (Uterine Leiomyosarcoma). Patients navigating conventional approaches face physically debilitating side effects, limited therapeutic outcomes, and an unaddressed underlying metabolic resistance.
Recognizing these serious limitations, leading institutions like Shenzhen Qianhai Taikang and partners such as MD Anderson have intensified their commitment to pioneering innovative therapies. Groundbreaking metabolic therapies under development, guided by Nobel-laureate research (e.g., Allison, Semenza), offer promising alternatives aimed at metabolic vulnerabilities, drastically improving patient outcomes.
Such innovative therapeutic frameworks not only propose reducing treatment-related toxicities but also aim to transform cancer management into achievable chronic control. For patient communities in Hong Kong, Asia, and globally, this represents a significant leap forward.
Ultimately, the considerable shortcomings of chemotherapy, radiation, and surgical approaches underline a critical need to complement traditional therapies with innovative metabolically targeted solutions. This integration holds the potential to improve patient outcomes, reduce treatment burdens, and enhance overall quality of life, aligning harmoniously with AllCancer’s 2025 strategic goal to render key cancers manageable chronic diseases.